Mallet Finger
Table of Contents
What Is The Mallet Finger
Mallet Finger is a finger injury where the tip cannot be straightened due to damage to the extensor tendon. It usually occurs from a sudden impact, such as a ball striking the fingertip.
Common symptoms include pain, swelling, and a drooping fingertip. Treatment often involves splinting the finger in extension for several weeks, though severe cases may require surgery.
The injury can occur when the tip of a finger or thumb is struck by an unyielding (rigid or solid) object, such as a baseball, causing it to bend farther than it should. Because of the damage, you are unable to straighten your thumb or fingertip on your own, which causes the tip of the digit to be bent.
Anatomy
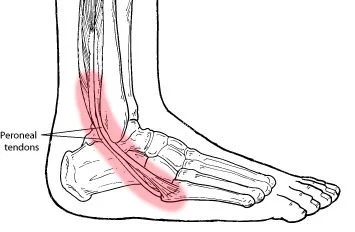
The tissues that join muscles to bones are called tendons. The hand and forearm contain the muscles that move the thumb and fingers. You can move your fingers and thumb thanks to tendon attachments that go from these muscles through the wrist and connect to their little bones.
- The fingers are straightened by the extensor tendons on the top of the hand.
- The fingers are bent by the flexor tendons on the palm side of the hand.
Causes of Mallet Finger
The distal extensor tendon is torn in mallet finger injuries. When a finger is actively extended and its distal phalanx is driven into flexion, as happens in ball sports when a ball strikes the tip of an extended finger, the rupture takes place.
- After starting in the forearm and passing across the metacarpophalangeal joint, the extrinsic extensor tendon indirectly connects to the proximal phalanx before joining the distal phalanx. The digits’ ability to extend is due to these tendons.
- Damage to the extensor tendon results in a mallet finger injury. When a tendon injury results in an avulsion fracture of the distal phalanx, a mallet fracture happens.
- Nonoperative therapies are supported by current research, however, injuries must be treated quickly to prevent negative results.
Signs and symptoms
Following the damage, your finger may hurt and droop at the tip. Your hand will still be functional. When a bone fracture occurs, pain is frequently present.
Additional signs of mallet finger include:
- Redness, swelling, and bruises
- Tenderness
- Unable to straighten your fingers without holding it up with your other hand
Epidemiology
Mallet finger injuries and other terminal extensor tendon injuries are frequent. 5.6% of hand and wrist injuries are caused by injuries to the terminal extensor tendon. Injuries from mallet fingers:
- Usually, it takes place during work or athletic events.
- Are often observed in young to middle-aged men, and they can also be seen in elderly ladies on occasion. Men who sustain a mallet finger injury are 34 years old on average. Women are 41 years old on average.
- It is more prevalent in ball sports because the ball strikes the tip of an outstretched finger. This results in an extensor tendon disruption by forcing the distal interphalangeal joint into a forced flexion posture.
- Lower injury impacts, such as an older person “jamming” their finger while carrying out daily tasks like tucking in bedsheets or putting up socks, can also result in terminal extensor tendon injuries.
- The dominant hand’s ring finger and long or middle finger are the digits most frequently impacted.
Diagnostic Procedures
- Mallet’s finger is often diagnosed during the physical examination.
- An X-ray might be obtained to determine whether the injury is a broken bone, a tendon rupture, or an avulsion fracture.
Treatment of Mallet Finger
To address a mallet finger’s discomfort and swelling right away:
- Put some ice on it.
- Make sure your fingers are over your heart by raising your hand.
- Use NSAIDs or nonsteroidal anti-inflammatory medicines.
Physiotherapy Treatment of Mallet Finger :
- Mallet finger injuries require careful management, and physiotherapy plays a crucial role in the recovery process. Here’s a breakdown of common physiotherapy treatment approaches:
Splinting:

- Splints come in a wide variety and are made to be more comfortable to wear at all times. A metal pin can be inserted within the bone across the DIP joint to serve as an internal splint in certain severe situations when the patient must continue to operate with their hands (such as a surgeon). Patients are able to keep using their hands as a result. After six weeks, the pin is taken out.
- Splinting may still be effective in situations of persistent mallet fingers. Before thinking about surgery in this situation, splint the finger for eight to twelve weeks to see whether the drooping gets under control.
- Skin disintegration is one of the skin issues associated with long-term splint use. It’s critical to keep an eye out for this and perhaps suggest a new or alternative splint.
- When the wounded finger is splinted for this long, nearby joints may become rigid. Create an exercise regimen to help with finger range of motion and to ease tight joints.
Exercises:
The primary goal of physiotherapy following surgery is to maintain the other joints’ range of motion in order to avoid stiffness.
The use of cryotherapy
- For 10 to 15 minutes, two to three times a day, cryotherapy can help reduce discomfort in its early phases.
Mobilization of the joints
- After the splint is removed, the active and passive range of motion is initiated. The proximal joints are mobilized to progressively reduce stiffness and increase mobility in the fingertip.
Passive range of motion
- In order to preserve the joint range of motion, passively bend the damaged joint softly before straightening it again. Three to four times a day, ten repetitions of each posture are held for five seconds.
Passive finger flexion
- Roll the stiff finger into a complete fist and extend it at the middle joints and tip with the other hand. Repeat for each finger separately. Another way to perform this exercise is to simultaneously extend all four fingers. Repeat ten repetitions while holding this posture for five seconds.
Stretching activities
- With the palms flat on the table, hold each finger individually and raise it one at a time. Hold this posture for five seconds, then repeat ten times.
Glides of the active finger flexor tendon
- Start with your fingers and wrist straight. Make a flat fist by bending at the first knuckle and touching the fingertips to the palm’s base. Reposition the fingers into a claw position and roll them into a complete, tight fist while keeping the fingers taut. Repeat ten repetitions while holding this posture for five seconds.
Pick-up of objects
- Practice handling little items such as buttons, coins, pins, and so on.
Exercises to increase your grip
- Restoring normal hand and finger strength can also be accomplished with strengthening workouts.
- Regaining strength and mobility can be greatly aided by strengthening activities such as gripping a rubber ball, squeeze ball, or therapeutic putty. Repeat ten repetitions while holding this posture for five seconds.
Non-Surgical Treatment
Perhaps six weeks of nonstop splinting, followed by six weeks of splinting at night.
- In most cases, this will lead to enough healing and enable the finger to grow.
- Patient education is crucial for the patient to comprehend the need to preserve DIP joint extension.
- Continuous splinting for the first six weeks is crucial.
- If the splint is taken off and the finger is permitted to bend, the procedure is interrupted and must be repeated.
- Even while taking a shower, the splint needs to be in place.
- The splint should allow the tendon ends to migrate as close together as possible while maintaining the DIP joint in its maximum extension. The tendon is repaired by scar formation throughout the healing process.
- Once the tendon is strong enough to support the fingertip straight, a plan to wean out of the splint is established. You must instruct the client to securely strap their splint with sports tape so that it doesn’t come loose if they continue playing sports while wearing it.
Surgical Treatment
- When the fingertip has slightly migrated, the bone fragment is significant, or the reason is a laceration, surgery is necessary to heal a mallet finger.
- The primary goals of rehabilitation following mallet finger surgery are to maintain the other joints’ range of motion and avoid stiffness from inactivity.
Complication
These issues may arise when mallet fractures are treated surgically or non-surgically.
- On a physical examination, residual extensor lag is seen.
- Swan neck abnormalities (produced by the volar plate being disturbed by the extensor tendon, which causes the proximal interphalangeal joint to stay hyperextended and the distal interphalangeal (DIP) joint to become abnormally flexed)
FAQs
What is the main cause of a mallet finger?
Mallet finger injuries occur when the phalanx’s extensor mechanism is disrupted at the distal interphalangeal joint level, typically as a result of a forceful flexion at the distal interphalangeal joint. The distal phalanx cannot be extended as a result of this damage.
Which tendon is involved with the mallet finger?
Extensor tendons run down the back of the hands and wrists, just beneath the skin. The capacity of the hand to straighten the wrists and fingers is under their control. When a finger is jammed, an extensor tendon ruptures at the base of the finger joint, resulting in a mallet finger injury.
How to avoid a mallet finger?
Extensor tendons run down the back of the hands and wrists, just beneath the skin. The capacity of the hand to straighten the wrists and fingers is under their control. When a finger is jammed, an extensor tendon ruptures at the base of the finger joint, resulting in a mallet finger injury.
Which tendon is involved with the mallet finger?
Extensor tendons run down the back of the hands and wrists, just beneath the skin. The capacity of the hand to straighten the wrists and fingers is under their control. When a finger is jammed, an extensor tendon ruptures at the base of the finger joint, resulting in a mallet finger injury.
What finger is most common for mallet finger?
The dominant hand’s tiny (pinky), ring, and long fingers are most vulnerable to harm. But a mallet can form on any digit.
References
- Mallet Finger, Physio Pedia, https://www.physio-pedia.com/Mallet_Finger
- Mallet Finger – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/mallet-finger-baseball-finger/
- What is Mallet Finger? Symptoms, Causes, Diagnosis & Physiotherapy Treatment of Mallet Finger. . .. . . (n.d.). Cbphysiotherapy. https://cbphysiotherapy.in/condition/mallet-finger