DEGENERATIVE DISC DISEASE (DDD): Physiotherapy Treatment
Table of Contents
What’s degenerative disc disease?
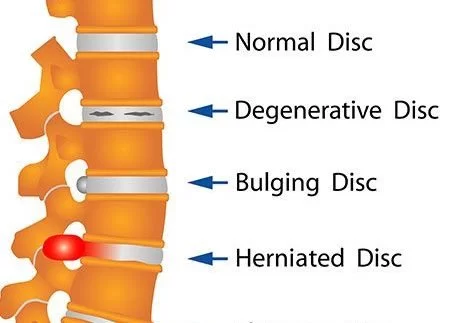
Degenerative disc disease is a condition in which the discs between two or more vertebrae begin to deteriorate. A disc is a soft cushion that sits between the bones of the spine where it acts as a shock absorber. As discs age, they can become less elastic and begin to wear down causing pain and stiffness. Degenerative disc disease is one of the most common causes of back pain.
Degenerative disc disease is a medical condition that occurs when the discs in the spine begin to break down over time, causing changes in the way that the spine functions. Discs are made from a gel-like substance that is surrounded by a tough membrane which serves to separate each vertebrae of the spine. Degeneration of discs can cause pain and discomfort, and it can also lead to a more serious condition called spinal stenosis.
The intervertebral discs of the spine begin to break down gradually over-time, resulting in pain and stiffness in the back. It is a common condition, especially among older people, and it can result from a number of causes.
Spinal disks are like shock absorbers between the vertebrae, or bones, of your spine. They help your back stay flexible, so you can bend and twist. As you get older, they can show signs of wear and tear. They begin to break down and may not work as well.
Nearly everyone’s disks break down over time, but not everyone feels pain. If worn-out spinal disks are the reason you’re hurting, you have degenerative disk disease.
DEFINATION :
Degenerative disc disease (DDD) represents a wide category of back pain resulting from or associated with the degeneration of intervertebral discs. It involves a process where the intervertebral discs lose height and hydration.
When this occurs, the discs are unable to fulfill their primary functions of cushioning and providing mobility between the vertebrae. Although the exact cause is unknown, it is thought to be associated with the aging process during which the intervertebral discs dehydrate, lose elasticity, and collapse.
Despite its name, degenerative disc disease is not so much of a disease, but a natural occurrence that comes with aging. Degenerative disc disease may develop at any level of the spine, but is most common in the cervical and lower lumbar regions.
Clinically Relevant Anatomy
Lumbar degenerative disc disease is a condition that maybe a cause of lower back pain, which results from the co-existence of two different time scales, the slow dynamics of disc degeneration and the fast dynamics of pain recurrence.
Lumbar degenerative disc disease can also imply radiating pain from damaged discs in the spine. A lumbar spinal disc acts as a shock absorber between two vertebrae and allows the joints and the spine to move easily.
The outer region of the disc, the annulus fibrosis, surrounds the soft inner core of the disc, the nucleus pulposus. Spinal discs undergo degenerative changes as we age, but not everyone will have symptoms as a result of these changes. Neural inflammation is one such possible cause of pain. When the outer section of the disc ruptures, the inner core can leak out, releasing proteins that irritate the neural tissue. Another cause is when discs can no longer absorb stress as well, leading to abnormal movement around the vertebral segment and causing back muscles to spasm as they try to stabilise the spine. In some cases the segment may collapse, causing nerve root compression and radiculopathy. Pain often reduces with time as the inflammatory proteins dissipate and the disc collapse settles into a stable position.
Pathology
Degenerative Disc Disease is thought to begin with changes to the annulus fibrosis, intervertebral disc, and subchondral bone. The process of degeneration is divided into three classifications: early dysfunction, intermediate instability, and final stabilisation.
Early dysfunction is the start of degenerative changes which can occur as early as 20 years old.Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause lower back pain.Final stabilisation is where fibrosis develops in the posterior structures and osteophytes form. Pain and motion both decrease.
What causes degenerative disc disease?
Your spinal disks are made up of a soft inner core and a tough outer wall. The disks change in ways that may cause degenerative disk disease, such as:
1) Dry out. When you’re born, the disks in your spine are mostly made up of water. As you age, they lose water and get thinner. Flatter disks can’t absorb shocks as well. The water loss also means less cushion or padding between your vertebrae. This can lead to other problems in your spine that may cause pain.
2) Crack. The stress of everyday movements and minor injuries over the years can cause tiny tears in the outer wall, which contains nerves. Any tears near the nerves can become painful. And if the wall breaks down, the disk’s soft core may push through the cracks. The disk may bulge, or slip out of place, which is called a slipped or herniated disk. It can affect nearby nerves.
Degenerative disc disease symptoms :
You’ll probably feel a sharp or constant pain in your back and neck. Your exact symptoms depend on where the weak disk is and other changes it has caused.
Common signs include pain that:
- Is in your lower back, buttocks, or upper thighs Comes and goes. It can be nagging or severe, and can last from a few days to a few months.
- Feels worse when you sit, and better when you move and walk
- Feels worse when you bend, lift, or twist
- Gets better when you change positions or lie down In some cases, degenerative disk disease can lead to numbness and tingling in your arms and legs. It can also cause your leg muscles to become weak. This means the damaged disks may be affecting the nerves near your spine.
DIAGNOSIS
When the pain started
1) Which part of your spine hurts
2) If it has spread to other parts of your body
3) If you’ve had past spine injuries
4) If you have a family history of similar problems
5)He’ll look at your spine for signs of the condition, like pain in your lower back or neck. He may also ask you to walk or bend to see which movements cause pain.
degenerative disc disease occur with condition such as:
- idiopathic low-back pain
- lumbar radiculopathy
- myelopathy
- lumbar stenosis
- spondylosis
- osteoarthritis
- zygapophydeal joint degeneration
Activities that typically increase pain include:
- Sitting for extended periods of time
- Rotating, bending, or lifting
- Activities that typically decrease pain include:
Frequent changes in positions
- Lying down
- Staying active
Differential Diagnosis
People with DDD will often present with low back pain with varying levels of severity between individuals. Pain is often chronic, but can also be acute on chronic with varying episodes of exacerbation
There are different degrees of annular disruption[3] which are classified into 5 grades. These grades are differentiated by means of a contrast medium injection.
- Grade 0: no disruption
- Grade 1: the contrast medium passes into the cartilage endplate through a tear
- Grade 2: the contrast medium flows into the bony endplate
- Grade 3: the contrast medium enters into the cancellous bone of vertebra under endplate
- Grade 4: the contrast medium leaks completely in the cancellous bone.
Investigation
X-ray or MRI to check for bone or nerve damage near your spine
Treatment for degenerative disc disease
The goal is to ease pain and stop more damage. Your doctor will suggest the best treatment plan for you, based on your symptoms and how serious your condition is.
It affects mainly people older than 40 years. The best way to prevent degenerative disc disease is to maintain a healthy weight and to be physically active (Active life-style). A well-designed and maintained exercise program can be beneficial. Physical therapy and other forms of treatment will also be useful.
Treatment may include:
1) Medical Treatment :
The preferred treatment protocol for patients with chronic low back pain, as a result of disc degeneration, is conservative management of physical therapy and medication.
Conservative treatment includes rest, adequate stimulation for motor activity, regular physical activity, muscle strengthening, analgesic medication, physiotherapy, rehabilitation programs and lifestyle adjustments, such as weight loss.
Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (e.g. Tylenol) help patients to feel confident enough to engage in their regular activities. Stronger prescription medications such as oral steroids, muscle relaxants or narcotic pain medications may also be used to manage intense pain episodes on a short-term basis only and some patients may benefit from an epidural steroid injection. Epidural steroid injections can provide low back pain relief by delivering medication directly to the painful area to decrease inflammation.
2) Steroid shots.
These have strong medications to ease pain, swelling, and inflammation. Your doctor may suggest you get a shot in the
epidural space in your back, a fluid-filled area around the spinal cord, or get one in your nerve or muscle.
3) Surgery
If other treatments don’t work, your doctor may recommend surgery. One procedure, called a discectomy, removes the injured part of the disk. This helps take pressure off your nerves.
In some cases, your doctor might remove the whole disk and put an artificial one in. If you have a severe problem, your doctor might fuse (permanently connect) the bones in your spine after he removes the disk.
Taping or bracing can also help in reduce pain. Surgery to remove the disc is usually recommended when conservative treatment has failed. The use of steroids or the use of painkillers may temporarily relieve pain, but a permanent cure is rarely achieved. Surgery carries risks and may have long term side effects.
4) Physiotherapy Treatment
Physical therapy can help prevent the symptoms of degenerative disc disease and help you with the rehabilitation of your body. Physiotherapy treatment can help you with the following: movement assessment and re-education, spinal stabilization, training and conditioning, and functional movement.
One of the main aims of physical therapy is to reduce pain. Various physical modalities are used, including heat and cold application, traction, spinal manipulations , exercise programs and electrical stimulation such as ‘IFT’ and ‘pulsed radiofrequency (PRF)’ treatment and lifestyle modifications (e.g., weight reduction, smoking cessation).
Amongst exercise approaches, unloaded movement facilitation exercises of McKenzie, core strengthening, and core stabilization exercises are all effective in pain reduction for degenerative disc disease.
*Spinal manipulations
Spinal manipulations have traditionally been used to relieve lower back pain, but the effects are generally only temporary. The HVLA (High-Velocity, Low-amplitude) is a manipulation that includes many different techniques and may involve preliminary preparation of the joint and its surrounding tissues, using stretching, assisted motion and other methods. Loads, both forces and moments, are applied to the joint, and it is moved to its end range of voluntary motion. An impulse is then applied, the effective load is the summation of forces applied by the therapist, with the inertial forces
generated by the motion of body segments, and the internally generated tensions from client muscle reactions.
This technique can immediately improve self-perceived pain, spinal mobility in flexion and hip flexion during the passive SLR test, but Paige et al reported only moderate improvements in pain and with (transient) minor musculoskeletal harms Before Spinal Manipulation Therapy (SMT) can be considered as a treatment option, patients with LBP need to be screened for possible serious pathology.
There are two reasons for this: some conditions, such as a fracture, affect the mechanical integrity of the spine and would make SMT clearly dangerous. In other conditions, a failure to recognize the condition delays commencement of more appropriate care. For example, early detection and treatment of spinal malignancy is important to prevent the spread of metastatic disease and the development of further complications such as spinal cord compression. Application of SMT with the presence of any red flags are considered as contraindications to SMT until further investigation has excluded other pathologies.
Degenerative disc disease exercises :
Degenerative disc disease exercises are mainly core stability exercise and flexibility exercise and Back muscle strengthening exercise.
Core Stability Exercise :
Strength training aims to enhance core stability by strengthening and improving the coordination between the abdominal and back muscles. Core Stabilisation exercises will increase a patient’s capacity to resist higher loads in the degenerative discs. This is a key element for prevention and treatment of injury as muscle tissue reduces at a rate of 1 kg/year after the age of 40.
A posterior dynamic stabilisation programme will have result in a significant improvement in pain and disability. Training exercises performed 1-3 times a week reduces pain and should be continued once pain has subsided and patients are able to return to their jobs and hobbies/activities and are able to cease the use of analgesics.
Exercises are performed to reduce pain and to ensure stability by strengthening the hip extensors, hip flexors, abdominal muscles and the sacrospinalis muscles. Other important exercises include engaging of the pelvis musculature to restore body symmetry, such as the back extensors and abdominal muscles. The Williams method suggests stretching of the back extensors and strengthening of the abdominal muscles to relieve some of the pressure placed on the lumbar intervertebral discs.
Flexibility exercise :
A lack of flexibility through the hips (hamstring, hip flexors, gluteus muscles) can contribute to low back pain, therefore it is important to work on this if you are experiencing back pain. Please make sure all stretches are “pain free”. If you feel discomfort, you may not be ready to do that specific stretch.
1- Quadriceps Stretch

Using a towel, or band, lie on your stomach, attach the band to affected
foot and pull your heel to your butt. Hold this stretch for 1 min. Repeat
3 times.
2- Hip Flexor Stretch
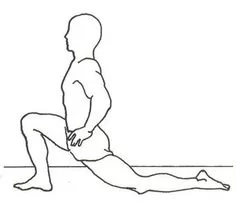
Kneel with affected knee on the ground, same side arm goes back
causing pelvis (hips) to shift forward, and back to extend. Hold for 20-
30 seconds. Repeat 3 times.
3- Adductor Stretch
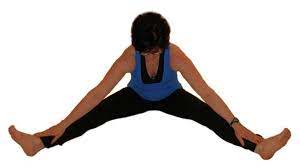
Prop the inside of your ankle up on a table, lean into the side you’re
stretching. Hold for 20-30 seconds. Repeat 3 times.
4- Hamstring Stretch
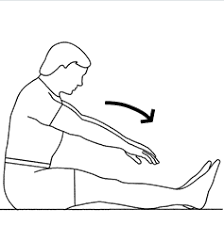
Prop the back of your heel up on a table, keep your back straight, and
lean forward at the hips. Hold for 20-30 seconds. Repeat 3 times.
5- Dynamic Hamstring Stretch

Lie on your back, reach hands behind your knee, keep knee at 90
degree angle, and kick up until you feel stretch. Repeat 15-20x each
side.
6. lying ITBand Stretch
Lie on your side, use a towel, or band and pull foot back as if stretching
quadriceps, use opposite foot to push down on distal part of leg. Hold
this stretch for 1 min. Repeat as needed.
7- C stretch for ITBand
In standing, place affected leg behind the good leg, and lean away.
Hold for 20-30 seconds. Repeat 3 times.
8- Glute Stretch
Prop the outside of your ankle up on a table, make sure leg is at 90
degrees, keep your back straight, and lean forward at the hips. Hold for
20-30 sec. Repeat 3 times.
9- Prayer Cat and Camel
Start on all fours. Prayer- Exhale as you sit back onto heels, lower head,
tuck chin and reach arms out. Cat- Inhale as you arch the back up and
hollow out abdominals while head remains tucked. Camel- Exhale and
lower abdominal and reach chin towards ceiling. Tuck chin and sit back
into Prayer position. Repeat 5 times.
STRENGTHENING EXERCISES EASY
Supine hip twist on physioball
Supine Lie on your back on floor with hips and knees bent to 90 degrees over a physioball; draw in abdominal muscles and maintain throughout exercise; slowly and with control, rotate knees to one side keeping hips in contact with the floor; engage obliques to pull knees back to center and repeat on opposite side; Repeat 10-20 times on each side.
Supine Abdominal Draw In
Lie on your back on a table or mat, knees up with feet flat on table/
mat; pull the abs in and push your low back to the table/mat. Repeat
20 times.
Abdominal Draw In with Knee to Chest
Lie on your back on table or mat, draw one knee to the chest while
maintaining the abdominal draw in; do not grab the knee with your
hand. Repeat 10-20 times each leg.
Abdominal Draw In with Heel Slide
Lie on your back on table or mat, draw the heel back towards the
buttock while maintaining the abdominal draw in. Maintain as you
return to the start position. Repeat 10-20 times each leg.
Abdominal Draw In with Double Knee to Chest
Lie on your back on table or mat, bring both knees to your chest at
the same time. Maintain the abdominal draw in throughout the entire
exercise. Repeat 10-20 times.
Supine Twist
Lie on your back on floor with hips and knees bent to 90 degrees with
feet flat on floor; draw in abdominal muscles and maintain throughout
exercise; slowly and with control, rotate knees to one side keeping hips
in contact with the floor; engage obliques to pull knees back to center
and repeat on opposite side; Repeat 10-20 times.
Prone Bridging on Elbows
Lie on your stomach on a table or mat with your forearms/elbows on
the table/mat; rise up so that you are resting on your forearms and
toes; maintain abdominal draw in; your back should be completely
straight; hold this position for 15 sec – 1 min. Progress in increments
of 15 seconds. Repeat 5-10 times.
Side Bridging on Elbow
Lie on your side with your elbow underneath you; rise up so that
you are resting one forearm/elbow and foot on same side; hold this
position for 15sec – 1min. Progress in increments of 15 seconds.
Repeat 5-10 times. Make sure to complete exercise on both sides.
Press Ups
Lie on your stomach on table or mat with legs extended and hands
palm down just above shoulders; retract shoulder blades down and in
towards the midline of your spine; maintaining that position, lift your
chest off of the floor; hold for 3-5 seconds keeping the back of the
neck long and making sure front hip bones stay in contact with mat
during entire movement.. Repeat 10-20 times.
Prone Cobra’s
Lie on your stomach on a table or mat with your arms at your side;
lift your head and chest off the table/mat; hold your glutes (buttock
muscles) tight and squeeze your shoulder blades together; hold briefly
and return to starting position. Repeat 10-20 times.
Superman’s
Lie on your stomach on table or mat with arms and legs extended;
retract shoulder blades down and in towards the midline of your spine
and draw in abdominal muscles; maintaining this position, lift opposite
arm and opposite leg ensuring that your hips stay in contact with the
floor; hold for 3-5 seconds and reverse sides. Repeat 10-20 times.
Quadruped Opposite arm/leg
In a quadruped position (on all fours); keep head straight with knees
bent to 90 degrees. Engage your core to keep back straight during
entire exercise and use your hamstrings, glutes, and low back muscles
to lift your leg straight while simultaneously lifting opposite arm;
Repeat 10 times each side.
Degenerative disc disease surgery
There are several treatments to help individuals with degenerative disc disease, and the goal of surgery is to remove the part of the disc that is causing the most pain. The surgery is usually performed in conjunction with a fusion. Fusion is the process of fusing or permanently joining together two or more bones, and when it is performed for degenerative disc disease, it is called lumbar fusion. Fusion for degenerative disc disease produces many benefits, including improved functioning of the nervous system and elimination or reduction of pain.
There is extensive evidence to suggest that degenerative disc disease surgery is often beneficial in the treatment of spinal disorders. However, many patients are sceptical of the success of this type of treatment because of the high risk of complications. Patients who have undergone degenerative disc disease surgery can expect to experience pain relief, which can improve their quality of life. This can be achieved by using steroid medication to control inflammation in the area.
In 1996, Degenerative Disc Disease was the second leading cause of back surgery in the United States. By 2006, the number of spinal fusions performed to treat degenerative disc disease had increased by nearly 600%, from 18,500 to 56,000. Degenerative disc disease was the leading reason for spinal fusions in 2006. Many of these surgeries are not necessary and result in complications and other issues.
Despite the fact that degenerative disc disease has been prevalent for centuries, many physicians have failed to adequately address this condition. In the past, surgeons relied on invasive techniques that damaged the surrounding tissue when attempting to remove the degenerative discs. These techniques resulted in a significant amount of pain and discomfort for patients, and a number of surgical complications. However, new surgical techniques have proven to be more successful than surgery that was done in the past.








14 Comments