Gastrocnemius strain: Cause, Symptoms, Treatment, Exercise
Table of Contents
What is a gastrocnemius strain?
A gastrocnemius strain, also sometimes called “tennis leg”, is an injury to the calf muscle in the back of the leg. It occurs when the gastrocnemius muscle is stretched too far resulting in a partial or total tear or rupture within the muscle. Tennis Leg refers to an acute medial head of the gastrocnemius muscle tear in the older athlete characterized by sudden onset of very severe calf pain and significant disability.
The injury is invariably associated with extensive bruising & swelling, & can be mistaken for a deep venous thrombosis. The more common site is the medial head of gastrocnemius, but occasionally the plantaris muscle is involved. Symptoms are a sudden, sharp or burning pain in the leg, many time accompanied by an audible sound. In more cases, the player is unable to resume play because of the severe pain. Depending on the severity of the injury, recovery may take between a few days & 6 weeks.
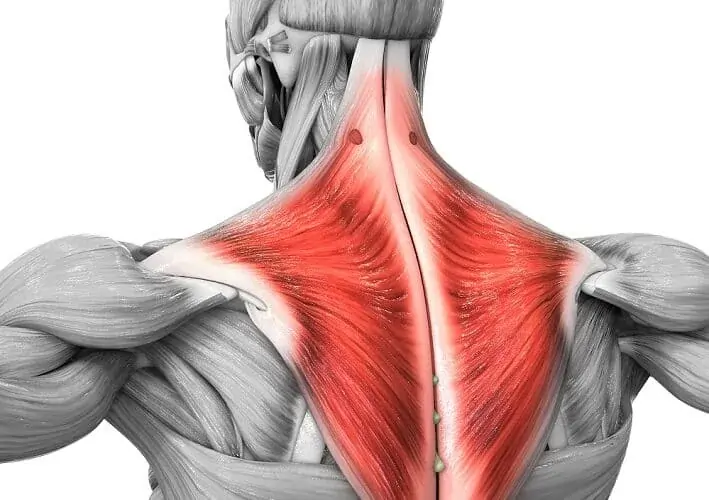
Anatomy of gastrocnemous muscle
The gastrocnemius is a superficial two-headed muscle. It runs from two heads just above the knee to the heel, it is a three joint muscle (knee, ankle, and subtalar joints). This muscle is just under the skin at the reverse of the lower leg. Because the gastrocnemius is close to the skin’s face, It forms the bulk of the shin muscle.
It is a large muscle located in the posterior leg. Posteriorly, it is the most superficial muscles of the leg, and forms the bulk of the calf muscle group. Gastrocnemius muscle with soleus and plantaris muscle which are the part of calf muscle also called Triceps Surae.
Origin: proximal to body part surfaces of aspect condyle of the leg bone and medial condyle of the femur
Insertion: tendo calcaneus (Achilles tendon) into mid-posterior or tarsi fibular
Nerve: tibial nerve from the sciatic, nerve roots S1 – S2
Actions: plantar flexes foot, flexes knee
Antagonist: Tibialis anterior muscles
What causes of Gastrocnemius strain?
- Age/activity status: Medial gastrocnemius occur more commonly in the middle-aged recreational athlete. This population typically resume to be physically active at a average to high intensity but not on a regular basis, and these individuals are also likely to have continue a moderate degree of the muscle mass from their more active days.
- Deconditioned/unstretched muscles: The cold & unstretched muscles that recreational athletes often use to compete with are very likely to rupture when challenged compared with conditioned & stretched muscles.
- Previous injury: The athlete with recurrent gastrocnemius strains is likely to have healed with fibrotic scar tissue, which absorbs forces differently & is thus more likely to result in rupture when the muscle is challenged.
What is Risk Factors of Gastrocnemius strain?
This strain occur commonly in sports activities (e.g, hill running, jumping, tennis), but it can occur in any activity. A medial Gastrocnemius injury is often seen in the irregular active athlete. Medial Gastrocnemius injuries occur most commonly in men than in women,& these injuries usually afflict athletes and others in the 4th to 6th decade of life. Medial Gastrocnemius injuries are more commonly seen acutely, but up to 20% of affected patients report a prodrome of calf tightness several days before the injury, thus suggesting a potential chronic predisposition.
What are the symptoms of gastrocnemius strain?
- An audible pop when the strain to the medial gastrocnemius occurred is usually reported.
- The patient complains of calf pain, which also radiates to the knee or the ankle. In addition, the patient complains of pain with ankle movements.
- The patient complains of a swollen leg that extends down to the foot or ankle, as well as the associated color changes of bruising.
- Tenderness is noted upon palpation in the entire medial gastrocnemius muscle, but this tenderness is observed to be exquisitely more painful at the medial musculotendinous junction.
- Palpation of the Achilles tendon should demonstrate an intact tendon.
- The peripheral pulses should be present and symmetric.
- Moderate to severe pain is demonstrated with passive ankle dorsiflexion (due to stretching of the torn muscle fibers) in tennis leg, as well as with active resistance to ankle plantar flexion (due to the firing of the torn muscle fibers).
How is gastrocnemius strain diagnosed?
Assessment
Subjective assessment
- history with associated symptoms
- mechanism of injury:
- Inciting trauma- side and magnitude of injury force
- recurrent trauma-faulty postural related injuries
Objective assessment
- Examine the foot and ankle in supine and standing position
- Ankle Active range of motion
- Ankle Passive range of motion
- Resisted strength check the ankle and foot
- Knee Active ROM and manual muscle testing
- On objective assessment, there will be:
- muscle Tenderness- to touch at the point of injury
- Swelling
- Bruising may appear within hours or days
- Stretching of the muscle will reproduce pain
- Pain on resisted plantar flexion.
A diagnostic ultrasound imaging test may be ordered to confirm the gastrocnemius tear and to determine the level of the injury. If a deep venous thrombosis is suspected, a Doppler ultrasound or an MRI might also be used.
Grades of gastrocnemius strain:
Grade 1: Grade 1 injury causes minimal muscle damage, although there may be sharp pain at the time of injury. May be able to continue an activity, without pain or with mild discomfort.
Average time to come back to sport:10-12 days
sign-pain on unilateral calf raise.
Grade 2: Grade 2 injuries cause moderate muscle damage, and people with this category of muscle injury may have difficulty walking. They will often experience a sharp pain that worsens when they flex or extend their foot.
Average time to come sport:16-21 damage days
sign-pain with active plantar flexion, pain and weakness with resisted plantar flexion, loss of flexion.
Grade 3: A grade 3 injury is a complete tear of the muscle, and it can cause significant bruising and swelling in the calf.Full recovery can take three to four months and, in some instances, surgery may even be needed.
Average time to come sport: 6 months once surgery
sign-inability to contract calf muscle may have the palpable defect, & Thomson’s test positive
What is a Differential diagnosis?
- Medial leg bone stress syndrome
- Plantar fasciopathy
- Ankle Joint sprain
- Medial leg bone stress syndrome
- Leg injuries related to sports with same symptoms and treatment as a calf strain are mentioned below.
- Chronic exertional compartment syndrome (CECS)
- Achilles tendinopathy
- Popliteal Artery entrapment Syndrome (PAES)
What is the treatment of gastrocnemius strain?
RICE Principle:
R- rest
I- ice for cooling
C- compression: tapping and splinting
E- elevation

Rest: Refused some activities that cause pain, swelling, or discomfort. don’t avoid all physical activity.
Ice: Ice is a tried-and-true tool for decrease pain and swelling. Apply an ice pack (covered with a light, absorbent towel to help prevent frostbite) for 15-20 minutes every 2 to 3 hours during the first 24 to 48 hours after injury.
Compression: This means wrapping the injured part to prevent swelling. Wrap the affected part with an elastic medical bandage. You should to be snug but not too tight.if it’s too tight, it’ll interrupt blood flow. If the skin under the wrap turns blue or feels cold,numb, or tingly, loosen the bandage. If these symptoms don’t disappear right away, seek instantly medical help.
Elevation: Elevate the leg on high of your heart’s extent, importantly at night time, that allows gravity to help reduce swelling.
Medical treatment:
Pain management should include analgesics as indicated. Caution should be used with non steroidal anti-inflammatory drugs (NSAIDs) during the acute injury phase, as these agents can predispose the patient to increased bleeding and hematoma formation in the initial days after an injury. Theoretically, cyclooxygenase-2 (COX-2) inhibitors may provide pain control without the risk of bleeding in acute injuries, which is a concern with conventional NSAIDs.
Ankle/foot bracing should be used to keep the ankle in a position of maximal tolerable dorsiflexion. Studies have shown an increased rate of healing with this intervention.
Physiotherapy Treatment and Exercise for gastrocnemius strain
The goal of physiotherapy treatment are:
- Relieve gastrocnemius muscle pain
- Reduce muscle swelling
- Increases gastrocnemius muscle strengths.
- restore patient’s confidence
- restore patients’ full functional activities
- increase full mobility of the ligament and corresponding joint
Electrotherapy
physiotherapy rehabilitation can be begin after 48 hours of injury, For the first few days give electric modality give to reduce swelling and pain
Ultrasound
ultrasound has been used about tissue healing increases blood circulation and mobility & reduce swelling.
Cryotherapy
Inflammation and swelling can be decrease by applying cryotherapy in form of ice packs, and cold water baths to the affected part. Constant application of cold several times a day for 15-30 minutes at a time is suggest.
TENS
Trans cutaneous electrical nerve stimulation (TENS) may be able to help decrease pain and muscle spasms.
Massage
- When in the gastrocnemius muscle pain presents to tender & trigger points in the physiotherapy treatment therapist is advised to massage the area of muscle pain.
- It is applied with the help of oil & powder for 5 to 10 minutes to the area of muscle pain.
- Effleurage massage is mostly help to relive muscle pain.
- It is applied in a circular motion. It is also applied with the help of a messenger.
Stretching Exercises:
To get the best gastrocnemius stretch, the knee must be extended while the ankle is dorsiflexed.

Patient position and procedure:
Long-sitting or with the knees a certain degree flexed.
teach the patient to strongly dorsiflex the feet, attempting to keep the toes relaxed.
Long-sitting and with a towel or belt wind under the forefoot.
teach the patient to pull with equal force on both ends of the towel to move the foot into dorsiflexion
Patient position and procedure:
In standing teach the patient to stride forward with one foot, keeping the heel of the back foot flat on the floor. Have the patient brace his or her hands against a wall if necessary. To provide stability to the foot, the patient certain degree rotates the back leg inward so the foot presumes a supinated position and locks the joints. The patient then moves body weight forward onto the front foot. To stretch the gastrocnemius muscle, the knee of the back leg is retained extended.
Exercise:
All exercise helps you release pain & weakness.
- Calf raises
- Standing heel calf raise
- Squat with gastrocnemius raise
- Donkey calf raise
Calf raises :
- The patient is in a Standing position straight, then push through the balls of the feet & raise the heel till you are standing on the toes. Then lower to slowly back to the start.
- Do this exercise 10 times in 1 session & 3 sessions per day.

Calf raise variations :
- Weighted calf raise:
- It is a good idea to increase the difficulty of the calf raises with the weights with the exercise.
- The patient is Holding a dumbbell in each hand while doing the calf raises which is help to prepare the calf muscle to handle the put extra pressure during the exercise.
- Do this exercise 10 times in 1 session & 3 sessions per day.
- Raised calf raise:
- You are in the Standing position on a step so that your heel is dropping lower than the rest of the foot at the bottom of the movement. Then provides a greater range of motion in the calf muscle during the exercise.
- You can hold the dumbbells to make this variation tougher, but it is difficult to must keep the balance when holding the dumbbells too heavy.
- Do this exercise 10 times in 1 session & 3 sessions per day.
- Bent-knee calf raise:
- When Bending the knee joint slightly when doing any kind of calf raises which is mostly used for soleus muscle.
- During the bent knee position do the calf raise exercise.
- Do this exercise 10 times in 1 session & 3 sessions per day.
- Seated calf raise:
- You are in a sitting position on a chair with the feet on a raised surface so that heels are hanging off the back.
- With the latter, you can rest dumbbells on the knee joint to add resistance to the movement.
- Seated calf raises are mostly good for working the soleus muscles & allow to you add significant weight to the exercise with less risk of losing the balance.
- Do this exercise 10 times in 1 session & 3 sessions per day.
- Standing heel calf raise:
- This exercise starts with the standing position and then holding onto a stable surface for support.
- Then Slowly raise the heels off the ground as far as you can & lower them back to the floor
- You are Make sure to keep the balls of the feet on the ground & maintain the balance.
- Then Repeat this exercise 10 times in 1 session & 3 sessions per day.

Foam Roller Exercise:
- You are in a sitting position on the floor with your legs extended in front of you.
- Then place the roller under the calves.
- Use the hands for support then slowly roll from the knee joint down to the ankle & pausing on any tight or sore spots.
- Do this roll for 30 seconds to 1 minute & repeat 5 times in 1 session & 3 sessions per day.
Squat with gastrocnemius raise :
- You are Holding a squat rack with both hands an upright torso & feet hip-width apart & toes pointed forward.
- You can also hook a band to a pole & sturdy object to wrap it around the waist so that you can lean back safely.
- It allows you to must keep the shins perpendicular to the floor when squatting down.
- Must be Keep the shoulder down & chest up perform a squat till the thighs are parallel with the ground.
- Then Perform a calf raise by the raising up onto the toes.
- Hold for 30 seconds & return to heel to the ground.
- Then Stand up from the squat & reset.
- Repeat this exercise 10 times in 1 session & 3 sessions per day.

Donkey calf raise :
- You are Set up in the donkey calf raise machine by securing the hands hinge back at the hip joint & placing the balls of the feet at the far edge of the step.
- Bend the knee joint as much as tolerated.
- Then lower the heels as far as possible to the floor & hold for 30 seconds.
- Then lift the heels as far as possible & squeezing the calves at the top.
- Repeat this exercise 10 times in 1 session & 3 sessions per day.
Strengthening exercise:
Strengthening exercise is help to you for release the muscle weakness & strengthen the muscle.
- Strengthening exercise for gastrocnemius muscle
- Single-Leg Calf Raises With Bent Knee On A Step
- Seated gastrocnemius raise with weight
Strengthening exercise for gastrocnemius muscle :
- You are standing with the feet are shoulder-width apart.
- Then Raise the heels to the count of 2 & lower them to the count of 4.
- Make sure to you are on the tips of your toes.
- Use a chair & wall for support if you need it.
- Do the 10 to 20 repetitions of 2 to 3 sets daily.
- To make this exercise harder, try doing this exercise on one leg.
Single-Leg Calf Raises With Bent Knee On A Step:

- You are standing on a step with the heels hanging off the edge.
- Hold the something for stability
- Then Stand on the leg you want to for exercise & bend the knee joint to as close the 90 degrees as you can.
- Next, raise onto the toes & slowly lower back down till you get a stretch in the calf muscle & repeat.
- If you are ready for this exercise more times then add weight to the hand.
- Then Choose a resistance that is high for strengthening & low for endurance.
- Perform this exercise for 6- 10 repetitions &repeat this exercise for 3-5 sets in total for strength.
- For endurance, you do this exercise for 15-25 repetitions & repeat for 3-5 sets.
- You need to rest at least 3 minutes between the sets for strength & no more than 30 seconds for endurance.
- You must be taken to aim the work either 2 to 3 times per session per week.
Seated gastrocnemius raises with weight:
This exercise is performed in the 3 versions like as isometric, eccentric, and concentric.
- An isometric version of this exercise :
- This exercise involves holding this right foot tiptoe position for up to 30 seconds.
- Then the weight needs to be heavy enough to allow no more than 30 seconds.
- Once you feel stronger from this exercise & do this exercise over 30 seconds then you will add more weight.
- An eccentric version of this exercise :
- This exercise involves holding this right foot tiptoe position for 2 seconds.
- Then slowly lowering the heel back down over the edge of the step for 3 seconds.
- Repeat this movement by using the two feet to lift the weight, one foot to hold & lower, and so on.
- The weight needs to be heavy enough to allow no more than 12 repetitions.
- Once you feel stronger for this exercise & do the 12 repetitions & you add more weight.
- A concentric version of this exercise:
- In exercise involves using just one foot to lift & lower the weight.
- Must be Keep the tempo slow & controlled & use enough the weight to allow no more than 12 repetitions.
- Once you feel stronger for this exercise & do the 12 repetitions & you add more weight.
Preventive measures:
Prepare: The best way to prevent tennis leg and muscle strains is to sufficiently warm-up prior to the playing. I know no one likes to give the time to warm-up, but it is critical for injury prevention. Get to the court early to perform dynamic warm-up. A 5-7 minutes dynamic warm-up is perfect within 15 minutes of match time. This includes movements to help lengthen muscles to prepare for tennis and increases your heart rate and body temperature so body is warm, which may help decrease risk for injury. Once you compete dynamic warm-up, grab racket and start hitting.
Recover: Immediately following match, stay on the court to stretch arms and legs. They just did a lot of work so help the muscle cool down so aren’t stiff or sore the next day. Stretching helps maintain flexibility and joint mobility. Hold each stretch for about 30 seconds. A few of stretches are best done on the floor, so it is ideal to throw a yoga mat down and finish stretching in the club house or locker room. Cool-down stretching might be done within 30 minutes of coming off the court, so do this prior to shower & change clothes.
Roll it out: Foam rolling is a great way to stretch and massage muscles and fascia after you play.The combining this with stretching. Roll all muscle for about 30 seconds.
Repair: At the last of day, take a warm bath with 1-2 cups of Epsom salts for about 15 minutes. The magnesium sulfate in the Epsom salts is soothing for sore, tight and tired muscles & diminishes pain & muscle tension promoting more restful sleep. So, take bath prior to bedtime.
Protect: If you have expertise a calf muscle strain or Tennis leg, consider applying a compression sleeve around the lower leg. During the cool weather months, adapt clothing to the weather conditions. It may be benefit to wear pants, running tights, or compression gear to keep legs warm. Well-warmed muscles are better able to withstand pulling & traction forces than cold muscles.
Cross train: Cycling, running, Pilates & yoga as great ways to cross train for tennis, which build strength & flexibility and will help reduce risk of muscle trains & tears.





2 Comments