Cervical Degenerative Disc Disease
Table of Contents
What is a Cervical Degenerative Disc disease?
Cervical degenerative disc disease is a condition in which gradual degeneration of the intervertebral disc due to age-related wear and tear which causes Neck pain with or without radiating arm pain.
Degenerative disc disease of the cervical spine usually develops in aging people uniformly in terms of patient gender. Patients commonly present with pain. Pain, or in combination with added neurological clinical presentation, may need surgical intervention. Treatment options range from nonoperative measures to decompression, instrumented fusion, laminoplasty or instrumentation, or a combination of both. This chapter will examine the anatomy, natural history, cause, pathophysiology, evaluation, and management options.
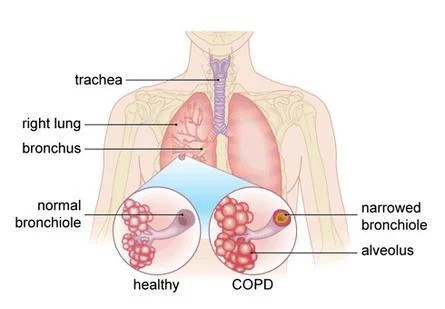
The cervical spine, C1 to C7, gives exceptional function and range of movement. The higher cervical spine, C1 (the atlas, which articulates with the occiput), and C2 (the axis) are extremely specialized, allowing for major ranges of movement (rotation, flexion, extension, and side-bending) associated with facet orientation allowing for extra rotation. Structures nearby to the cervical vertebrae consist of the spinal cord and nerve roots, blood vessels as well as the trachea and esophagus.
The intervertebral disc (IVD) is created from the C2-C3 level down, helping in cervical spine mobility and stabilization. In comparison to the thoracic and lumbar vertebrae, the cervical vertebrae have a distinctive bony prominence known as the uncinate process, which articulates with the neighboring level to form the joint of Luschka or uncovertebral joint. It helps to reinforce the intervertebral disc (IVD) and provides additional stability and motion. The IVD is an intricate structure composed mainly of two parts, the peripherally situated annulus fibrosus (AF) and the centrally located nucleus pulpous (NP) responsible for its’ load distribution purpose. The anterior and posterior longitudinal ligaments were again strengthened by the IVD.
The AF of the intervertebral discs is typical of type I collagen in layers (lamellae), proteoglycans, glycoproteins, elastic fibers, and extracellular matrix (ECM) secreting cells. These collagen layers are exclusively positioned to form a physically powerful shell for the inner contents, the NP.
The NP has a gel-like consistency composed mostly of water, which decreases with age (~90% at delivery and 70% by age 60). The residual minority of the NP contents then contains type II collagen and proteoglycans. An important proteoglycan in the NP is aggrecan, which, when bound to hyaluronic acid, aids to keep water within the NP, allowing for load resistance.
Following the first years of life, the IVD becomes the major avascular structure within the body. Most of the nutrition delivery is via metabolite circulation from the vertebral endplates. after a while, the IVD not only begins to lose its water content but its proteoglycan supply as well, resulting in an additional fibrotic consistency of the NP and subsequent fissuring As those vertebral endplates calcify according to the aging. There are diverse types of NP herniations. If the NP herniates but remnants contained by the annulus, it is called a disc protrusion. still, the NP can also go through injured annular fibers, and NP contents can extrude through a desert in the annulus, referred to as a disc extrusion. in addition, NP fragments can be divided from the extruded disc material, yielding disc sequestration.
The degenerative process of the cervical spine is into three separate stages:
- Dysfunction
- Instability
- Stabilization.
- Dysfunction happens between the ages of 15 to 45 years old. through this stage, radial and circumferential tears can occur in the annulus accompanied by the facet joint localized synovitis.
- Instability can happen in persons between the ages of 35 to 70 years old. This stage is characterized by disturbance of the inner disc with progressive restoration, as well as facet joint degeneration. This condition results in the last stage of the process,
- Stabilization happens after 60 years of age. Here, hypertrophic bone develops nearby the facet joints in addition to the disc, promoting a rigid and possible ankylosing spine. entertainingly, every spine segment may be at a dissimilar degenerative stage. One level can be completing the dysfunction stage while another begins the stabilization phase.
Disc herniations emerge to occur as a result of the dysfunction and instability phase while spinal stenosis occurs as a result of the late instability stage and before the time stabilization stage as a lead to the bony overgrowth and disk space narrowing It is, for this reason, one can find a patient whose cervical spine segments have a combination of disc herniations and cervical spinal stenosis. C5-6 is most usually affected because of the biomechanics of the cervical spine.
When discussing the natural history of cervical degenerative disc disease and management options, symptomatic patients be capable of suffering an array of clinical presentations from pain intermittent or continuous, with a potential neurological clinical presentation with no pain. Patients usually receive nonoperative management when experiencing nonprogressive pain and/or minimal neurological issues.
If surgery is crucial, it is classically elective, and it is able to be delayed with the hope of symptomatic improvement. though, an exception is patients diagnosed with cervical myelopathy who must have more urgent surgical management to avoid progression.
The proper diagnosis and management for degenerative cervical myelopathy be able to be very challenging, particularly in patients with or still without ongoing axial neck pain with potential radiculopathy.
One must also be aware that 20% of patients with cervical stenosis might also have lumbar stenosis. While a lot of patients can have straightforward diagnoses with a thorough history and physical assessment accompanied by positive imaging modalities, there is an important subset of patients who have pain with no experiencing neurological findings (away from possible sensory changes) and whose imaging may not easily associate with physical exam findings.
For example in which other diagnostic modalities must hold a watchful history and physical assessment for an exact diagnosis. Thus, a systematic assessment is imperative to diagnose and treat these patients properly and effectively.“
Epidemiology
Related to the lumbar spine, cervical disc deterioration is an in nature occurring age-related phenomenon. The occurrence of cervical DDD enhanced with age in spite of the patient’s symptomatology. Literature has confirmed that in select residents, a quarter of patients below the age of 40 showed proof of disk degeneration or reduction at one level.
This proof was found in about 60% of patients in the same population who were more than 40 years old. Lehto et al. confirmed a parallel conclusion in asymptomatic patients older than age 40, in which 62% showed abnormalities on MRI.
In a Japanese study classify 497 asymptomatic individuals, Matsumoto et al. showed almost 90% of patients (Male and female) over 60 years of age had irregular findings as 17% and 12% of males and females correspondingly, in their 20s confirmed abnormalities. More than a few studies have acknowledged the main disc level involved in degeneration was C5-6, and the second most common being C6-7. Research has also confirmed that cervical DDD was related to lumbar degenerative changes in both males and females but did appear afterward in life. An association has also been initiated in the pain distribution in the neck-shoulder-brachial area in patients with modest to severe cervical DDD.
Evidence of degenerative change is usually present in most asymptomatic adults, with evidence of little disc degeneration in:
- 25% of adults below the age of 40
- 50% of adults above the age of 40, and
- 85% of adults above the age of 60
- Asymptomatic adults display revealing degenerative changes at one or more levels
- 70% of females and 95% of males between ages 65 and 60 were affected
- The highly common evidence of degeneration is present at the C5-C6 followed by C6-7 and Then C4-5.
Pathophysiology
- The pathophysiology of cervical spine degenerative disc disease is similar to the thoracic and lumbar spine. classically, physiologic changes happen inside the nucleus pulposus first, followed by progressive degeneration of the annulus.
- This usual degenerative process can result in the extrusion of the nucleus content. The segments start to become hypermobile resulting in additional degenerative arthritic changes and instability.
- Unlike the lumbar spine, these hypertrophic changes mostly happen at the uncinate process, which forms the ventral wall of the foramen (uncovertebral joint). The facet joints and vertebral bodies also ultimately begin to experience these hypertrophic changes because of altered load. As aforementioned, these changes result in stiffness and a reduction in motion of the cervical spine.
- Once an HNP happens, pain, which is the most frequent finding in CDD, is dependent upon the level affected and the location of the herniation. on the other hand, HNPs can also be asymptomatic.
- Most herniations happen posterolaterally given the AF’s thinner and weaker structure in this region because the PLL (posterior longitudinal ligament does not cover this region as thickly. Given the posterolateral place of the nerve root, the HNP can produce pain in two ways; one is if the dorsal root ganglion (DRG) becomes compressed, the presenting symptoms will classically follow a dermatomal pattern.
- On the other hand, if the HNP is directly posterior, the second way is that spinal cord compression can happen, with symptoms distal to the injury.
Risk factors
- Age, sex, and occupation.
- The incidence of cervical degeneration is equal in both gender, although the degree of severity is larger in men.
- Repeated occupational injury may be prone to the development of cervical degeneration. enhanced incidence in individuals who lift and carried heavy weights on their heads or shoulders and in dancers and gymnasts.
- In about 10% of individuals, cervical degeneration is because of congenital bony anomalies, blocked vertebrae, and malformed laminae that place undue stress on above and below intervertebral discs.
Causes
- As IVD is reliant on intervertebral endplate distribution for nutrition, cervical degeneration is an ordinary part of aging, which starts previous to time on the second decade of life. Since the discs lose water content, they can become not as much of obedient and fissure resulting in a decline in disk height and disintegration.
- This variation in alignment is able to further put pressure on the posterior aspect of the cervical spine and end result in spondylotic changes as well (that is., facet hypertrophy).
- The less hydrated NP, as it degenerates, the load of the cervical spine and the enlarged forces exerted on the NP are then as well transmitted to the AF, which then begins to obliterate and fissure, weakening the AF. This further causes the IVD to fall in height, as the AF begins to bulge and increase in diameter and then fissure.
- At the same time as aging, some environmental and hereditary factors can dispose persons to the development of cervical degenerative disc disease.
- Of interest, with enhanced use of electronics (for instance handheld devices for instance smartphones) during sitting, chronic flexion at the neck can lead to enlarged stress on the discs. In the neutral position, the head weight is around 12 lbs (5.4 kg). With increased flexion, the relative weight seen on the discs increases to 27 lbs (12.2 kg) at 15 degrees, 18.1 kg at 30 degrees, 22.2 kg at 45 degrees, and 27.2 kg at 60 degrees of flexion. This chronically added load yields extra chronic stress on the IVD, mostly the NP, poor distribution, and nutrition to the IVD and subsequent deterioration.
- Other potential risk factors and causes have been objects of research, including smoking, occupation, genetics, atherosclerosis, contact sports, and earlier surgeries. Though, studies have initiated contradictory proof demonstrating unsure help of body mass index, gender, sports, smoking, and alcohol consumption. Gore et al. showed no proof suggesting cigarette smoking is a contributing agent in cervical spine degeneration. Sports for example weightlifting were also not initiated to enhance the risk of deterioration.
History and Physical
- A cautious history is paramount to make sure that existing symptoms are caused by degenerative changes and not more severe conditions. conversation with the patient regarding potential constitutional symptoms (weight loss, fever, chills, or sweats) and infections can be vital, along with oncologic history and injury. If pain is an existing symptom, a thorough pain history for example functional limitation, intensity, onset, alleviating and exacerbating symptoms, radiation, and associated symptoms is required. A complete history of neurologic complaints for example weakness, sensory loss, and gait is very important.
- The physical exam must always start with the patient’s vitals (i.e., fever). A thorough neurologic examination is essential, which at a minimum must consist of motor testing of the upper and lower extremities, cranial nerve testing, gait, and balance evaluation, sensation, and reflexes (involving Hofmann’s and Babinski), and any clonus. The range of motion of the cervical spine must undergo assessment for both degrees of movement and elicit any symptoms.
- Most usually, patients present with axial neck pain and difficulty with movement. A little subset of patients might complain of headaches, while others tend to experience shoulder pain. Unilateral radicular symptoms are also quite prevalent and most usually cause by posterolateral disc herniations and osteophytes located at the neural foramen.
- Other clinical presentations comprise changes in deep tendon reflexes, muscle atrophy, hypesthesias, paresthesias, or weakness demonstrated by definite nerve root signs. A significant proportion of flexion/extension motion of the cervical spine happens between C4-C6. fascinatingly, the study shows that the C5-C6 interspace has the initial and most significant amount of degeneration. The most frequent nerve roots affected by a disk protrusion are C6 and C7. C6 is between C5-C6.
- Provocative testing for example a Spurling test and a shoulder abduction (relief) test can assess for any radicular symptoms. A Lhermitte’s sign is able to also assist diagnose potential cervical myelopathy. Evaluation of the paraspinal muscles for spasms and trigger points is necessary. An evaluation of the upper extremity would also be helpful, to assist in further differentiating existing symptoms. for instance, a patient may be complaining of a vague numbness and tingling in the hand, which may be secondary to carpal tunnel syndrome, double crush syndrome, or cervical radiculopathy.
- Cervical disc disease can be asymptomatic and degenerative changes only start on imaging for example CT scan, X-rays, or MRI. A posterolateral symptomatic HNP will exist with dermatomal pain, myotomal weakness, or sensory change. The most frequent HNP is at C6-7, just anterior to the C7 nerve root. When the C7 nerve root is inflamed or compressed, the patient will complain of pain from In the region of the neck radiating to the lateral forearm and then palm and possibly radiation to the middle finger. Muscle weakness may exist in the ipsilateral triceps muscle, making extension at the elbow hard. The triceps reflex may also be depressed and irregular.
- C5 root compression can exist with neck pain radiating to the shoulder along with peri-scapula pain. The deltoid may be affected, and weakness during shoulder abduction, external rotation, and elbow flexion can happen. The biceps and brachioradialis reflex can also be depressed and irregular.
- When the C6 nerve is impaired, neck pain will radiate to the region of the neck, shoulder, and down to the thumb, and index digits, in addition to periscapular pain. This nerve root innervates the biceps along with the wrist extenders, and weakness through elbow flexion and wrist extension may exist. The biceps and brachioradialis reflex may also be depressed and irregular.
- The C8 nerve root gives a sensation from the region of the neck to the medial forearm and medial hand. The muscle groups innervated are the finger extensors, and weakness through the thumb extension can happen.
- Similar to the C8 nerve root, the T1 nerve root, when involved, will present with pain in the neck radiating to the medial arm and forearm but will hardly ever go to the hand. First dorsal interosseous muscle weakness might be present.
- Extreme cervical spondylosis, ossification of the posterior longitudinal ligament, disc herniation, or any combination of these can reason to cervical spondylotic myelopathy. This condition most usually takes place in patients in their 50s or afterward. The signs and symptoms are broadly variable and rare, describing their legs as feeling stiff and/or wooden. a little can complain of numbness and tingling originating from the fingertips to the hands as if they were wearing gloves). Writing and other fine motor functions (dexterity) can also become altered. Hyperreflexia, a positive Hoffman sign, ankle clonus, and a Babinski reflex may also be there. Gait disturbances can take place. In extreme cases, bladder and bowel changes can occur.
Differential Diagnosis
- Brachial plexopathy
- Carpal/cubital tunnel syndrome
- Peripheral neuropathy or neuritis
- Complex regional pain syndrome
- Demyelinating disorder
- Radiation plexopathy
- Malignancy (Pancoast tumor for neuropathic symptoms)
- Myofascial pain
- Cervical spondylosis
- Sprained ligaments
- Cervical sprain and strain
- Rheumatologic disorders– such as Fibromyalgia
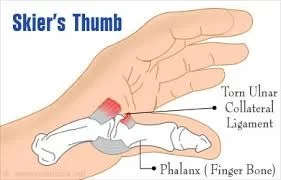
- Shoulder pathology/rotator cuff injury
- Thoracic outlet syndrome
- Infectious etiology/osteodiscitis
- Other non-specific neck pain lesions – such as acute neck strain, postural neck ache, or Whiplash, Fibromyalgia, and psychogenic neck pain
- Mechanical lesions – such as disc prolapse or diffuse idiopathic skeletal hyperostosis
- Inflammatory diseases – such as Rheumatoid arthritis, Ankylosing spondylitis, or Polymyalgia rheumatica
- Metabolic diseases – such as Paget’s disease, osteoporosis, gout or pseudo-gout, Infections – osteomyelitis or tuberculosis
- Malignancy – such as primary tumors, secondary deposits, or myeloma
Prognosis
- The prognosis and disease development are hard to predict and very uneven from patient to patient. In a study establish in 1956, Clark and associates followed 120 patients with cervical degenerative. They establish that in 75% of patients, the disease process weakened in an episodic manner, in 20% of patients, symptoms steadily progressed, and in 5%, patients became symptomatic quickly.
- Several years later, Lees et al. further established the randomness of the disease. In his study of thirty-seven patients, Nurick et al. establish that there was an early phase of deterioration, then a nonprogressive phase which, in a few cases, lasted for years.
- Older patients were more prone to additional deterioration. In another study, 26% of patients’ conditions worsened, 38% remained stable, and over one-third were better.
Diagnostic Procedures
Cervical degenerative is frequently diagnosed with clinical signs and symptoms only.
Signs:
- Unfocalized tenderness
- Lose of range motion
- minor neurological changes (unless complicated by myelopathy or radiculopathy)
Symptoms:
- Cervical pain aggravated by the movement
- Referred pain (occiput part, between the shoulder blades and upper limbs)
- Retro-orbital or temporal pain
- Stiffness of Cervical
- Vague numbness, tingling sensation, or weakness in upper limbs
- Dizziness or vertigo
- Poor balance and coordination
- Rarely, syncope triggers migraine
- Many patients do not require further investigation and the diagnosis is made on clinical grounds alone however, diagnostic imaging for example X-ray, CT, MRI, and EMG can be used to confirm a diagnosis.
- Plain radiographs of the cervical spine might indicate a loss of normal cervical lordosis, indicating muscle spasm, but frequently other features of degenerative disease are present in asymptomatic people and correlate poorly with clinical symptoms.
- It is necessary to realize that radiological changes with age alone represent structural changes in the vertebrae, but such changes do not necessarily cause symptoms.
- It is believed that this mismatch between radiographic appearance and clinical symptoms is not only due to age but also due to sex, race, ethnic group, height, and work.
- MRI of the cervical spine is the first choice for investigation if more serious pathology is suspected, as it provides detailed information about the spinal cord, bones, discs, and soft tissue structures.
- However, normal people can show important pathological abnormalities on imaging so scans require to be interpreted with proper care.
Complications of Cervical Degenerative Disc disease
Patients with cervical disc disease can experience a considerable impact from pain and disability, frequently not correlated to the level of pathologic changes in the discs themselves. This disability is able to yield loss of productive days at work, worsening of roles in personal life along with overall poor health from being more inactive in their lifestyle.
Neurologic complications are able to take place as outlined above with loss of lower extremity function and incontinence being a very catastrophic, albeit rare, impediment with myelopathy.
Evaluation
- Laboratory testing can assist in diagnosis, particularly if an infection (that is Lyme disease), autoimmune arthritis, or a metabolic disorder (folate or vitamin B12 deficiency) is high on the differential diagnosis. A CBC with differential along with an ESR and CRP are also essential; though, all lack specificity for spinal infection. Blood cultures can also be indicated when an infection is supposed.
- Imaging must start with a radiographic assessment, which can indicate a decrease in normal cervical lordosis, hypertrophic changes, and disc space narrowing. They are also useful in ruling out additional problems like fractures or instability. Computed tomography (CT) may also be useful for preoperative planning, mainly in patients with dorsal osteophytes and OPLL.
- MRI is the gold standard for patients when in view of degeneration of the cervical spine as a latent diagnosis as ligaments, disc, and neural structures are visible. Magnetic resonance (MR) imaging allows for the evaluation of both soft tissue and boney structures and precisely measures functionally relevant spinal canal and spinal cord dimensions in a variety of planes.
- Reduced spinal canal width enhanced the risk of cervical cord compression and myelopathy. Because space around the cord becomes relatively reduced in the lower cervical spine segments, the risk peaks at these levels. On MRI, the inner disk spaces tend to have a fairly high signal intensity, and the nearby rim, the annulus fibrosus, is of low signal intensity.
- A region of medium-intensity dorsal demonstrates central or paracentral disc herniations to the disk space. Myelopathic patients can not originally be there with cord changes but may be present with time. These changes are demonstrated by hyperintensity at the level of cord compression with cord edema or even myelomalacia.
- It is also vital to note further modalities to help in ruling out other potential diagnoses. For instance, EMG can be helpful to eliminate compressive and/or peripheral neuropathies caused by occupational exposures, diabetes, or folate/vitamin B12 deficiencies.
Treatment of Cervical Degenerative Disc Disease
Medical Management
- The management strategy for cervical degeneration depends upon the severity of the signs and symptoms of a patient.
- In the absence of “red flag” symptoms or significant myelopathy, the aim of treatment is to minimize the pain, improve functional ability in ADL activities, and prevent permanent trauma to neural structures.
- Symptomatic cervical spondylosis must be approached in a stepwise fashion, starting with non-operative management.
Non-surgical
- Conservative modalities comprise rest, modification of activity, pharmacological agents, physical therapy, manipulation, diverse types of injections, and acupuncture. early short-term immobilization can be useful. Medications may offer symptomatic relief. These may contain nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, or muscle relaxants. NSAIDs are usually used and give relief by the use of interfering with prostaglandin synthesis resulting in the inhibition of the inflammatory cascade.
- Steroids can be helpful in early management for short-term usage as they are related to deleterious side effects. Muscle relaxants are an option when patients are experiencing muscle spasms. Gross et al. established cervical mobilization and manipulation might give immediate or short-term relief for neck pain. GABA-class drugs similar to gabapentin and serotonin uptake inhibitors can be considered as well. Tricyclic antidepressants may also play a vital role. Clinicians must keep away from using opioids.
- A cervical collar may be suggested in patients who present with intractable neck pain. the argument exists over the efficacy of cervical traction for the treatment of HNP as there is no confirmation to recommend a reduction in the degree of disc herniation. It, though, may allow for some neuro foraminal decompression.
- Physical therapy is supposed to start early in the treatment algorithm. Passive modalities must be used and comprise but are not limited to heat, mechanical traction, massage, and a soft cervical collar. Heat has been shown to decrease pain and reduce muscle spasms. Confirmation suggests cryotherapy can aid reduce inflammation and reduce muscle guarding. Massaging the region of intensity allows for mechanical stimulation leading to an increase in circulation and the promotion of muscle relaxation. Cervical traction can allow for joint distraction and potentially relieve pressure off nerve roots/disks; this may get better epidural blood flow in the region and decrease pain, inflammation, and spasms.
- Active modalities are supposed to also be part of rehabilitation. These comprise aerobic conditioning, dynamic muscle training, isometric, and range of motion exercises. Postural training may help. Isometric exercises allow for the strengthening of paravertebral muscles with the prevention of certain motions that can cause pain. Recent reports suggest there was no tough confirmation for patients with chronic neck pain to undergo neck strengthening and stretching exercises.
- As confirmed previously, the diagnosis and treatment of cervical myelopathy may be tricky and random. Some patients may develop a sudden onset and turn down of symptoms while some may experience a plateau in symptoms, but in general, it is usually progressive as a timeline may be variable. Regrettably, spontaneous improvement hardly ever takes place. Sometimes, close observation may be a consideration in patients with symptoms that appear not to be progressing and are mild.
Surgery
- Patients who be unsuccessful to respond to nonoperative treatment, particularly those experiencing stubborn pain, progressive or considerable neurological compromise, or myelopathy can need surgical intervention.
- One surgical option is decompression. Decompression procedures may comprise fusion with or without instrumentation. on the other hand, classically most decompressions will consist of a fusion to minimize the potential for post-surgical deformity.
- Pain management procedures can also be helpful. Nerve root injections or epidural steroid injections be able to not only used as a diagnostic tool but can also be therapeutic. though, they are not without undesirable complications. In the past, trigger point injection has also been used, but no confirmation has shown its long-term effectiveness.
- There are a diversity of surgical approaches to the cervical spine. usually, the neural structures become compressed anteriorly; consequently, an anterior approach is essential to remove a disk, resulting in decompression directly and will most likely comprise a fusion (ACDF). The approach of choice in patients with normal to a kyphotic position is the anterior approach as a laminectomy in these patients can further cause kyphosis secondary to the destabilization that happens.
- During an ACDF, compressive and degenerative structures are removed with a fusion across the segments neighboring to the decompression. Furthermore, some disks can be removed with multi-level fusions (with or without strut graft).
- A corpectomy with strut grafting can be essential for multi-level decompressions. An anterior cervical plate is able to be inserted to add to stability and earlier mobilization. Distraction across the disk space with an interbody implant can result in further indirect decompression of the neural foramen.
- A few studies reveal a fusion rate of up to 94% following an ACDF. though, for fusion to be successful, appropriate patient selection and exact operative techniques are key. The present literature shows support for the major symptomatic improvement of most patients. Even though recurrent clinical presentation, evening worsening, can still happen most likely secondary to nearby level degeneration to the fusion. Furthermore, neurological compromise is rare (0.01%).
- Other possible complications comprise soft tissue dissection when using the anterior approach followed by grafting and plating. During dissection, the recurrent laryngeal nerve is able to suffer injury, causing a palsy, potentially leading to hoarseness.
- Additionally, the esophagus or trachea can be injured, and possibly perforated, and the graft can become dislodged and subside. Hoarseness and/or dysphasia can be noted postoperatively, particularly with higher levels operated on or with multi-level cases.
- When an indirect decompression is warranted, the posterior approach to the spinal cord is able to be utilized. This approach is mainly for patients with neutral or lordotic cervical spine alignment. in addition, the posterior approach is fairly useful with patients who have multi-level compression and congenital stenosis, typically involving C3-C6 or C7.
- The muscles attaching to the 2nd cervical segment are protected to prevent progressive kyphosis and postoperative neck pain. Posterior decompression provides the spinal cord with extra space, moving away from the disk/bony ridges and compressing anteriorly. Options comprise laminectomy (either with or without fusion) or open-door laminoplasty. Both of these can achieve a similar goal, to increase the diameter of the canal.
- Highsmith et al. showed the same neurological outcomes between the two, but patients who underwent a laminectomy with fusion had less neck pain compared to laminoplasty. If neck pain is there, fusion must be done to address this as just doing a decompression may allow for neurological recovery but not alter pain from DDD.
- Laminoplasty is frequently reserved for patients with cord compression without or with minimal neck pain. Laminoplasty can minimize the potential risk of postoperative kyphosis in patients with neutral to lordotic spine. Presently, laminectomies are typically accompanied by instrumented fusion, which increases stability and is able to maintain or restore lordosis. Lees et al. demonstrated satisfactory results in 70 to 80% of patients who underwent a laminectomy.
- Hirabayashi et al. described the expansive open-door laminoplasty, which has shown good results in 66% of patients. though, These techniques are not without their complications, which range from hematoma, dural injury, paralysis, postoperative C5 palsy, postlaminectomy kyphosis, and neck pain. furthermore, a foraminotomy is an option for direct decompression of nerve roots in patients with only radiculopathy.
- In recent times, cervical disk arthroplasty has gained popularity.
- A few studies show no significant difference between fusion and arthroplasty regarding revision rates two years postoperatively. Though, this procedure is not indicated for degenerative disc disease but rather for herniated discs.
- A mutual approach (anterior and posterior) may be required when a multi-level corpectomy is indicated or when there is diminished bone quality secondary to the patient’s metabolic state.
Physical Therapy Treatment

- There is little evidence of using exercise only or mobilization and or manipulations only.
- Mobilization and or manipulations in combination with exercises are effective for pain minimization and improvement in activity of daily living (ADL) in sub-acute or chronic mechanical neck pain with or without the headache.
- There is moderate evidence that different exercise regimens, for example proprioceptive, strengthening, endurance, or coordination exercises are more effective than common pharmaceutical care.
- Treatment must be individualized, but generally involved rehabilitation exercises, proprioceptive re-education, manual therapy, and postural education and guidance
- In 2018 study contrasting isometric exercises with dynamic exercises, both with traditional physiotherapeutic ways concluded that short-term physiotherapy plays a vital role in the management of cervical degeneration.
- The contrast between the two treatment techniques gives priority to dynamic exercises, compared to isometric exercises
- In 2001 meta-analysis done by the Philadelphia Panel were finding
- Physical modalities for example cervical traction, heating and cryotherapy, therapeutic ultrasound, massage, and transcutaneous electrical nerve stimulator (TENS) required adequate evidence regarding their efficacy in the treatment of acute or chronic neck pain.
- For an individual suffering radicular pain, cervical traction may be incorporated to relieve the nerve root compression that developed with the foraminal stenosis.
- Trigger point injections can be used to treat myofascial trigger spots, which can clinically manifest in the region of neck, shoulder, and upper arm pain.
- Manual therapy is stated as high-velocity; low-amplitude thrust manipulation or non-thrust manipulation. Manual therapy of the thoracic spine can be used for minimized pain, improve function, to improving the range of motion, and address the thoracic hypomobility
- Thrust manipulation of the thoracic spine could involve techniques in a prone position, supine position, or sitting position based on the therapist’s choice. Also, cervical traction can be used as physical therapy to enlarge the neural foramen and shifting and minimized the stress of the neck
- Non-thrust manipulation consists of posterior-anterior (PA) glides in the prone position. The cervical spine techniques can consist of retractions, rotations, lateral glides in the ULTT1 position, and PA glides.
- The techniques are preferred based on the patient’s response and centralization or minimization of symptoms.
- Postural education involved the alignment of the spine during sitting and standing activities.
- Thermal therapy gives symptomatic relief only and ultrasound appears to be ineffective in this case.
- Soft tissue mobilization was given on the muscles of the upper quarter with the involved upper extremity positioned in the abduction and external rotation to pre-load the neural structures of the upper limb.
- Home Exercises consist of cervical retraction, cervical extension, strengthening of the deep cervical flexor, scapular strengthening, and stretching of the chest muscles via isometric contraction of the flexor o the extensor muscles to reinforce the mobility of the neural structures of the upper extremity.
- Education The natural history of cervical degeneration is extremely variable, as well as challenging to prevent, given that it is part of the normal aging process.
- The patient must receive training on ways to detect the early onset of cervical degeneration, which consists of maintaining good neck strength and flexibility, resulting in an active and healthy lifestyle, and preventing neck injuries (such as good ergonomics, preventing prolonged neck extension, proper equipment for contact sports, proper safe tackling technique, and use a seatbelt in automobiles while traveling).
FAQ
The reply is yes, even if it forces you to be out of occupation for an extended amount of period. Don’t give up. There are various alternatives to pain relief that you can perform at your home that can help you to live a routine life.
Degenerative disc disease is usually frequent in aging adults, and, as a reassurance, it seldom needs surgery. When medical attention is required, the majority of patients respond well to non-surgical forms of treatment, and recovery happens in about six weeks.
Cervical degenerative disease can’t be back—same as aging, no treatment can reverse nonetheless that process. However, exercise and stretching may relieve minimizing neck pain and strengthen the nearby neck structures (eg, muscles, and joints) to decrease the possibility of future disc problems.
The Four Stages of Degenerative Disc Disease
• Dysfunction Stage (Stage 1)
• Dehydration Stage (Stage 2)
• Stabilization Stage (Stage 3)
• Collapsing Stage (Stage 4)
If the diagnosis is a degenerative disease, your orthopedic surgeon will give you a treatment plan to improve function and minimize pain. For most people, at-home and minimally invasive treatments are adequate to control back pain.





One Comment