ACHILLES TENDINITIS
Table of Contents
What is Achilles Tendinitis?
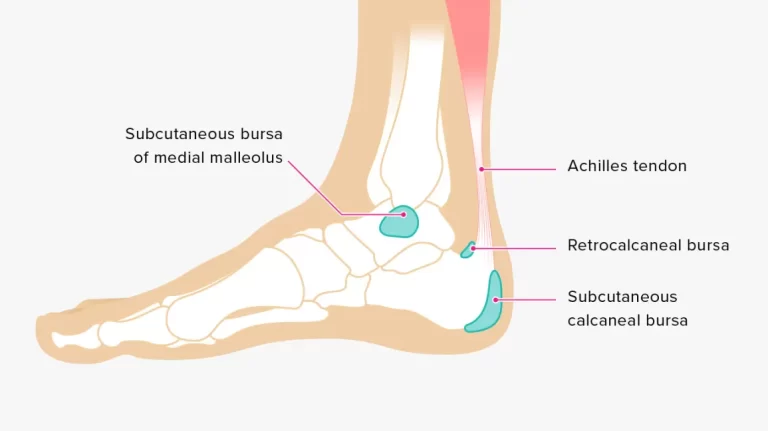
- The Achilles tendon joins the calf muscles to the heel bone or calcaneus and runs down the back of the lower leg. When this tendon is put under excess strain, it can become inflamed. This is Achilles tendinitis.
- this tendon use to jump, walk, run, and stand on the balls of your feet.
- Continuous, intense physical activity, such as running and jumping, can cause painful inflammation of the Achilles tendon, known as Achilles tendonitis (or tendinitis).
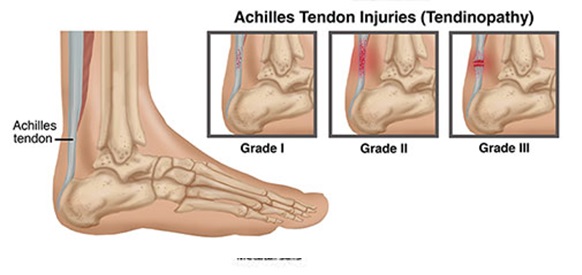
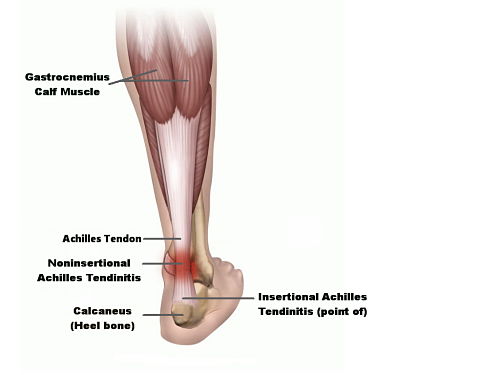
- There are two types of Achilles tendonitis: -insertional Achilles tendonitis -noninsertional Achilles tendonitis

- Insertional Achilles tendonitis: -affects the lower portion of your tendon where it attaches to your heel bone. -not necessarily related to the activity. It affects the lower portion of the tendon as it inserts into the heel bone.
- Non-insertional Achilles tendonitis: -involves fibers in the middle portion of the tendon and tends to affect younger people who are active. -more common in younger, more active people. The fibers in the middle of the tendon start to break down, thicken, and swell.
- Simple home treatments can help Achilles tendonitis.
- However, if home treatment doesn’t work, it’s important to see a doctor.
- If your tendonitis gets worse, your tendon can tear.
- You may need medication or surgery to ease the pain.
Causes of Achilles tendinitis:
- Excessive exercise or walking commonly causes Achilles tendonitis, especially for athletes.
- However, factors unrelated to exercise may also contribute to your risk such – Rheumatoid arthritis- infection is both linked to tendonitis.
- Any repeated activity that strains your Achilles tendon can potentially cause tendonitis. Some causes include: -exercising without a proper warmup. -straining the calf muscles during repeated exercise or physical activity. -playing sports, such as tennis, that require quick stops and changes of direction.
- A sudden increase in physical activity without allowing your body to adjust to increased training, for example, running speed or distance covered.
- wearing old or poorly fitting shoes -wearing high heels daily or for a prolonged duration
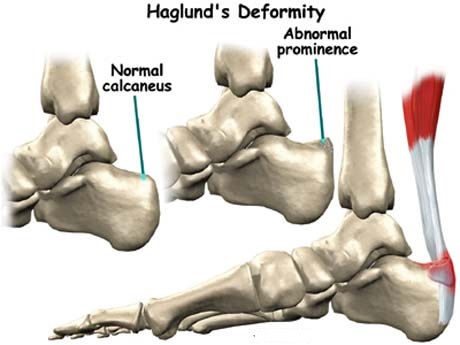
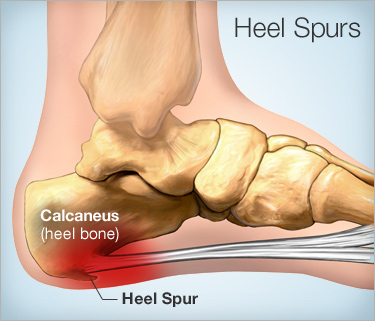
- having bone spurs in the back of your heel
- being older, as the Achilles tendon weakens with age
- Prematurely introducing hill running or stair climbing to an exercise routine
- Running on hard or uneven surfaces
- Differences in foot, leg, or ankle anatomy can also lead to Achilles tendinitis.
- Flat feet or fallen arches can put a strain on the tendon.
- Bone spurs are extra bone growths where the tendon joins the bone. These can rub against the Achilles tendon, causing damage and discomfort.
- Patients taking fluoroquinolone antibiotics may have a higher risk of tendinitis and tendon rupture.
Symptoms of Achilles tendonitis:
- The main symptom of Achilles tendonitis is discomfort pain and swelling in the backside of your heel when you walk or run.
- tight calf muscles.
- limited range of motion when flexing your foot.
- the skin on your heel is overly warm to the touch.
- The Achilles tendon feels sore a few centimeters above where it meets the heel bone.
- The lower leg feels stiff, slow, or weak.
- A slight pain appears in the back of the leg after running or exercising and becomes more severe.
- Pain is greater when running fast, for a long time, or when climbing stairs.
- The Achilles tendon swells or forms a bump.
- The Achilles tendon creaks when touched or moved.
Diagnosing in Achilles tendonitis:
- To diagnose Achilles tendonitis, your doctor will ask you a few questions about the pain and swelling in your heel or calf.
- Your doctor may ask you to stand on the balls of your feet while they observe your range of motion and flexibility.
- The doctor also feels around, or palpates, the area directly to pinpoint where the pain and swelling are most severe.
- Some prime elements of the physical examination include inspecting and palpating (pressing on) the area around the Achilles tendon for swelling, warmth, crepitus (popping sensation), and tenderness
- all of these features may be present with acute Achilles tendonitis. With Achilles tendonosis, besides tendon pain with palpation, the tendon may feel thick or there may be small bumps along the tendon, signifying areas of scar tissue and fibrosis.
- A doctor can sometimes diagnose an Achilles tendon rupture by palpating the tendon.
- Another physical exam clue for an Achilles tendon rupture is bruising over the tendon, especially if the blood tracks beneath the malleolus (the bone that projects out on each ankle).
Thompson Test :
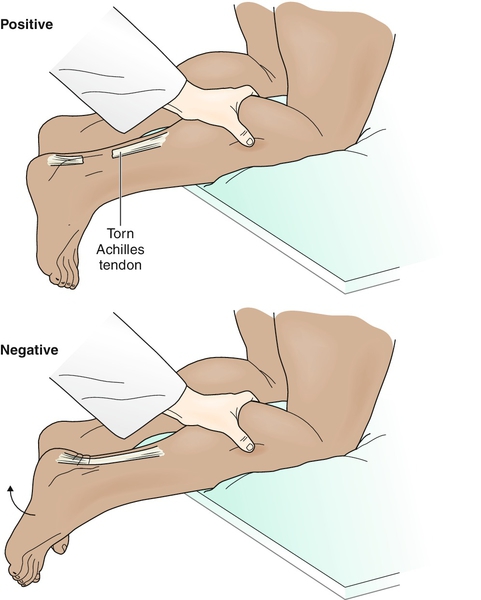
- also called the calf squeeze test.
- During this test, a person lies flat on the exam table with his or her feet hanging over the edge.
- The doctor will then squeeze on the calf muscle, which should flex the toes downward (called plantar flexion).
- If this does not occur, the test is positive for an Achilles tendon ruptur.
Differential Diagnoses in Achilles Tendinitis:
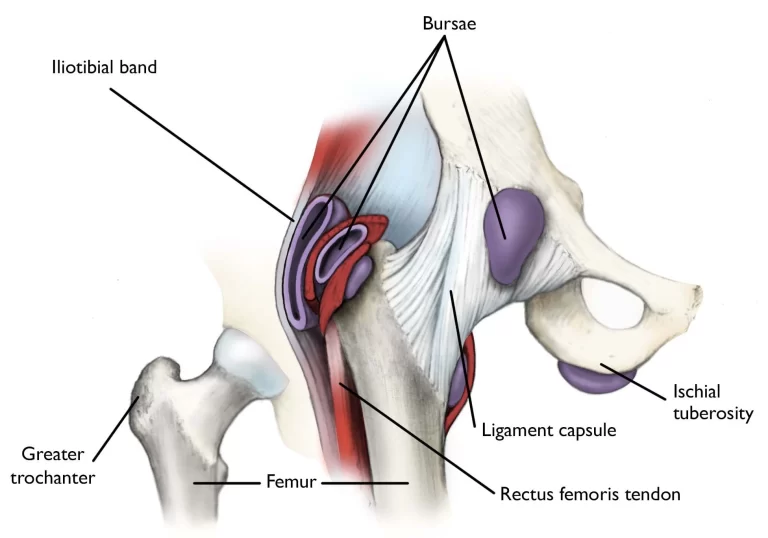
- When you see your doctor for Achilles tendon pain, your doctor will consider several other conditions. Some of the more common conditions include an ankle sprain, stress fracture, or heel bursitis (called calcaneal bursitis).
- Bruising around the Achilles tendon may be seen with an ankle sprain or a stress fracture, as well as an Achilles tendon rupture, so an X-ray is needed to distinguish among these conditions.
- With calcaneal bursitis, there is usually palpable tenderness where the tendon inserts into the heel bone. On the other hand, with Achilles tendonitis, the tendon pain is usually higher up— about two to six centimeters above the insertion site.
Other conditions that may be considered include:
- Osteoarthritis
- Inflammatory arthritis (for example, rheumatoid arthritis or gout)
- Fibromyalgia
- Blood clot in the calf (called deep venous thrombosis)
- Infection (for example, osteomyelitis or cellulitis)
- Bone cyst or cancer (rare)
- In these above instances, along with a thorough physical exam, blood tests or imaging tests, like an ultrasound or X-ray, may be used to confirm a diagnosis.

- For example, a Doppler ultrasound can rule out a blood clot in the calf, and an X-ray can reveal classic osteoarthritis changes in the ankle.
- Likewise, with rheumatoid arthritis, a person will usually have an elevated anti-cyclic citrullinated peptide (anti-CCP) blood level, along with other symptoms of RA like fatigue and joint pain.
- If a doctor is worried about an infection in the heel bone or in the skin near the tendon, identification of inflammatory markers (for example, erythrocyte sedimentation rate) and/or an elevated white blood cell count is helpful.
Treatment Achilles tendonitis:
- Many treatments are available for Achilles tendonitis, ranging from home remedies, like rest and anti-inflammatory medication to more invasive treatments, like steroid injections, platelet-rich plasma (PRP) injections, and surgery.
Your doctor might suggest:
- reducing your physical activity ( Rest )
- very gently stretching and later strengthening your calf muscles
- switching to a different, less strenuous sport
- icing the area after exercise or when in pain
- elevating your foot to decrease any swelling
- wearing a brace or walking boot to prevent heel movement
- going to physical therapy
- taking anti-inflammatory medication, such as aspirin (Bufferin) or ibuprofen (Advil), for a limited time
- wearing a shoe with a built-up heel to take tension off your Achilles tendon
- RICE method
- The rest, ice, compression, and elevation (RICE) method is usually effective in treating Achilles tendonitis right after you’re injured. This method works in the following way:
Rest :
- Don’t put pressure or weight on your tendon for one to two days until you can walk on the tendon without pain.
- The tendon usually heals faster if no additional strain is placed on it during this time.
- Your doctor may suggest that you use crutches if you need to go long distances while resting your tendon.
Ice:
- Put ice in a bag, wrap the bag in cloth, and place the wrapped bag of ice against your skin.
- Hold the bag on your tendon for 15 to 20 minutes, then take the bag off to let the tendon warm up again.
- The ice usually makes inflammation or swelling go down faster.
Compression :

- Wrap a bandage or athletic tape around your tendon to compress the injury.
- You can also tie an article of clothing around this area.
- This keeps the tendon from swelling too much. But don’t wrap or tie anything too tightly around your tendon, as it can limit blood flow.
Elevation :
- Raise your foot above the level of your chest.
- Because your foot is higher than your heart, blood returns to the heart and keeps the swelling down.
- This is easiest to do by lying down and putting your foot on a pillow or other raised surface.
Surgical Treatment :
- In a case where this treatment isn’t effective, surgery may be necessary to repair your Achilles tendon.
- If the condition worsens and is left untreated, there’s a greater risk of an Achilles rupture, which requires a surgical intervention.
- This can cause sharp pain in the heel area.
- Your doctor may recommend a few options for a tendon rupture surgery based on how severe your rupture is and whether you’ve had a rupture before.
- Your doctor will usually refer you to an orthopedic surgeon to decide which procedure is best for you.
One surgical method is called open repair:

- In this surgery, a surgeon makes an incision to open your leg above the heel bone.

- Then they sew the two sides of the ruptured tendon back together and close the incision.
In another method :
- a surgeon makes an incision to open the area on your leg where the rupture happened.
- Then they pass needles with sutures through the tendon and the skin and back out through the incision.
- Finally, they tie the sutures together.
Complications of Achilles tendonitis :
- The most common complications of Achilles tendonitis are pain, having trouble walking or exercising, and your tendon or heel bone becoming deformed.
- You can also experience a complete tear, or rupture, of your Achilles tendon. In this case, you’ll usually need surgery to fix the rupture.
- other complications such as infection or difficulties in wound healing are possible, though uncommon, after a surgery for Achilles tendonitis.
- Complications can worsen if you don’t follow your doctor’s instructions after an operation.
- If you continue to put stress or wear on your Achilles tendon after a surgery, your tendon can rupture again.
Recovery and outlook from Achilles tendonitis :
- Tendonitis usually goes away after a few days, following rest and proper home treatment (including the RICE method). Recovery takes a lot longer if you continue to put pressure on the tendon or don’t change your exercise habits to prevent another injury or rupture.
- Long-term tendonitis can cause worse issues, including insertional tendonitis, or the tendon inserting itself into the heel bone, and tendonosis, or weakening of the tendon.
- A tendon rupture or chronic tendonitis may require long-term treatment or surgery. Recovery from surgery can take anywhere from a few weeks to a few months for full recovery.
- Seeking treatment for your tendonitis or ruptured tendon right away is very important. Carefully following your doctor’s instructions will give you a much better chance for a quick recovery.
- Posture Correction Exercises and Physical Therapy
Because they can help reduce weakness and compensations, physical therapy and other types of form/postural adjustments have been shown to be beneficial for those with Achilles tendinitis (especially noninsertional tendinitis). - A physiotherapist can help show you how to correctly perform eccentric exercises and stretches targeting the Achilles, along with improving posture and range of motion in other ways to prevent future inju
Preventing Achilles tendonitis :
To lower your risk of Achilles tendonitis, try to:

- Stretch your calf muscles at the beginning of each day to improve your agility and make your Achilles tendon less prone to injury.
- Try to stretch before and after workouts.
- To stretch your Achilles tendon, stand with a straight leg, and lean forward as you keep your heel on the ground.
- Ease into a new exercise routine, gradually intensifying your physical activity.
- Combine high- and low-impact exercises, such as basketball with swimming, to reduce constant stress on your tendons.
- Choose shoes with proper cushioning and arch support.
- Also make certain the heel is slightly elevated to take tension off your Achilles tendon.
- If you’ve worn a pair of shoes for a long time, consider replacing them or using arch supports.
- Reduce the heel size of shoes gradually when transitioning from high heels to flats.
- This allows your tendon to slowly stretch and increase its range of motion.
Outlook :
Recovery depends on how severe the tendinitis is.
- The AAOS says that it may take several months for the pain to go away, even with early treatment.
- If the pain does not resolve within 6 months, surgery may be necessary. Those who have surgery may not be able to return to competitive sports or running for at least 12 months. Some cannot return to their sport.
- Prevention and early treatment are the best way to prevent long-term problems.
Prevention :
- warming up
- Warming up before exercise can prevent injury.
- Achilles tendinitis cannot be completely prevented, but the risk of developing it can be reduced by being aware of the possible causes and taking precautions.
These include:
- Varying exercise: Alternating between high-impact exercises, such as running, and low-impact exercise, for example, swimming, can reduce stress on the Achilles tendon on some days.
- Limiting certain exercises: Too much hill running, for example, can put excessive strain on the Achilles tendon.
- Wearing the correct shoes and replacing them when worn: Shoes that support the arch and protect the heel create less tension in the tendon.
- Using arch supports inside the shoe: This can help if the shoe is in good condition but does not provide the required arch support.
- Gradually increasing the intensity of a workout: Achilles tendinitis can occur when the tendon is suddenly put under too much strain, so warming up and increasing the level of activity gradually gives the muscles time to loosen up, and this puts less pressure on the tendon.
- It is important to stretch and warm up before and after exercising. Stretching helps to keep the Achilles tendon flexible, so there is less chance of tendinitis developing. Stretching every day, including rest days, will further improve flexibility.
Physiotherapy Treatment:
Physiotherapy treatment is Pain relieving Electrotherapy modalities such as Short wave Diathermy(SWD), Interferential therapy(IFT), TENS, and Ultrasound therapy helps to relieve pain and muscle spasms.
Regular stretching and strengthening exercise of the calf muscle is an important part of treatment.
Stretching :
- Moreover, stretching before you exercise is important for preventing an Achilles tendon injury. Some basic stretches include the following: –Achilles tendon stretch – Calf stretch – Plantar fascia stretch (Maintaining some flexibility along the bottom of the foot, can also improve Achilles tendon health.)
- Besides stretching, be sure you begin exercising slowly and then ramp up your pace—in other words, allow for a proper warm-up.

- Wrap a strap or another band (such as a thera-band used by some physical therapists) under your affected foot for resistance, placing it under the toes and then tilting the heel back gently.
- Pump the heel slowly and carefully to loosen up the tendon, repeating about 10–15 times.
- Do three sets of 10–15 repetitions daily, unless you notice soreness and increased pain.
- Stand at the edge of a stair with just the front half of your foot on the stair.
- Lift your heels off the ground then slowly lower your heels to the lowest point possible. Repeat 5–15 times, several times daily.
- Improve the flexibility of the ankle joints and varying your exercise moves to include all different ranges of motion.
- Roll the ankles in small circles in the air while laying down, or lift the toes against a wall while gently pumping the heel.

Strengthening :

- Some experts also believe that eccentric strengthening of the Achilles tendon, gastrocnemius, and soleus muscles may reduce the risk of Achilles tendonitis and calf strain.

Ergonomics:
Other tips that may help prevent an Achilles tendinitis include:
- Always wear shoes that provide adequate cushioning for your heel and good arch support
- Avoid running on hard surfaces
- Avoid exercising outside in cold weather
- Use footwear with heel and soft sole
Related Other Article Related To Heel Pain :





11 Comments