Ataxic Gait
Table of Contents
What is Ataxic Gait?
A common feature of ataxic gait is the inability to walk straight ahead, as well as lateral veering, poor balance, a wider base of support, irregular arm movements, and lack of repeatability. These signs frequently reflect the way a person walks after drinking.
During walking, there are some features of intralimb leg coordination problems that are caused by weaknesses in handling interaction torques (such as stepping over barriers).
The majority of the identified walking deficiencies, on the other hand, are strongly related to impairments in dynamic balance, or inefficiencies in the coordination of the trunk and the two legs to keep the body’s center of gravity over the feet. Numerous gait ataxia symptoms are not present in cerebellar individuals with relatively mild balance deficits but rather severe leg coordination impairments, according to research. However, cerebellar individuals with major balance abnormalities but just moderately impaired leg coordination exhibit virtually all the symptoms of gait ataxia.
What is Ataxia?
When you have ataxia, your muscles have trouble coordinating, resulting in awkward, ungainly, or sloppy motions. It can occur as a standalone condition or as a symptom of a variety of other disorders or situations. It may be possible to treat or reverse the symptoms of ataxia depending on the cause.
Types of ataxia
- Vestibular Ataxia: A issue with your inner ears, which are a component of your sense of balance, causes this sort of vertigo. You find it difficult to coordinate your movements when your sense of balance is off.
- Cerebellar Ataxia: This form of ataxia results from a problem with the cerebellum, a region of the brain that controls how various brain regions interact with one another.
- Sensory Ataxia: Your body possesses a “self-positioning” sense that your brain may use to keep track of where each body part is. How, for instance, do you know where your hands and feet are when you can’t see them (like when your eyes are closed or you’re in a dark room)? The sensation of your own place is disturbed by sensory ataxia.
What causes Ataxic Gait?
Abnormalities in the brain, spinal cord, and peripheral nervous system can lead to ataxic gait. Ataxic gait abnormalities have distinctive characteristics when brought on by cerebellar problems. The combination of dysmetria, dyssynergia, dysdiadochokinesia, dysrhythmia, and intention tremor is referred to as cerebellar ataxia
The cerebellum communicates with other parts of the brain to control fine motor action. The cerebellum has trouble integrating data from the brain and the rest of the body when cerebellar neurons are injured. As a result, it is challenging to coordinate balance, posture, and smooth muscle activity, which adversely affects gait function.
Signs and symptoms of Ataxic Gait
About 50% of patients experience gait ataxia. Vision loss, vertigo, tinnitus, alternating hemiparesis, and paresthesias of the fingers, toes, and corners of the mouth are additional symptoms. It is possible to experience a sudden loss of consciousness, which typically lasts only a few minutes. Rare but potentially fatal consequences include cardiac arrhythmia and brainstem stroke. Following the neurological abnormalities, a severe, throbbing occipital headache is typical. A little over one-third of instances involve vomiting and nausea.
Ataxia is frequently described as a lack of coordination in bodily motions or a loss of balance that is not brought on by muscular weakening. Ataxia symptoms can be observed in a range of voluntary motor activities, including using the hands or fingers, speaking, moving the eyes, eating, donning garments, and pacing (ataxic gait). Ataxia is a symptom of one or more underlying disorders that damage the neurological system; it is not a distinct disease in and of itself. Ataxia symptoms can be extremely obvious in a repeatable motor task like gait. Ataxia’s gait symptoms are significantly different from those of Parkinson’s disease, leg spasticity, or orthopedic issues.
Even though children may experience recurring basilar migraine attacks, over time the assaults develop into a pattern of classic headaches. The patient may still experience vertigo and ataxia even during occurrences of classic headaches.
Types of ataxic gait
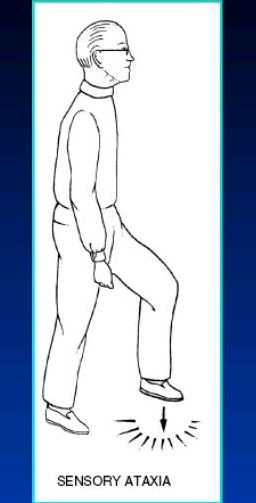
Sensory Gait: Although the cerebellum is unaffected in ataxic gait, its afferent fibers, or sensory stimuli, are altered.
Symptoms and Signs
Typically, the patient has lost sensory and proprioceptive stimulation in the lower limb.
They are not conscious of where their limbs are. They take steps that are more than required while walking, carefully watching the ground. To boost sensory input, only patients with sensory ataxia strike the ground.
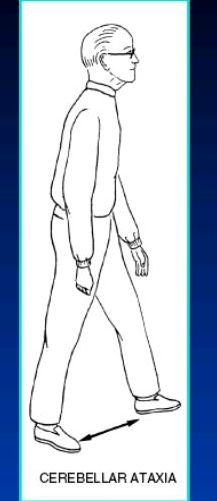
Cerebellar Gait: Due to a cerebellar lesion, this uneven and stumbling stride is directed in towards the lesion.
- Patients frequently look for something to lean on, such as a cane, a bed rail, or even the wall, because it frequently occurs by swaying to one side or the other.
- It loses balance when attempting to walk in tandem (heel-to-toe gait).
- Stance is also made wider, although this is insufficient to stop stumbling.
- When patients are instructed to close their feet and narrow their base, creating a fall, titubation (a fore-and-aft tremor of the head and trunk) while standing becomes noticeably worse.
- Open (or closing) the eyes thus has the opposite effect on posture (negative Romberg’s).
- Since it is linked to additional cerebellar deficiency symptoms such as dysmetria, dysarthria, nystagmus, hypotonia, and intention tremor, it varies from sensory ataxia.
Treatment of Ataxic Gait
Lying bent knee rotation

This exercise will help with bed mobility and transfers because it focuses on the segmental movement of the lower extremities. Legs should be level, hip distance apart, and both knees should be bent. The arms should be spread widely away from the body. Allow both knees to slowly start rotating from one side to the other. While your lower body pivots from side to side, make an effort to maintain a flat back and upper body. Ten repetitions of this exercise should be done gently and smoothly.
Quadriceps weight shifting
Weight Shifting on Four Legs This exercise will concentrate on developing kneeling-based core stability. This will make it easier to reach and balance unstable positions. Beginning in a neutral spine position, kneel with hands under shoulders and knees under hips. Slowly raise an arm to shoulder height before starting to stretch the leg on the other side backward to hip height. Before lowering your arm and leg to the ground, maintain your balance for a time. Repeat with the arm and leg on the other side. Keep your spine in a neutral position and move slowly and steadily throughout this exercise. Make an effort to finish 10 repetitions.
Sit to stand
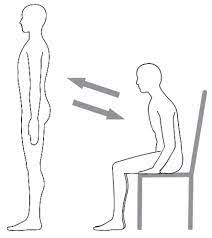
Stand-to-Sit This workout aims to improve balance and lower extremity strength during functional sit-to-stand. Place your feet under your knees while seated, about hip distance apart. Place your full body in the front of the chair and sit up straight. As your weight is transferred to your feet, push yourself up into a standing position by using the strength in your legs. Ten repetitions later, sit back down in the chair. Do this slowly and steadily, and avoid using your arms as support.
Weight shifting in sitting
Sitting Lateral Weight Shifts Instructions: Sit upright on an exercise ball (more difficult) with your feet under your knees and your hips spaced out. Slowly and smoothly start moving your upper body to the right before switching to the left. Allow your trunk’s weight to completely shift from side to side. Do 10 repetitions. This exercise focuses on core stability and balance.
Weight shifting in standing
lateral weight shifts while standing This balance-building practice serves as a warm-up for side-stepping and turning motions. Standing feet should be at least hip-width apart. Slowly start to lateralize your weight by shifting your hips, trunk, head, and shoulders onto one foot. Ten repetitions of this shifting motion from one side to the other are required.
Forward-backward weight shifting
Standing Anterior-Posterior Weight Shift is a balance exercise that prepares the body for walking. Place your feet hip-width apart or further apart when standing. Start slowly shifting your entire weight into your toes, then slowly back into your heels. Perform 10 repetitions of this shifting motion forward and backward.
Side-to-side weight shifting
lateral weight shifts while standing This balance-building practice serves as a warm-up for side-stepping and turning motions. Standing feet should be at least hip-width apart. Slowly start to lateralize your weight by shifting your hips, trunk, head, and shoulders onto one foot. Ten repetitions of this shifting motion from one side to the other are required.

One leg stand
Single Leg Stance Functionally related to walking and transfers (such as getting in and out of a bathtub, etc.), this exercise addresses balance with a small base of support. Start with standing up straight and distributing your weight onto one leg. Then, without letting the other leg touch the standing leg, lift it off the floor. Try to maintain your balance for longer periods of time while standing on one leg. Repeat on the other side, lowering the raised leg.
FAQ
Physiotherapy can enable enhanced participation by reducing activity restrictions and enhancing gait, balance, and trunk control in ataxia patients. Given their high frequency and the prevalence of injuries caused by falls, it is crucial to think about fall prevention in individuals with progressive ataxia.
Ataxia is a symptom that appears frequently. Ataxia is a condition that occurs less frequently and usually only in conjunction with specific hereditary disorders and diseases.
A set of neurological illnesses known as ataxia are characterized by motor behavior that appears disorganized. Patients with ataxia may exhibit abnormalities in activities requiring fine motor control, such as walking, speaking clearly, swallowing, writing, and reading.