Brachial Plexus Block
Table of Contents
What is the Brachial plexus block?
Brachial plexus block is a regional anesthetic method occasionally used instead of or in addition to general anesthesia for upper extremity surgery. This procedure involves injecting local anesthetic drugs near the brachial plexus, which temporarily blocks sensation and movement of the upper extremities. The individual can be awake during the surgical operation, or they can be sedated or completely anesthetized if required.
There are several methods for performing a brachial plexus nerve block. These procedures are classified based on where the needle or catheter is placed to provide the general anesthesia, such as an interscalene nerve block in the cervical spine.
- Supraclavicular nerve block above the neck region,
- Infraclavicular nerve block below the clavicle region,
- Axillary nerve block in the armpit.
Indication
General anesthesia can cause low blood pressure, undesired reductions in cardiac output, central nervous system depression, respiratory depression, loss of protective airway reflexes (such as coughing), the requirement for tracheal intubation and mechanical breathing, and persistent sedative effects.
- Surgery is planned to be confined to the area between the middle of the shoulder and the fingers.
- A block has no contraindications, including infection at the injection site, major bleeding disorder, anxiety, allergy, or intolerance to local anesthetics.
- The patient prefers this treatment to other accessible and appropriate options.
Contraindications
Brachial plexus blocks should be avoided if there is an active infection or a pus pocket at the injection site or if the patient is allergic to the local anesthetic used for the procedure. Other contraindications unique to each block are listed below.
Interscalene brachial plexus blocks are not indicated for certain respiratory-related problems and cardiac problems. Diaphragmatic paralysis can cause respiratory insufficiency; hence, morbid obesity may be a relative contraindication.
Superior trunk blocks have similar contraindications as interscalene blocks, but phrenic nerve palsy appears to occur less commonly. The dorsal scapular nerve passes through the middle scalene muscle and is frequently seen at the normal injection site.
Supraclavicular brachial plexus blocks should be performed with caution in patients with a low pulmonary reserve, since any ensuing pneumothorax can dramatically exacerbate their respiratory condition. This relevant contraindication includes known pneumonia disease on the contralateral side.
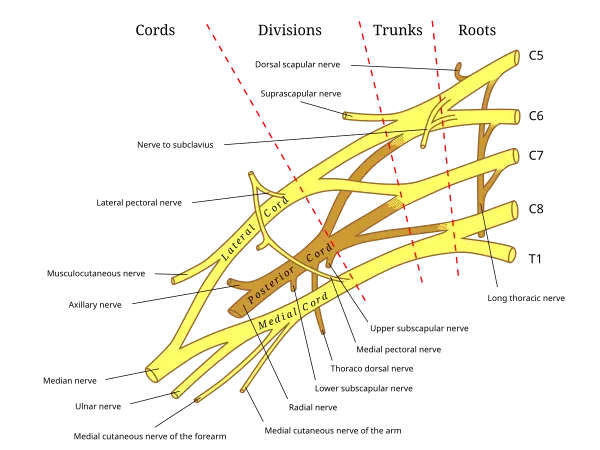
Anatomy
The brachial plexus can be blocked using a variety of ways, beginning with the interscalene block and progressing to the axillary, supraclavicular, and infraclavicular blocks. All of these approaches to the brachial plexus are based on the idea that the neurovascular bundle is encased in a sheath that extends from the deep cervical fascia to just outside the axillary borders.
Complication
Brachial plexus block, like any other operation that disrupts the skin’s integrity, might result in infection or bleeding. People who use anticoagulants are more likely to develop bleeding problems.
Disadvantages of brachial plexus block involve intravenous or intravascular injection, which can produce general anesthetic toxicity. This can be characterized by severe central nervous system issues such as epileptic seizures, depression, and coma. Cardiovascular symptoms of local anesthetic toxicity include a lowering of the heart rate and impaired capacity to pump blood through the circulatory system, which can lead to cardiac collapse.
Inadvertent subarachnoid or epidural distribution of local anesthetic might result in respiratory collapse.
Due to the lung’s proximity to the brachial plexus at the level of the clavicle bone, pneumothorax is the most common complication associated with this block, with an increased risk of up to 6.1 percentSupraclavicular nerve block can also occur in subclavian artery puncture and local anesthetic distribution, causing paresthesia of the stellate ganglion, phrenic nerve, and recurrent laryngeal nerve.
Technique or Treatment.
Anesthesiologists are often the ones who conduct brachial plexus blocks. Injecting where the paresthesia is felt can lead to a successful nerve block. Transarterial, paresthesia-elicitation, and the use of a peripheral nerve simulator or portable ultrasound scanning equipment are all common ways for acquiring such a needle location. Suppose the needle comes into a nerve. In that case, the individual may suffer paresthesia (a sudden tingling sensation similar to “pins and needles” or an electric shock) in the arm, hand, or fingers. Injection at the spot where that tingling sensation (paresthesia) is felt could lead to a successful nerve block.
A peripheral nerve simulator linked to an appropriate needle allows an electric current to be emitted from the tip. When the needle tip comes into contact with a motor neuron, the innervated muscle may contract as expected. Modern portable ultrasound instruments enable the operator to see interior anatomy, including the nerves to be blocked, adjacent anatomic structures, and the needle as it approaches the nerves. Observation of local anesthetic around the nerves during ultrasound-guided injection predicts a successful block. This table shows the recommended nerve blocks for specific procedures or locations.
| Procedure Site | Interscalene | Supraclavicular | Infraclavicular | Axillary1 |
| Shoulder2 | ++ | +3 | ||
| Arm2 | + | ++ | + | |
| Elbow2 | ++ | ++ | + | |
| Forearm2 | + | ++ | ++ | |
| Hand2 | + | + | ++ |
Include the musculocutaneous nerve 2. Include T1-T2 if the block is anesthetic 3. Include C3-C4 if the block is anesthetic
Interscalene block
The interscalene block is achieved by injecting a local anesthetic into the brachial plexus nerves as they travel through the groove between the anterior and middle scalene muscles, near the cricoid cartilage. This block is very beneficial for giving anesthetic and postoperative pain relief during clavicle, shoulder, and arm surgery.
The advantages of this block include quick shoulder blockage and anatomical markers that are very easy to palpate. One disadvantage of this block is that it provides insufficient anesthesia in the ulnar nerve distribution, making it unsuitable for surgeries on the forearm and hand.
Side effects
Almost everyone who has had an interscalene or supraclavicular brachial plexus block experiences temporary paresis (thoracic diaphragm function impairment). Pulmonary function tests can reveal significant respiratory impairment in some persons. In certain persons, such as those with severe chronic obstructive pulmonary disease, this might lead to respiratory failure, necessitating tracheal intubation and artificial ventilation until the block resolves. Horner’s syndrome may occur if the local anesthetic solution travels cephalad and inhibits the stellate ganglion. This can be accompanied by difficulties swallowing and vocal cord paralysis. These signs and symptoms, however, are temporary and seldom cause long-term difficulties, though they can be quite stressful for patients until the effects wear off.
Contraindication
- Severe chronic obstructive pulmonary disease
- Phrenic nerve paresis
Supraclavicular block
The supraclavicular block is an effective choice for arm and forearm surgeries because a single injection at this site quickly produces strong numbness in the entire arm. The brachial plexus is most compressive at the level of the trunks made by the C5-T1 nerve roots; hence, nerve block at this level offers the best chance of blocking all of the brachial plexus branches. This leads to short start times and, eventually, great success rates for upper extremity surgery and analgesia, except for the shoulder.
Surface landmarks can be used to determine the appropriate proper location for general anesthetic injection, which is usually outside the lateral border of the sternocleidomastoid muscle and above the neck area, shoulder blade, with the first rib representing the limit below which the needle should not be directed (the pleural cavity and uppermost part of the lung are at this level). The subclavian artery, located just above the collarbone, can be palpated or imaged with ultrasound to help find the brachial plexus, which lies lateral to the artery in this position. You can tell how close you are to the brachial plexus in a few ways: by getting a tingling sensation (paresthesia), by using a device that stimulates nerves with electricity, or by looking with an ultrasound machine.
The supraclavicular block gives an extra full block of the median, radial, ulnar, and musculocutaneous nerves compared to the interscalene block; nevertheless, it does not provide postoperative pain relief. However, the supraclavicular nerve block is typically easier to do and may result in a smaller amount difficulties than the interscalene nerve block. In comparison to the infraclavicular and axillary nerve blocks, the effective accomplishment of sufficient anesthesia for upper limb surgery is roughly similar to the supraclavicular nerve block.
Unlike the interscalene nerve block, which causes diaphragmatic hemiparesis in all individuals, only half of those who receive a supraclavicular nerve block develop this adverse effect. One disadvantage of the supraclavicular block is the possibility of pneumothorax, which is thought to be 1%-4% when employing paresthesia or peripheral nerve simulator-guided procedures. Ultrasound guidance enables the operator to visualize the first rib and the pleura, ensuring that the needle does not penetrate the pleura. This minimizes the chance of pneumothorax.
Infraclavicular block
The current study suggests that when using a peripheral nerve stimulator for an infraclavicular block, a double-stimulation technique is more effective in finding nerves than a single-stimulation method. Furthermore, an infraclavicular nerve block is just as effective as an axillary nerve block performed with multiple stimulations. However, it may be connected with a quicker performance time and reduced procedural discomfort for the patient.
Axillary block
The axillary block is the most dependable of the four fundamental approaches to the brachial plexus because it avoids phrenic nerve paresis and the formation of pneumothorax. It is also particularly effective for anesthetic and after-pain treatment during elbow, forearm, wrist, and hand surgery. The easily perceptible axillary artery serves as a reliable anatomical reference for this block, and administering local anesthetic near it usually results in a successful brachial plexus block.. The axillary block is very beneficial for delivering anesthetic and postoperative pain relief during elbow area, forearm, wrist joint, and hand surgery.
The axillary block is also the most dependable of the four primary approaches to the brachial plexus because it avoids phrenic nerve paresis and the formation of pneumothorax. The brachial plexus nerves and the axillary arteries are surrounded by a thick, protective fibrous coating. This layer is an outgrowth of the neck’s dense connective tissue, known as the deep cervical fascia.
The easily perceptible axillary artery serves as a reliable anatomical reference for this block, and administering local anesthetic near it usually results in a successful brachial plexus block. The axillary block is an excellent method for providing anesthesia and postoperative pain management during elbow, forearm, wrist, and hand surgery. The axillary block is also the most dependable of the four primary approaches to the brachial plexus because it avoids phrenic nerve paresis and the formation of pneumothorax.
Single-injection methods often don’t reliably block the areas supplied by the musculocutaneous and radial nerves. Current research shows that a triple-stimulation approach—with injections on the musculocutaneous, median, and radial nerves—is the optimum strategy for the axillary block.
FAQ
How do you do a brachial plexus block?
Inject 1 to 2 mL of a local anesthetic to ensure proper tip insertion and spread into the interscalene groove, inducing spread around the nerve roots. Once the insertion has been checked, repeat the incremental injection and negative aspiration until the local anesthetic has been distributed evenly.
What is the landmark of the brachial block?
Interscalene Brachial Plexus Block: Landmarks and Nerve…
Landmarks of the low interscalene procedure to brachial plexus block:
(1) clavicle.
(2) The posterior edge of the sternocleidomastoid muscle.
(3) External jugular vein.
The palpating fingers are located in the scalene “groove” located between the anterior and middle scalene muscles.
What’s the most frequent brachial plexus block?
The most common blocks are axillary, infraclavicular, supraclavicular, and interscalene. To employ these blocks properly, one needs to understand brachial plexus anatomy and the practical clinical differentiation between the blocks.
What is the most usual route to a brachial plexus block?
Axillary block is a basic regional anesthetic technique and may be the most popular kind of brachial plexus block.
What is the location of the brachial block?
A brachial plexus block is a medical technique in which a dosage of local anesthetic is administered into a region of your neck, above your collarbone, or into your upper arm (near the armpit).
Reference
Wikipedia contributors. (2025b, May 25). Brachial plexus block. Wikipedia. https://en.wikipedia.org/wiki/Brachial_plexus_block
Pester, J. M., Hendrix, J. M., & Varacallo, M. A. (2023, August 4). Brachial plexus block techniques. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470213/







