Arthritis of the temporomandibular joint
Table of Contents
What is arthritis of the temporomandibular joint?
Arthritis of the temporomandibular joint is characterized by chronic degeneration of the various hard & soft tissues around the joint.
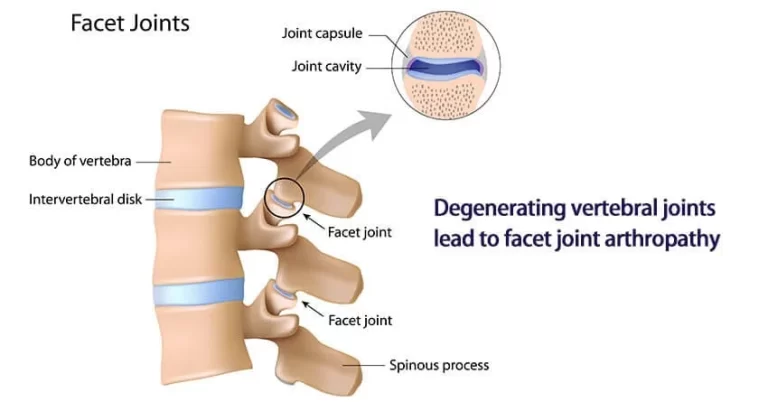
This results in anatomical changes in the joint, & joint pain because of alterations in peripheral and central pain processing mechanisms. Stress-bearing joints of the body such as the knee, hips, spine, & fingers are most commonly affected. Osteoarthritis can also affect other joints in the body such as the wrist, shoulder, ankle, & Temporomandibular joint (TMJ).
Temporomandibular joint arthritis affects the cartilage, subchondral bone, synovial membrane, & other hard and soft tissues causing changes such as Temporomandibular joint remodeling, articular cartilage abrasion, & deterioration. Osteoarthritis localized to the TMJ might also be a part of this generalized condition.
It is estimated that approximately 15 % of the world’s population suffers from osteoarthritis. Big-scale multicenter, well-conducted epidemiologic studies are lacking in India. Nevertheless, it is estimated that 22–29 % of people in India might have osteoarthritis.
Osteoarthritis can happen at any age, although, it occurs with greater frequency as age increases. At 40 years of age, only 20 % of the population might have osteoarthritis; nevertheless, by 65 years the rates drastically increase & a majority will exhibit radiographic evidence of the disease. A study of subjects in the age group of 73–75 years estimated that 70 % of the subjects have radiographic evidence of osteoarthritis. Nevertheless, in spite of the high prevalence, only 9.6 % of men & 18 % of women ≥60 years have symptomatic Osteoarthritis. The prevalence pattern exhibits a bell-shaped curve with peak prevalence in the 5th and 6th decades followed by a reduction in the progression after 75 years.
In most cases, the pain & discomfort associated with Temporomandibular joint disorders are temporary & can be relieved with self-managed care or nonsurgical treatments. Surgery is typically a last resort after conservative measures have failed, but some people with Temporomandibular joint disorders might benefit from surgical treatments.
temporomandibular joint disorder refers to any dysfunction of the Temporomandibular joint. Many people use the terms TMJ & TMD interchangeably.
Epidemiologic studies on the prevalence of Temporomandibular joint osteoarthritis vary because of variations in diagnostic criteria employed to define the condition. Nevertheless, the prevalence & the symptomatic rates are similar to generalized osteoarthritis. In osteoarthritis of the Temporomandibular joint, clinical evidence of the disease occurs in 8–16 % of the population Temporomandibular joint Osteoarthritis might be unilateral or bilateral & has a strong preference for women. This might be due to Estrogen Receptor alpha polymorphism and might be associated with increased pain susceptibility in female Temporomandibular joint Osteoarthritis patients.
According to the American Academy of Orofacial Pain, Temporomandibular joint Osteoarthritis is categorized into primary & secondary. Primary Temporomandibular joint osteoarthritis is characterized by the absence of any distinct local or systemic factor. Secondary Temporomandibular joint osteoarthritis is however associated with a previous traumatic event or disease.
What are the causes of arthritis of the temporomandibular joint?
Arthritis has a complex & multifactorial cause. Risk factors include age, genetics, trauma such as previous instances of fracture, repetitive adverse loading, high-impact & torsional loads, external or overt jaw trauma & instances of prolonged micro-trauma, disturbances of joint or muscle joint instability, inadequate muscle strength or endurance, internal derangements, discectomy, ligament laxity, systemic conditions generalized osteoarthritis, infection & idiopathic degenerative process, congenital & developmental abnormality. Bruxism (teeth grinding or clenching). Dislocation of the disc in the ball & socket joint.
In most cases, the pain & discomfort associated with Temporomandibular joint disorders are temporary & can be relieved with self-managed care or nonsurgical treatments. Surgery is typically a last resort after conservative measures have failed, but some people with Temporomandibular joint disorders might benefit from surgical treatments.
Etiopathogenesis involves a sustained inflammatory process. Metabolic or mechanical factors assist in the early damage to the cartilage. This initiates a series of biomechanical changes in the hard & soft tissues of the joint triggering the immune response. Immune cells trigger an inflammatory reaction by releasing various inflammatory mediators such as cytokines & chemokines. The process is coupled with the activation of the complement system, and the release of cartilage-degrading factors such as matrix metalloproteinase (MMPs) & prostaglandin E (PGE) which further damage the articular cartilage. This results in the eventual degradation & abrasion of joint cartilage & the remodeling of the subchondral bone by the initiation of a local inflammatory response.
Arthritis in the jaw can be lead by:
- osteoarthritis
- rheumatoid arthritis
- psoriatic arthritis
Jaw arthritis can range from mild to severe & might get worse over time. It can also result in symptoms associated with temporomandibular joint disorders.
Other causes of jaw pain
Jaw pain can have many causes, & sometimes there can be more than 1 cause. Pain in the jaw isn’t always associated with bone damage.
Besides arthritis, jaw pain might also be caused by:
- Repetitive motion. Some usual culprits include:
- frequent gum chewing
- fingernail biting
- sinus infection
- a blow to the jaw
- stretching the jaw, like with a dental process
- insertion of tubes during a medical procedure
- misalignment of your teeth
- inherited structural jaw problems
- connective tissue diseases
- Medications. Some prescription drugs might affect your jaw muscles & cause pain.
- Emotional factors. Anxiety, depression, & stress can cause tense, tight jaw muscles or make jaw pain worse.
What are the symptoms of arthritis of the temporomandibular joint?
Temporomandibular joint dysfunction is most usual in those 20 to 40 years of age & is more common in women than in men. In general, the natural course of Temporomandibular joint osteoarthritis is favorable & can be divided into three slow progressive phases, with periods of remission & cartilage regeneration. The starting stage where there is the evolution of the condition is termed the early phase. This might take on average 2.5–4 years.
Clinically it is associated with clicking sounds & intermittent locking. The intermediate phase, associated with Temporomandibular joint destruction, lasts on average 6 months to a year & clinically the patient might undergo spontaneous joint pain at rest or with function, limitation in opening, & grating sounds. The late phase is the stage at which there is no degenerative activity, & the joints are said to be stable or in the “burnout phase”. It lasts about 6 months, & it will eventually stabilize with time therefore if invasive procedures can be postponed with medical management, patients will ultimately benefit from it. There is the absence of joint pain, absence or presence of limitation, & absence or presence of grating sounds. The entire procedure from starting to the final burnout phase takes approximately 5.5 years.
The most common clinical signs & symptoms include pain, restriction in joint function, & joint sounds. Pain is usually dull aching and might have occasional sharp components on movement. Pain is prevalent in the starting phases because of the presence of synovitis. It might be associated with joint stiffness, limitation in mouth opening, and increasing sensitivity to cold and dampness and might be relieved with rest & NSAIDs. Patients usually have morning stiffness for more than 30 minutes, joint crepitus, joint sounds, and absence of joint warmth.
Patients in advanced stages might exhibit facial skeletal remodeling, with chin deviation to the affected side, & unstable or fluctuating malocclusion with occlusal discrepancies. Occlusal changes like skeletal anterior open bite, reduced overbite, and increased overjet might be associated with osteoarthritic Temporomandibular joint. In addition, internal derangements might co-exist in the same joint in approximately one-third of cases.
Some of the most usual features include:
- pain, which can be a dull ache or a sharp stab when moving your jaw
- inflammation in or around your jaw joints
- restricted jaw movements or locking of your jaw
- jaw tenderness
- jaw stiffness, especially in the morning
- a creaking, grating, clicking, or crunching noise (called crepitus)
- difficulty chewing
- facial pain or pain around the ear or neck
- headaches
- tooth pain
Temporomandibular joint disorders are fairly usual, affecting about 10 million trusted Source Americans, according to the National Institute of Dental & Craniofacial Research.
Arthritis in the jaw can make symptoms of Temporomandibular joint disorders. These can include:
- chronic inflammation
- cartilage deterioration
- restriction of movement
The progression and severity of Temporomandibular joint disorders depend on the type of arthritis involved. The mechanism of how arthritis cartilage degeneration results in Temporomandibular joint disorders isn’t fully understood.
What are the types of arthritis of the temporomandibular joint?
Infectious arthritis
Infection of the temporomandibular joint might result from the direct extension of adjacent infection or hematogenous spread of bloodborne organisms. The joint site is inflamed, & jaw movement is limited & painful. Local signs of infection related to evidence of a systemic disease or with an adjacent infection advocate the diagnosis. X-ray results are negative in the early stages but might show bone destruction later. If suppurative arthritis is suspected, the joint is aspirated to confirm the diagnosis & to identify the causative organism. Diagnosis must be made quickly to prevent permanent joint damage.
Treatment includes antibiotics, proper hydration, pain control, & motion restriction. Parenteral penicillin G is the drug of choice until a specific bacteriologic diagnosis can be done on the basis of culture & sensitivity testing. For methicillin-resistant Staphylococcus aureus infections of the oral structures, IV vancomycin is the drug of choice. Suppurative infections are aspirated or drained. Once the infection is controlled, passive exercises of jaw-opening help prevent scarring & limitation of movement.
Traumatic arthritis
Rarely, acute injury (eg, due to difficult tooth extraction or endotracheal intubation) might lead to arthritis of the temporomandibular joint. Pain, tenderness, & limitation of mandibular motion happen. Diagnosis is based primarily on history. X-ray outcomes are negative except when intra-articular edema or hemorrhage widens the joint space. Treatment includes oral corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), the application of heat, a soft diet, & limitation of jaw movement.
Osteoarthritis
The temporomandibular joint might be affected by osteoarthritis (degenerative joint disease), usually in people more than 50 years. Sometimes, patients complain of stiffness, a grating sound on jaw movement, or mild pain. Crepitus might come from disk degeneration or perforation, causing the bone to grate on bone. Joint involvement is generally bilateral. X-rays or cone beam CT might show flattening (eg, subchondral cysts, erosions, & lipping of the condyle, suggestive of dysfunctional change, most likely because of excessive loading of the joint). Management is symptomatic. An oral appliance (mouth guard) worn during sleep (and possibly while awake) might help alleviate pain & reduce grating sounds.
Secondary degenerative arthritis
This arthritis commonly develops in populations aged 20 to 40 years with a history of trauma or persistent myofascial pain syndrome. It is characterized by the limited movement of the jaw, unilateral pain during jaw movement, joint tenderness, & crepitus. When it is related to myofascial pain syndrome, symptoms wax, & wane.
Unilateral joint involvement helps differentiate secondary degenerative arthritis from osteoarthritis. Diagnosis is based on x-rays, which, as in osteoarthritis, commonly show condylar flattening, lipping, spurring, or erosion.
Treatment is conservative, as it is for myofascial pain syndrome, although arthroplasty or high condylectomy might be required. An oral appliance (occlusal splint [mouth guard]) commonly relieves symptoms. The appliance is worn continuously, except during meals, oral hygiene, & appliance cleaning. When symptoms resolve, the length of time that the appliance is worn each day is slowly decreased. Intra-articular injection of corticosteroids might relieve symptoms but might harm the joint if repeated frequently.
Rheumatoid arthritis
The temporomandibular joint is affected in > 17% of adults & children with rheumatoid arthritis, but it is usually among the last joints involved. Pain, swelling, & limited movement are the most usual findings. In children, damage to the condyle results in mandibular growth disturbance & facial deformity. Ankylosis might follow. X-rays of the temporomandibular joint are usually negative in the early stages but often show late-stage bone destruction, which might result in an anterior open-bite malocclusion. The diagnosis is suggested by temporomandibular joint inflammation associated with polyarthritis & is confirmed by other findings typical of the disease.
Treatment is the same as that of rheumatoid arthritis in other joints. In the acute stage, nonsteroidal anti-inflammatory (NSAID) drugs might be given, & jaw function should be restricted. An oral appliance worn during sleep is frequently helpful. When symptoms subside, mild jaw exercises help prevent greater loss of mandibular movement. Surgery is needed if ankylosis develops but should not be done until the condition is quiescent.
What are the risk factors of arthritis of the temporomandibular joint?
Factors that might increase the risk of developing temporomandibular joint disorders include:
- Various types of arthritis, such as rheumatoid arthritis & osteoarthritis
- Jaw injury
- Long-term (chronic) grinding or clenching of teeth
- Certain connective tissue diseases cause problems that might affect the temporomandibular joint
How to prevent arthritis of the temporomandibular joint?
How can patients decrease the risk for Temporomandibular joint disorder, Some Temporomandibular joint symptoms are caused by factors out of your control, such as the way your bite fits together. However, in some cases, you might be able to reduce the risk of Temporomandibular joint dysfunction by:
- Practicing good posture.
- Wear a night guard, especially if the patient clenches or grinds their teeth.
- Wearing a mouthguard when playing contact sports.
- Practicing relaxation & stress-reduction techniques.
What is the diagnostic procedure for arthritis of the temporomandibular joint?
The diagnosis starts with an orderly & systematic review of the patient’s history and a thorough physical examination. The information thus gained should be combined with preliminary radiographic evidence to formulate a differential diagnosis. Once the clinician has a differential diagnosis, the diagnosis might be confirmed through appropriate imaging studies & necessary clinical lab studies. This entire procedure of completing the different aspects is important for the successful management of these patients.
- Listen to & feel your jaw when you open & close your mouth
- Observe the range of motion in the jaw
- Press on areas around the jaw to identify areas of pain or discomfort
Clinical Laboratory Evaluation and Imaging
In the lab panel, the Erythrocyte sedimentation rate (ESR) is generally used. Normal ESR should be 40 mm/h. Rheumatoid tests are utilized to rule out rheumatoid arthritis. Rheumatoid factor titer should be < 1:40. The elevation in ESR & C reactive protein is indicative of an infectious or inflammatory etiology.
In addition, if radiographs are deemed required, the panoramic evaluation is the imaging of choice because it can be used as a screening tool to evaluate the overall status of the maxillo-mandibular complex (Fig. 2) & to rule out other possible disease processes. temporomandibular joint tomograms might be utilized for showing osseous condylar abnormalities in the clinic. Nevertheless, transcranial projection examination is inferior. Both transpharyngeal & transcranial views are no longer used for the radiographic diagnosis of temporomandibular joint osteoarthritis.
A study comparing the different imaging modalities concluded that for the radiologic diagnosis of osteoarthritis, reliability and marginal sensitivity were inadequate for panoramic radiography, the average for MRI, & close to the threshold for excellent for CT. Using MRI, reliability was very good for diagnosing disc displacements. Cone beam CT, which reproduces multiple images including axial, coronal, & sagittal planes of the joint, provides a comprehensive radiographic inspection of the bony components of the temporomandibular joint.
The following were the most often morphological changes observed: flattening of the anterior surface of the condyle; followed by erosions & irregularities of the joint surfaces; flattening of the articular surface of the temporal eminence, subchondral cysts, osteophytes; & idiopathic condyle resorption. Ultrasonography has been tried because of its lower costs & has shown promising results.
What is the treatment plan for arthritis of the temporomandibular joint?
Once the diagnosis has been established; treatment will be contingent upon the stage of the condition clinical symptomatology, & preexisting risk factors. Treatment of temporomandibular joint osteoarthritis should be directed at suppressing the active inflammatory process, preserving function, preventing further deformity, & relieving pain. Management is largely symptomatic. Studies have shown that nonsurgical management can successfully be used to treat patients with osteoarthritis. Treatment involves physical therapy, pulsed electrical stimulation, pharmacological, topical ointments, supplements, steroid injections, hyaluronic acid (HA) injections, & acupuncture. Early start of concomitant multimodal therapies offers the best outcome for long-term management.
Non-Pharmacologic
Most of the recommendations for the treatment of temporomandibular joint osteoarthritis are similar to algorithms followed for hip & knee osteoarthritis with certain changes. Recommendations include the usage of education & self-management, regular telephone contact, referral to a physical therapist, muscle strengthening, appliances, thermal modalities, transcutaneous electrical nerve stimulation, & acupuncture. There is moderate-quality evidence that acupuncture, transcutaneous electrical nerve stimulation, & low-level laser therapy decrease pain & that psychoeducational interventions improve psychological outcomes.
Patient education & self-management consist of patient counseling & patient education on the natural course of the disease. Activity modification involves patient instruction on a soft diet, avoiding excessive mouth opening, avoiding gum chewing, & habit modification. The usage of active & passive jaw movement, manual therapy techniques, correction of body posture, & relaxation techniques has also been recommended. Thus a combined approach might be used in patients. Auto-massaging may help in reducing pain & stiffness but might not have any effect on a range of motion.
Eat soft foods. To keep your jaw from working overtime, eat soft foods such as yogurt, mashed potatoes, cottage cheese, soup, scrambled eggs, fish, cooked fruits & vegetables, beans, and grains. Avoid hard & crunchy foods (like hard rolls, pretzels, and raw carrots) & chewy foods (like caramels and taffy). Don’t chew gum.
Wear a splint or night guard. Splints & night guards are mouthpieces that fit over your upper or lower teeth. When worn, the mouthpieces give stable tooth contacts during closure. When worn, mouth guards also correct the bite by placing a jaw in a more favorable position. The main difference between splints & night guards. those night guards are only worn at night and splints are worn full-time. Your healthcare provider can determine which type of oral appliance you might need.
- Avoid extreme jaw movements. For example:
- Keep yawning & chewing to a minimum.
- Don’t rest your chin on your hand or hold the telephone between your shoulder & ear. Practice good posture to reduce neck & facial pain.
- Keep your teeth slightly apart as frequently as you can to relieve pressure on the jaw. To control clenching or grinding during the day, place a tongue on the palate behind the upper front teeth.
- Learn relaxation techniques to control muscle tension in the jaw.
Oral Appliance Therapy
Literature on the usage of appliance therapy to manage osteoarthritis is weak since most of the studies lack the basis of sound clinical research. Certain studies on the usage of appliances for the reduction of painful conditions of the temporomandibular joint have found the resolution of painful symptoms after the insertion of appliances. Others conclude that they are not effective.
Among appliances, joint stabilization appliances are most commonly used & they have been hypothesized to provide joint stabilization, protect teeth, redistribute forces, relax elevator muscles, reduce bruxism decrease joint loading, & might secondarily stabilize occlusion, and cause masticatory muscle relaxation. In certain specific instances, an anterior repositioning appliance might be beneficial. The benefits of splint therapy might be further enhanced in combination with pharmacotherapy. In general, in carefully selected instances with an accurate diagnosis, patients report symptomatic relief of pain with the usage of intra-oral appliances. Therefore, intraoral appliance therapy can’t be ruled out for patients with temporomandibular joint arthropathies.
Irreversible Oral Rehabilitation
temporomandibular joint Osteoarthritis progresses through phases & finally reaches a burnout phase. Long-term follow-up of patients treated with conservative reversible procedures has shown the best results. Dental procedures such as orthodontic treatment, full mouth rehabilitation, & fixed partial dentures should be avoided in the active phase of the disease. In the active phase of the disease, reversible procedures & stabilization procedures must be carried out to offer the best results.
Pharmacological treatment for arthritis of the temporomandibular joint:
Pharmacological management is generally based on side effects, safety, patient acceptance, medical complexity, cost, & routes of intake. Pharmacological modalities of treatment include acetaminophen, cyclooxygenase-2 (COX-2) non-selective & selective oral non-steroidal anti-inflammatory drugs (NSAIDs), topical NSAIDs and capsaicin, intra-articular injections of corticosteroids & hyaluronates, glucosamine & chondroitin sulfate for symptom relief; glucosamine sulfate, chondroitin sulfate and diacerein for possible structure-modifying effects & the use of opioid analgesics for the treatment of refractory pain.
Acetaminophen is one of the oldest & most widely used pharmacological agents for the treatment of osteoarthritis. Although its effectiveness for pain reduction is not as high as NSAIDs it is preferred because of its safety profile & therefore, is commonly used as the first line of treatment. Maximum dosage is up to 4 g/day. It should be used with caution in alcoholics & patients with a history of liver problems.
NSAIDs are extremely beneficial for treating patients with temporomandibular joint Osteoarthritis as they have a dual effect of reducing pain & reducing inflammation. By decreasing the inflammatory process we automatically slow down the degenerative process. NSAIDs have the propensity to cause gastrointestinal (GI) problems & should be used with caution in patients with peptic ulcers and renal failure. Selective COX-2 inhibitors have a somewhat good GI profile. Nevertheless, most of them were discontinued because of the risk to cause Cerebrovascular accidents. In general, NSAIDs can be utilized with GI prophylaxis (generally proton pump inhibitors).
Two randomized controlled trials indicate that tramadol is an effective and well-tolerated adjunctive therapy. In resistant cases, opioid analgesics can be utilized.
Supplements & Alternate Medicine
Ayurvedic medications have recently been compared to supplements & celecoxib and have shown similar efficacy. However, long-term assessment and monitoring for side effects have to be done.
Supplements
These are perhaps one of the most controversial subjects in the management of Osteoarthritis.
Among supplements, glucosamine & chondroitin have been studied most with conflicting results. A meta-analysis in 2000 concluded that it might show some effects. Glucosaminoglycan polysulfate & chondroitin sulfate have been suggested to have chondroprotective effects. Glucosamine in combination with hyaluronate reduced pain & improved joint function in one study. Nevertheless, another study concluded that it had no effect in comparison to the placebo. Other supplements that have been studied include vitamin D supplements & a recent study concluded that it might not have any effect. The results of various studies have to be dealt with caution & more careful research is warranted in this area.
Topicals
Guidelines proposed by the American Academy of Orthopaedic Surgeons, European League Against Rheumatism, Osteoarthritis Research Society International, & National Institute for Health and Clinical Excellence for patients with mild to moderate osteoarthritis of the knee or hand, especially in instances of insufficient affected joints & history of sensitivity to oral NSAID; topical NSAIDs might be considered before oral therapies. Most of the clinical trials of topical NSAIDs have studied diclofenac & ketoprofen, and these have shown improved safety & tolerability with the efficacy significantly superior to placebo & similar to oral NSAIDs (piroxicam being the exception). Diclofenac sodium topical solution 1.5 % with dimethyl sulfoxide was also found to be beneficial. Topical salicylates & capsaicin have not shown substantial efficacy in clinical trials. In addition, concerns exist about their ability to cause serious adverse events such as unexpected poisonings with salicylates, capsaicin-induced nerve desensitization, and their ability to increase the risk of skin ulcers in diabetic patients because of their autonomic nerve effects. Topical trolamine salicylate might be helpful.
Intraarticular Injections, Arthrocentesis & Viscosupplementation
Intra-articular injection of local anesthetics & corticosteroids has also been suggested following the failure of oral medications. Methylprednisolone and triamcinolone acetonide have been used. A systematic review concluded that lavage of the temporomandibular joint might be slightly more effective than nonsurgical treatment for pain reduction. Nevertheless, this difference is not likely to be clinically relevant. Systemic side effects include allergic reactions, and elevated blood sugar in diabetics, and long-term effects include fat atrophy & cartilage softening.
Viscosupplementation is now gaining popularity. Viscosupplementation is effective in primary & secondary osteoarthritis. Viscosupplementation has analgesic, anti-inflammatory, anabolic, & chondroprotective effects. It is a disease-modifying agent as well as gives pain relief. Arthrocentesis combined with HA injections might be useful in reducing pain & improving function. Controversy presents in the use of low molecular weight or high molecular weight HA.
A study that compared the efficacy of six different treatment protocols providing temporomandibular joint arthrocentesis with or without additional drugs concluded that there was no significant difference regarding outcome with the different treatment protocols & different molecular weight HA: however, the five-session low molecular weight HA was slightly better.
A systematic review of the use of HA injections suggests that since the superiority of HA injections has been shown only against placebo saline injections, their efficacy compared to other therapeutic modalities is inconclusive, & the outcomes might be comparable with those achieved with corticosteroid injections or oral appliances. Hence, this approach should be used in select cases with the failure of conservative techniques.
Surgical treatment for arthritis of the temporomandibular joint:
Surgical procedures should be considered only when conservative modalities fail. The different surgical interventions include arthroplasty procedures such as condylotomy, autogenous disc replacement, & total joint replacement procedures.
Arthrocentesis. Arthrocentesis is a minimally invasive procedure that includes the insertion of small needles into the joint so that fluid can be irrigated through the joint to remove debris & inflammatory byproducts.
Injections. In some patients, corticosteroid injections into the joint might be helpful. Infrequently, injecting botulinum toxin type A (Botox, others) into the jaw muscles used for chewing might relieves pain associated with temporomandibular joint disorders.
temporomandibular joint arthroscopy. In some cases, arthroscopic surgery can be as effective for treating various types of temporomandibular joint disorders as open-joint surgery. A small thin tube (cannula) is placed into the joint space, an arthroscope is then inserted & small surgical instruments are used for surgery. temporomandibular joint arthroscopy has fewer risks & complications than open-joint surgery, but it has some limitations as well.
Modified condylotomy. Modified condylotomy addresses the temporomandibular joint indirectly, with surgery on the mandible, but not on the joint itself. It might be helpful for the treatment of pain and if locking is experienced.
Open-joint surgery. If jaw pain does not resolve with more-conservative treatments & it appears to be caused by a structural problem in the joint, your doctor or dentist might suggest open-joint surgery (arthrotomy) to repair or replace the joint. Nevertheless, open-joint surgery involves more risks than other procedures do & should be considered very carefully, after discussing the pros & cons.
If the doctor recommends surgery or other procedures, be sure to discuss the potential benefits & risks, and ask what all your options are.
Physiotherapy treatment for arthritis of the temporomandibular joint:
Temporomandibular disorders are recurring, but self-limiting condition that tends not to be progressive. Non-invasive, conservative management has been found to be effective. Physiotherapy treatment is very effective in relieving & managing Temporomandibular disorders, even when the symptoms are long-standing & severe. With appropriate physiotherapy, most patients will see a significant improvement in the symptoms within 3 to 6 weeks.
Treatment requires addressing the issues identified in the assessment.
If the patient’s symptoms are acute & inflammatory then their condition is likely to be irritable & one should proceed very gently with the goal of first relieving pain, swelling, and muscle spasms. When the pain starts to settle then start to restore jaw movement & alignment. Treatment might include soft tissue releases to affected muscles and joint mobilization techniques.
It is also important to treat any associated neck pain & headaches. Posture correction is essential and should address head, neck, shoulder, & tongue position. The patient should be taught exercises to improve coordination, stability, & alignment of the jaw.
If the patient has signs of sleep bruxism then should discuss with their dentist whether an occlusal splint would be appropriate for them. Occlusal splints hold the temporomandibular joint slightly apart as the patient clenches or grinds, preventing compression of the temporomandibular joint. This can help to relax jaw muscles and reduce swelling & inflammation. There is some evidence supporting the use of splints to reduce long-term degeneration of the temporomandibular joint, disc, and teeth.
Other dental problems, such as cavities, that are causing pain or uneven chewing, lack of dental height, or missing teeth might also need to be addressed.
The patient should be taught strategies to help them manage their disease. This might include posture education, the long-term continuance of their home exercise program, good sleep habits including sleeping positions, stress management, and diet modification – a soft food diet while the condition is acute can help to reduce the pain & swelling more quickly. The patient should also be taught ways to reduce stress on the temporomandibular joint by avoiding activities such as resting the chin on the hand, pencil chewing, jaw clenching while awake, wide-mouth yawning, and nail-biting. They should avoid chewy foods, chewing gum, eating foods that need a wide opening like large hamburgers, & chewing hard foods such as nuts & apples. A case report suggests early post-operative exercises after temporomandibular joint ankylosis in pediatric patients along with a stringent follow-up to prevent post-operative shrinkage & adhesions.
Manual Therapy
A systematic review was published in 2015 to summarize the effectiveness of manual therapy on signs & symptoms of Temporomandibular disorders. It showed that protocols of mixed manual therapy techniques, upper cervical mobilization, or manipulation, had considerable evidence for Temporomandibular disorders symptom control & improvement in maximum mouth opening. The manual techniques included the intra-oral myofascial release & massage therapy on masticatory muscles, atlantooccipital joint thrust manipulation, & upper cervical spine mobilization.
Therapists should be trained, and follow the guidelines & standard procedures to perform cervical thrust manipulation if it is indicated.
The results of the recent clinical trial indicate that both methods, post-isometric muscle relaxation and myofascial release can be used as effective forms of supportive therapy in the prosthetic treatment of pain-related Temporomandibular disorders, accompanied by increased masticatory muscle tension.
Apply moist heat or cold packs. Apply an ice pack to the side of the face & temple area for about 10 minutes for acute pain. Do a few simple stretching exercises for the jaw (as instructed by your healthcare provider). After exercising, apply a warm towel or washcloth to the side of the face for about five minutes. Do that for few times every day.
- Transcutaneous electrical nerve stimulation (TENS). This therapy uses low-level electrical currents to decrease pain by relaxing jaw joints & facial muscles. TENS can be completed at home or at the healthcare provider’s office.
- Ultrasound. This is a deep heat treatment that is applied to the temporomandibular joint to relieve soreness or improve joint movement.
- Trigger-point injections. Medicines for pain or anesthetic are injected into tender muscles of the face to relieve pain.
- Radio wave therapy. Radio waves make a low-level electrical stimulation to the joint, which increases blood flow and provides temporomandibular joint relief.
- Botulinum Toxin (Botox). These injections help decrease muscle mass & inflammation.
Are there alternative temporomandibular joint treatments available?
Many healthcare providers suggest using alternative therapies in combination with traditional treatments. These therapies might include:
- Relaxation techniques. Mindfulness or meditation can help patients slow their breathing & relax tense muscles. As an outcome, pain can be reduced.
- Acupuncture. This technique includes inserting thin needles into the body at various points. Acupressure points might trigger the central nervous system & stimulate your body’s natural healing processes.
- Biofeedback. Electronic modalities can be used to detect areas of stress & tightness in your body. This gives the patient a greater awareness of where they’re holding tension so can focus on relaxing these muscles.
- Pain management referrals. In some cases, the patient might be referred to a pain psychologist or pain management clinic to help ease the symptoms.
Do any self-care measures help arthritis of the temporomandibular joint?
If your jaw pain isn’t too severe & isn’t interfering with your day-to-day life, you might want to try easing the jaw discomfort with self-care measures.
Some options include:
- Resting the jaw. Avoiding opening your jaw wide & trying to stick to eating softer foods that you don’t have to chew too much might provide relief.
- Ice or heat therapy. Applying a cold compress can ease inflammation, while a heating pad or hot water bottle might help relax your jaw muscles.
- Jaw exercises. Doing specific jaw exercises might help to strengthen your jaw muscles & improve the movement of your jaw joints.
- Relaxation exercises. If you clench the jaw when a patient is stressed, relaxation exercises might help you feel calmer & less tense.
- Massaging your jaw muscles. Massaging your jaw muscles might help to improve blood flow & speed up healing.
- Wear a mouthguard at night. If a patient is prone to grinding her teeth when you sleep, a mouthguard might help prevent this.
FAQ (frequently asked questions)
The temporomandibular joint isn’t life-threatening, but if it’s not treated, it can cause pretty persistent discomfort & tension in and around your jaw. It’s also possible that the affected joints could become inflamed, & there might even be damage to your teeth.
temporomandibular joint Disorders Can Be Both Medical & Dental Problems
Arthritis is another medical condition that can lead to a temporomandibular joint disorder. Nevertheless, temporomandibular joint disorders can also be dental problems by nature, especially when it is caused by an underlying problem with a person’s teeth.
Temporomandibular disorders are a group of more than 30 conditions that cause pain & dysfunction in the jaw joint and muscles that control jaw movement. Temporomandibular disorders refer to the disorders, and “TMJ” refers only to the temporomandibular joint itself. People have 2 temporomandibular joints; one on each side of the jaw.
The temporomandibular joint (TMJ) is well-innervated by branches of the trigeminal nerve. Temporomandibular joint disorders (TMD) can cause neural inflammation in the peripheral nervous system (PNS) at the site of injury, or compression, & might have systemic effects on the central nervous system (CNS).
Clenching & grinding of teeth is two of the major causes of temporomandibular joint pain. Nevertheless, this is not an irreversible condition, & with proper treatment, one might be able to cure temporomandibular joint pain permanently. For starters, the patient must stop any habits of teeth grinding or clenching, & anything that puts pressure on the joint.
“Osteoarthritis is the very usual type of arthritis that affects the temporomandibular joint.” Some people might be more at risk for arthritis in the jaw than others. “Macro or microtrauma, through grinding or clenching, along with reduced lubrication in the joint might increase the risk for developing arthritis.”