ULTRASOUND THERAPY
Table of Contents
Introduction of Ultrasound :
- Use of Sound-wawe in Physiotherapy Have Physiological Healing And Pain Relieving Effects is known as a Ultrasound Therapy.
- Ultrasound (US) is a form of mechanical energy (not electrical), and therefore, strictly speaking, not really electrotherapy at all, but does fall into the Electro Physical Agents grouping. Mechanical vibration at increasing frequencies is known as sound energy.
- The normal human sound range is from 16 Hz to something approaching 15-20,000 Hz (in children and young adults). Beyond this upper limit, the mechanical vibration is known as ultrasound. The frequencies used in therapy are typically between 1.0 and 3.0 MHz.
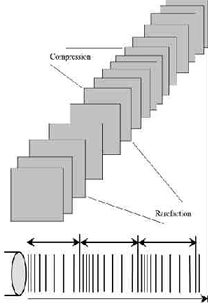
- Sound waves are longitudinal waves consisting of areas of compression and rarefaction. Particles of a material, when exposed to a sound wave will oscillate about a fixed point rather than move with the wave itself. As the energy within the sound wave is passed to the material, it will cause oscillation of the particles of that material.
- Clearly any increase in the molecular vibration in the tissue can result in heat generation, and ultrasound can be used to produce thermal changes in the tissues, though current usage in therapy does not focus on this phenomenon. In addition to thermal changes, the vibration of the tissues appears to have effects which are generally considered to be non thermal in nature, though, as with other modalities (e.g. Pulsed Shortwave) there must be a thermal component however small.
- As the Ultrasound wave passes through a material (the tissues), the energy levels within the wave will diminish as energy is transferred to the material. The energy absorption and attenuation characteristics of US waves have been documented for different tissues.
Ultrasound Waves :
Ultrasound waveform with compression and rarefaction
- FREQUENCY – the number of times a particle experiences a complete compression/rarefaction cycle in 1 second. Typically 1 or 3 MHz.
- WAVELENGTH – the distance between two equivalent points on the waveform in the particular medium. In an ‘average tissue’ the wavelength 1MHz would be 1.5mm and 3 MHz would be 0.5 mm.
- VELOCITY – the velocity at which the wave (disturbance) travels through the medium. In a saline solution, the velocity of US is approximately 1500 m sec-1 compared with approximately 350 m sec-1 in air (sound waves can travel more rapidly in a more dense medium). The velocity of US in most tissues is thought to be similar to that in saline.
These three factors are related, but are not constant for all types of tissue. Average figures are most commonly used to represent the passage of US in the tissues.
Typical US frequencies from therapeutic equipment are 1 and 3 MHz though some machines produce additional frequencies (e.g. 0.75 and 1.5 MHz) and the ‘Longwave’ ultrasound devices operate at several 10’s of kHz (typically 40-50,000Hz – a much lower frequency than ‘traditional US’ but still beyond human hearing range.
The mathematical representation of the relationship is V = F.l where V = velocity, F = frequency and l is the wavelength.
Ultrasound Waveform
The Ultrasound beam is not uniform and changes in its nature with distance from the transducer. The US beam nearest the treatment head is called the NEAR field, the INTERFERENCE field or the Frenzel zone. The behaviour of the US in this field is far from regular, with areas of significant interference.
The US energy in parts of this field can be many times greater than the output set on the machine (possibly as much as 12 to 15 times greater). The size (length) of the near field can be calculated using r2/l where r= the radius of the transducer crystal and l = the US wavelength according to the frequency being used (0.5mm for 3MHz and 1.5mm for 1.0 MHz).
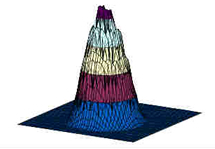
As an example, a crystal with a diameter of 25mm operating at 1 MHz will have a near field/far field boundary at : Boundary = 12.5mm2/1.5mm » 10cm thus the near field (with greatest interference) extends for approximately 10 cm from the treatment head when using a large treatment head and 1 MHz USus beam. When using higher frequency US, the boundary distance is even greater.
Beyond this boundary lies the Far Field or the Fraunhofer zone. The US beam in this field is more uniform and gently divergent. The ‘hot spots’ noted in the near field are not significant. For the purposes of therapeutic applications, the far field is effectively out of reach.
One quality indicator for US applicators (transducers) is a value attributed to the Beam Nonuniformity Ratio (BNR). This gives an indication of this near field interference. It describes numerically the ratio of the intensity peaks to the mean intensity. For most applicators, the BNR would be approximately 4 – 6 (i.e. that the peak intensity will be 4 or 6 times greater than the mean intensity). Because of the nature of US, the theoretical best value for the BNR is thought to be around 4.0 though some manufacturers claim to have overcome this limit and effectively reduced the BNR of their generators to 1.0.
Effect of ultrasound
~The ultrasound waves are generated by a piezoelectric effect caused by the vibration of crystals within the head of the probe. The ultrasound waves that pass through the skin cause a vibration of the local soft tissues. This vibration or cavitation can cause a deep heating locally though usually no sensation of heat will be felt by the patient. In situations where a heating effect is not desirable, such as a fresh injury with acute inflammation, the ultrasound can be pulsed rather than continuously transmitted.
How Ultrasound Transmitted through the Tissues?
All materials (tissues) will present an impedance to the passage of sound waves. The specific impedance of a tissue will be determined by its density and elasticity. In order for the maximal transmission of energy from one medium to another, the impedance of the two media needs to be as similar as possible. Clearly in the case of US passing from the generator to the tissues and then through the different tissue types, this can not actually be achieved.
The greater the difference in impedance at a boundary, the greater the reflection that will occur, and therefore, the smaller the amount of energy that will be transferred. Examples of impedance values can be found in the literature.
The difference in impedance is greatest for the steel/air interface which is the first one that the US has to overcome in order to reach the tissues. To minimize this difference, a suitable coupling medium has to be utilised. If even a small air gap exists between the transducer and the skin the proportion of US that will be reflected approaches 99.998% which means that there will be no effective transmission.

- Transmission through a coupling medium
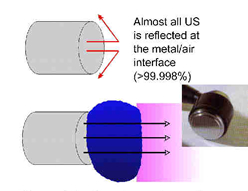
The coupling media used in this context include water, various oils, creams and gels. Ideally, the coupling medium should be fluid so as to fill all available spaces, relatively viscous so that it stays in place, have an impedance appropriate to the media it connects, and should allow transmission of US with minimal absorption, attenuation or disturbance. For a good discussion regarding coupling media.
At the present time the gel based media appear to be preferable to the oils and creams. Water is a good media and can be used as an alternative but clearly it fails to meet the above criteria in terms of its viscosity. There is no realistic (clinical) difference between the gels in common clinical use. The addition of active agents (e.g. anti-inflammatory drugs) to the gel is widely practiced, but remains incompletely researched. We are currently evaluating this intervention further
- Absorption and Attenuation
Exponential energy absorption in a medium
The absorption of US energy follows an exponential pattern – i.e. more energy is absorbed in the superficial tissues than in the deep tissues. In order for energy to have an effect it must be absorbed, and at some point this must be considered in relation to the US dosages applied to achieve certain effects.
Because the absorption (penetration) is exponential, there is (in theory) no point at which all the energy has been absorbed, but there is certainly a point at which the US energy levels are not sufficient to produce a therapeutic effect. As the US beam penetrates further into the tissues, a greater proportion of the energy will have been absorbed and therefore there is less energy available to achieve therapeutic effects. The half value depth is often quoted in relation to US and it represents the depth in the tissues at which half the surface energy is available. These will be different for each tissue and also for different US frequencies.
The table gives some indication of typical (or average) half value depths for therapeutic ultrasound. As it is difficult, if not impossible to know the thickness of each of these layers in an individual patient, average half value depths are employed for each frequency: 3MHz – 2.0cm; 1MHz – 4.0cm.
1 MHZ 3MHz
muscles 9.0mm 3.0mm
fat 50.0mm 16.5mm
tendon 6.2mm 2.0mm - To achieve a particular US intensity at depth, account must be taken of the proportion of energy which has been absorbed by the tissues in the more superficial layers. The table gives an approximate reduction in energy levels with typical tissues at two commonly used frequencies, and more detailed information is found in the dose calculation material
Depth (cm) 3MHz 1MHz
2 50%
4 25% 50%
8 25%F
- As the penetration (or transmission) of US is not the same in each tissue type, it is clear that some tissues are capable of greater absorption of US than others. Generally, the tissues with the higher protein content will absorb US to a greater extent, thus tissues with high water content and low protein content absorb little of the US energy (e.g. blood and fat) whilst those with a lower water con6:51 AM 11/22/2019 tent and a higher protein content will absorb US far more efficiently. Tissues can be ranked according to their relative tissue absorption and this is critical in terms of clinical decision making.
Pulsed Ultrasound :
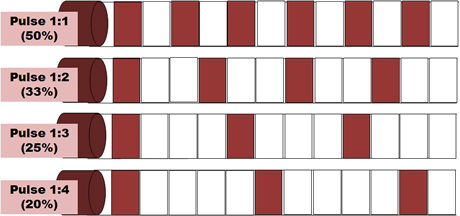
- Most machines offer the facility for pulsed US output, and for many clinicians, this is a preferable mode of treatment. Until recently, the pulse duration (the time during which the machine is on) was almost exclusively 2ms (2 thousandths of a second) with a variable off period. Some machines now offer a variable on time though whether this is of clinical significance has yet to be determined. Typical pulse ratios are 1:1 and 1:4 though others are available (see dose calculations). In 1:1 mode, the machine offers an output for 2ms followed by 2ms rest. In 1:4 mode, the 2ms output is followed by an 8ms rest period. The adjacent diagram illustrates the effect of varying the pulse ratio.
- The effects of pulsed US are well documented and this type of output is preferable especially in the treatment of the more acute lesions. Some machines offer pulse parameters that do not appear to be supported from the literature (e.g. 1:9; 1:20). Some manufacturers describe their pulsing in terms of a percentage rather than a ratio (1:1 = 50% 1:4 = 20% etc). The proportion of time that the machine is ON compared with OFF is a relevant factor in dosage calculations and further details are included in the dose calculation support material.
*Therapeutic Ultrasound & Tissue Healing
One of the therapeutic effects for which ultrasound has been used is in relation to tissue healing. It is suggested that the application of US to injured tissues will, amongst other things, speed the rate of healing & enhance the quality of the repair. The following information is intended to provide a summary of some of the essential research in this field together with some possible mechanisms through which US treatments `may achieve these changes. It is not intended to be a complete explanation of these phenomena or a comprehensive review of the current literature. It may, none the less, provide some useful basic information for clinical application.
The therapeutic effects of US are generally divided into:
THERMAL & NON-THERMAL.
Thermal Effects of US :
In thermal mode, US will be most effective in heating the dense collagenous tissues and will require a relatively high intensity, preferably in continuous mode to achieve this effect.
Many papers have concentrated on the thermal effectiveness of ultrasound, and much as it can be used effectively in this way when an appropriate dose is selected (continuous mode >0.5 W cm-2), the focus of this paper will be on the non thermal effects. Both Nussbaum and ter Haar[3] have provided some useful review material with regards the thermal effects of ultrasound.
Comparative studies on the thermal effects of ultrasound have been reported by several authors with some interesting, and potentially useful results. Further work continues in our research centre with a comparison of contact heating and longwave ultrasound and comparison of different US regiemes combined with US (Aldridge and Watson – in preparation).
It is too simplistic to assume that with a particular treatment application there will either be thermal or non thermal effects. It is almost inevitable that both will occur, but it is furthermore reasonable to argue that the dominant effect will be influenced by treatment parameters, especially the mode of application i.e. pulsed or continuous. Baker et al. have argued the scientific basis for this issue coherently.
Lehmann suggests that the desirable effects of therapeutic heat can be produced by US. It can be used to selectively raise the temperature of particular tissues due to its mode of action. Among the more effectively heated tissues are periosteum, collagenous tissues (ligament, tendon & fascia) & fibrotic muscle.
If the temperature of the damaged tissues is raised to 40-45°C, then a hyperaemia will result, the effect of which will be therapeutic. In addition, temperatures in this range are also thought to help in initiating the resolution of chronic inflammatory states. Most authorities currently attribute a greater importance to the non-thermal effects of US as a result of several investigative trials in the last 15 years or so.
Non-Thermal Of US :
The non-thermal effects of US are now attributed primarily to a combination of CAVITATION and ACOUSTIC STREAMING. There appears to be little by way of convincing evidence to support the notion of MICROMASSAGE though it does sound rather appealing.

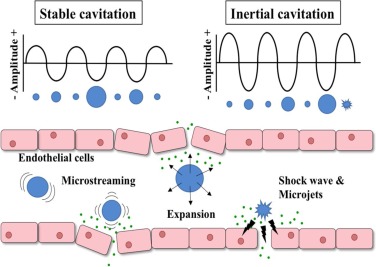
EFFECT OF CAVITATION
its simplest sense relates to the formation of gas filled voids within the tissues & body fluids. There are 2 types of cavitation – STABLE & UNSTABLE which have very different effects.
- STABLE CAVITATION does seem to occur at therapeutic doses of US. This is the formation & growth of gas bubbles by accumulation of dissolved gas in the medium. They take apx. 1000 cycles to reach their maximum size. The `cavity’ acts to enhance the acoustic streaming phenomena (see below) & as such would appear to be beneficial.
- UNSTABLE (TRANSIENT) CAVITATION is the formation of bubbles at the low pressure part of the US cycle. These bubbles then collapse very quickly releasing a large amount of energy which is detrimental to tissue viability. There is no evidence at present to suggest that this phenomenon occurs at therapeutic levels if a good technique is used. There are applications of US that deliberately employ the unstable cavitation effect (High Intensity Focussed Ultrasound or HIFU) but it is beyond the remit of this
EFFECT OF ULTRASOUND
ACOUSTIC STREAMING
a small scale eddying of fluids near a vibrating structure such as cell membranes & the surface of stable cavitation gas bubble. This phenomenon is known to affect diffusion rates & membrane permeability. Sodium ion permeability is altered resulting in changes in the cell membrane potential. Calcium ion transport is modified which in turn leads to an alteration in the enzyme control mechanisms of various metabolic processes, especially concerning protein synthesis & cellular secretions.
The result of the combined effects of stable cavitation and acoustic streaming is that the cell membrane becomes ‘excited’ (up regulates), thus increasing the activity levels of the whole cell. The US energy acts as a trigger for this process, but it is the increased cellular activity which is in effect responsible for the therapeutic benefits of the modality.
Use of Ultrasound :
- Increases healing rates
- Tissue relaxation
- Tissue heating
- Increase local blood flow
- Scar tissue breakdown.
Effect Of Ultrasound :
- The effect of ultrasound via an increase in local blood flow can be used to help reduce local swelling and chronic inflammation,promote bone fracture healing.Ultrasound can also be used to achieve phonophoresis.
- This is a non-invasive way of administering medications to tissues below the skin; perfect for patients who are uncomfortable with injections.Stimulate the production of collagen (the main protein in tendons and ligaments) during tissue healing.
Which Conditions are treated with the US?
- inflammation(Bursitis or tendonitis)
- chronic pain
- Muscle Strain and tears
- Osteoarthritis
- ligament and tendon injuries
- non-acute joint swelling and muscle spasm.
- Tightness or contractures (to improve range of motion)
- Frozen shoulder
- Wound healing
Which body Parts use for ultrasound therapy?
- Muscle pain.
- Trigger points.
- Soften the surgical scar.
- Softening the tendon after tendon transplant.
- Plantar fascitis.
- Carpal tunnel syndrome.
What is the condition where you need to avoid it?
- Tumor.
- Pregnancy.
- Over the metal implants.
- Knee replacement.
- Hip replacement.
- Pacemaker.
- Eyes.
Contraindications of Ultrasound :
- Directly on open wounds or active infections
- Over metastatic lesions
- On patients with impaired sensation
- Directly on metal implants
- Near a pacemaker or any other device that generates a magnetic field
- During pregnancy (except in the instance of diagnostic sonography)
- Additionally, ultrasound should not be applied over: ~ The eye ~ The gonads ~ Active epiphysis in children.
precautions in Ultrasound Treatment
- Always use the lowest intensity which produces a therapeutic response
- The head of the applicators should be moving throughout the treatment
- The ultrasound beam (treatment head) should be perpendicular to the treatment area for best results.
- All parameters (intensity, duration, and mode) need to be considered carefully for desired therapeutic effects.









38 Comments