Lumbar spine mobilization techniques
Table of Contents
What is Mobilization for the Lumbar spine?
- Lumbar spine mobilization is a passive, skilled, manual therapy maneuver applied to joints and related to the soft tissue at various speeds and amplitudes taking physiological or accessory movement for therapeutic purposes
- small volume oscillation glide applies at a fast velocity, and a large volume force applies at to slow velocity
- it is a hand-operated method that subsists of applying the target forces on a painful, stiff, or otherwise neglected joint in addition to elevating its overall function. Which is improper in all conditions, spine mobilizations/manipulation assists improve the range of motion, reduces pain, and reduces stiffness.
- Lumbar spine mobilization is a manual therapist’s hand-operated treatment that is frequently executed by physical therapists and healthcare professionals who master rehabilitation for locomotion huddles and chiropractors, health professionals managing disorders of the musculoskeletal system that subsists bones, muscles, soft tissue, and ligaments, etc.
Introduction to the Lumbar Spine
- A healthy spine has three natural loops that generate an S-shape in which the thoracic spine’s middle part creates a convex shape. The spinal curve absorbs shocks to your body and cares your spine from injury. Many different parts create the spine:
- Vertebrae: The thoracic spine has 33 improper vertebrae small bones that hammer the spinal canal. The spinal canal is a cave that houses the spinal cord and nerves, protecting them from injury. Most of the vertebrae locomote to give permission for a range of motion.
- Facet joints: These facet joints have cartilage a greasy connective tissue that gives permission to the vertebrae to slide in against each other. Facet joints give permission to twist and turn, giving flexibility and stability. facet joints may create arthritis and cause back pain or/and neck pain.
- Intervertebral disc: These flat, round cushions lie in the middle of the vertebrae and act as the spine’s shock absorbers. Each intervertebral disk has a soft, gel-like mid-portion of the nucleus pulposus confined by a flexible outer ring the annulus fibrosus. Intervertebral discs are under constant pressure. A herniated disk can crack, and tear, giving permission for some of the nucleus’s gel substance to expose. Herniated disks also termed as bulging, slipped, or/and ruptured disks can be dreadful.
- Spinal cord and nerves: The spinal cord is a line of nerves that pass along with the spinal canal. The line of a nerve from the skull to the lower back. 31 pairs of nerves branch out astride the vertebral beginning in the neural foramen. These nerves carry out messages in the middle part of the brain and muscles.
- Soft tissues: Ligaments affix to the vertebrae to clasp the spine in an upright proper position. Muscles support the back and help you to turn and twist on the front side and/or backside. muscle’s Tendon associates the muscles with bones and benefit movement.
What are the spine segments?
- The 33 vertebrae compose five specific spine segments. Starting at the neck and/or going descending toward the buttock’s rear end, these segments subsist
- cervical spine
- thoracic spine
- lumbar spine
- sacrum
- coccyx
Lumber spine
- Lumbar spine (lower back): Five vertebrae L1 to L5 create the lower part of the spine. the lumbar spine assists the upper part of the spine. It affixes to the pelvis and lifts most of your body’s weight, along with the stress of lifting and carrying items. Many back problems create in the lumbar spine. The lumbar spine turns/twists inward side to create a C-shaped lordotic curve.
ligaments of the lumbar spine
iliolumbar ligament
- The iliolumbar ligament is a strong strap-like band of connective tissue. and 1 of the 3 vertebropelvic ligaments. The other ligaments are the sacrotuberous and the sacrospinous ligaments. They help to stabilize the lumbosacral spine on the pelvis.
- The iliolumbar ligaments are decisive in assisting the lower lumbar spine; they affix the 4th and 5th lumbar vertebrae L4 and L5 to the iliac bone crest at the back of the pelvis. Injury to the iliolumbar ligament, fairly common among certain athletes due to the amount of agitated spinal motion involved in many sports, can create sacroiliac joint pain and related problems. The sacroiliac joint is destinated in the pelvis and assists to conduct the spine’s stable
Attachments
- Origin: the transverse process of L5
- amination: deep into the ventral area of the iliac crest 6-7cm from the central line
- The main part of the iliolumbar ligament originates from the L5 vertebral transverse processes. animation is protected by the crest dorsally, making it not attainable to palpation
Function
- It plays an essential role in the restraining movement in the lumbosacral and sacroiliac joints. The iliolumbar ligament strengthens the lumbosacral joint assisted by the lateral lumbosacral ligament, and, like all other vertebral joints, via the posterior and anterior longitudinal ligaments, the ligamentum flava, and the interspinous and supraspinous ligaments.
Sacrospinous ligament
- The Sacrospinous ligament small and/or anterior sacrosciatic ligament of the sacroiliac joint is a pelvic ligament. It is a thin triangular strap-like band and its length is about 3.8-4.6cm.
- The sacrospinous ligament’s fibers are knit with the sacrotuberous ligament. Posteriorly, the sacrotuberous ligament is the back of the sacrospinous ligament. Anteriorly, The sacrospinous ligament obscures the coccygeus muscle. It is affixed by the spine of the ischium and the outer edge of the sacrum and coccyx.
Attachments
- The sacrospinous ligament plays a broader role in the greater and lesser sciatic foramen. The greater sciatic foramen lives across the ligament and gives a path for superior gluteal nerves and/or vessels to join from the pelvis while acting as a passage for the inferior gluteal vessels and/or nerve, sciatic and posterior femoral cutaneous nerves to surround through and exit the pelvis.
- The lesser sciatic foramen is under the ligament, passing the tendon of the obturator internus, its nerve, and the internal pudendal vessels and nerve
Function
- The sacrospinous and sacrotuberous ligaments support pelvic stability. The ligament tasks with the sacrotuberous ligament to inhibit rotation of the illum past the sacrum thus inhibiting excessive twisting of the pelvis, low back pain, and sacroiliac junction strain.
Sacrotuberous ligament
- The sacrotuberous ligament is a stabilizer of the sacroiliac joint and affixes the bony pelvis to the vertebral column.
- the sacrotuberous ligament Is in the shape of a fan destinated in the posterior side of the pelvis, on both sides, and affixes to the sacrum to the iliac tuberosities.
- It subsists mainly of collagen fibers, it is strong enough to assist the sacrum and prevent adverse changes under body weight
- The Sacrotuberous ligament assists in pelvic stability and the obliquity arrangement of the sacrotuberous ligament on both sides prevent the anterior tapping of the sacrum by operating to control sacral nutation.
- The Sacrotuberous ligament prevents the sacrum from tapping forward when downward pressure is applied to the spine. It is tensed with sports that generate a lot of arching in the lower back like high jumping, golfing, gymnastics, pitching, and volleyball spiking.
- affixing the lower limb with the trunk, biceps femoris, and perineum to the thoracolumbar fascia, and erector spinae.
- sacrotuberous and sacrospinous ligaments stabilize the sacrum against twisting/turning with the pelvis, and excessive side bending. thus, an imbalance in the center of the sacrotuberous ligament on both sides causes pelvic rotation, Sacroiliac junction strain, or LBP
Nuchal ligament
- the nuchal ligament is destinated on the back of the neck extension with the Supraspinous ligament. It hammers a 2-layered fibroelastic septum that disassociated the dorsal muscles of the neck and runs from the spine of the C7 vertebra to the occiput bone.
attachments
- Extension from the external occipital protuberance on the skull and median nuchal root to the spinous process of C7 vertebrae. The deep fibers of the ligament associate with the external occipital crest, the posterior tubercle of the atlas, and/or the medial surface of the bifid processes of the other cervical vertebrae.
Function
- Limits flexion
- gives affixation between Trapezius and Splenius capitis.
Apical ligament of dens
- extents in the middle of the 2nd cervical vertebra in the neck and/or the skull. It lives as a fibrous cord in the triangular interval in the center of the alar ligaments.
- The ligament was on a median of 7.5 mm long and 5.1 mm broad. Structurally, the ligament is a small converging of elastic fibers surrounding a core of notochordal particles necessary it represents a rudimentary nucleus pulposus that is the particle of notochord shown at other vertebral levels.
attachments
- arise from the tip of the odontoid process on the Axis commonly hammer a small coronal groove located there and aminates into the anterior rim of the foramen magnum at the base on the center point.
- The apical ligament is not attached anteriorly from the anterior atlantooccipital membrane by a thin layer of fat and connective tissue. dorsally it is detached from the superior crus of a cruciform ligament by an intervening layer of connective tissue. The tectorial membrane is developed further dorsally, posterior to the cruciform ligament. Laterally the alar ligaments elong from the odontoid to the medial aspect of the condyles of the occipital bone. There is no accordant relation between the middle of the alar ligament and the apical ligament.
function
- The apical ligament is a small ligament that affixes the apex tip of the dens of the C2 vertebra to the anterior edge of the foramen magnum. It is the weak, fibrous particle of the notochord and does not devote original stability.
cruciate ligament of the atlas
- The cruciform ligament of the atlas cruciate may another form of the cruciform ligament is a cruciate ligament in the neck hammering part of the atlantoaxial joint. The ligament is named cruciate as such because it is in the shape of a miffed.
- It consists of two bands:
- Longitudinal band.
- Transverse band.
function
- It is the most important ligament that clasps the posterior dens of the C2 vertebra in cemented at the atlantoaxial joint. It lives back of a large synovial bursa surrounding a loose fibrous capsule and subsists in two bands:
- Longitudinal band: affix the body of the C2 axis to the foramen magnum
- Transverse band: affix to the inner margin of the C1 atlas lateral masses on both sides.
ligamentum flavum
- The ligamentum flavum is a short but wide ligament that affixes the laminae of adjoining vertebrae from C2 to S1 and/or is determined as a medical word elongation of a facet joint. It concludes 80% elastin fibers and 20% collagen fibers. The high percentage of elastin protein fibers provides to the ligament with its yellow color and flexible nature.
- in spite of the elastic and flexible essence of the ligamentum flavum, at the upright position, the ligament has a hypocrisy prohibiting it from buckling. At the lumbar vertebra, the neutral position is obtained by the traction and tension forces put by muscles on the Thoracolumbar fascia by the supraspinous, interspinous ligaments to ligamentum flavum generate hypocrisy in the neutral position of the theinterspinous_supraspinous thoracolumbar ligamentous complex
- At any intersegmental level, the ligamentum flavum is a joined structure represented symmetrically on both sides.
- In the neck side part, the ligaments are thin but broad and long; ligaments are wider in the thoracic segment and broadest in the lumbar segment.
Attachments
- The ligament flavum arises from the lower half of the anterior surface of the lamina apart from and affixed to the posterior surface and upper margin of the lamina under, hammering a cup-like shape clasp on the upper border of the lamina under.
- On either side the ligament is the division into two portions:
- The medial portion: ravine to the back of the next lower lamina and astride the gap in the middle of the neighboring vertebrae fusing with the interspinous ligament
- The lateral portion: ravine in front of the facet joint where it affixes to the anterior aspect of the inferior and superior articular processes and hammers the anterior capsule. Most lateral fibers elongated apart from the superior articular process to the under the pedicle.
Function
- The point-out elasticity provides conserves the upright posture and assists the vertebral column in reopening its shape after flexion. It prohibits the exaggerated separation of the relative vertebral lamina and prohibits buckling of the ligament into the spinal canal during extension, prohibiting canal compression. The lateral part of the ligament inhibits the anterior capsule of the facet joint from hideout within the joint cavity during movement.
supraspinous ligament
- The supraspinous ligament or/and the supraspinal ligament is a strong fibrous cord that affixes in association with the apices of the spinous processes from the 7th cervical vertebra to the 3rd or 4th lumbar vertebrae. From the C7 vertebra to the skull ligament turn structurally specific from more back parts of the ligament and is called the ligamentum nuchae
- Origin: It originates from the C7 vertebra.
- Insertion/Terminates: Sacrum
- The supraspinous ligament is fully grown up only in the upper lumbar part and may terminate at L3 vertebrae, in spite of the most common termination site tending to be at L4 vertebrae. The supraspinous ligament is almost not present at L5 and S1 vertebrae.
- It is thicker and broader in the lumbar part rather than in the thoracic part, it associates with the thoracolumbar fascia.
- The most superficial fibers of the supraspinous ligament enlarge betwixt 3 or/and 4 vertebræ; those numerous deeply seated ligaments pass away in the mid part of 2 or /and 3 vertebræ while the deepest ligaments affix the spinous processes of neighboring vertebrae
- The deep layer of the supraspinous ligament is organized by tendinous fibers of the multifidus muscle. in the middle of the spinous processes, it is elongated with the interspinal ligaments. The supraspinous ligament’s mid fibers affix with the thoracolumbar fascia’s dorsal layer.
Function
- restricts flexion onward with other ligaments of the vertebral column.
- The supraspinous ligament devotes as a part of the central line affix for some important muscles.
- The supraspinous ligament benefits in conducting the upright position of the head.
- supraspinous ligament stretched in flexion, its fibers prohibit the division of spinous processes during forward flexion, while hyperflexion, the interspinous ligament, and supraspinous ligament are the first to reduce.
- At the lumbar part, through the affixation of the supraspinous ligament to the thoracolumbar fascia and interspinous ligament, the ligaments hammer in association with the Interspinous_supraspinous thoracolumbar ligamentous complex which it`s function is to remove tension that is positioned on Thoracolumbar fascia to ligamentum flavum causing conceit in the neutral position
intertransverse ligament
- the intertransverse ligaments are ligaments that are compassed in the middle of the transverse processes of the lumbar spine.
- In the cervical part, the intertransverse ligament subsists of a few uneven, scattered fibers that are repeatedly reachieved by muscles. In the thoracic part, the intertransverse ligament is rounded cords affectionate affix to the deep muscles of the back. In the lumbar part, the intertransverse ligament is thin and fuzzy.
- The intertransverse ligaments in general fusion with the intertransverse muscles.
- The function of the intertransverse ligaments is to prohibit lateral flexion of the lumbar spine.
- The posterior longitudinal ligament bear to be most developed at the level of the L3 and L4 vertebrae, where its median thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker mid-segment almost about 2.5 to 4 mm thickness all over the length of the ligament. The ligament in the central part of every vertebral body shield the vascular foramina
interspinous ligament
- This ligament is determined of thin sheets affixing the spinous processes from roots to apexes from C1 to S1 vertebrae one part at a time. Anteriorly, Its fibers affix with ligamentum flavum, in association with dorsally its fibers affix with the supraspinous ligament. The ligaments are small and/or lengthen in the thoracic part, broader, thicker, quadrilateral in hammers in the lumbar area, and only are slightly clear in the neck. In the neck, the interspinous ligament is normally established as part of the nuchal ligament.
- The interspinous ligaments are thin and short structures that affix enthusiast spinous processes. The Interspinous ligament is well vascularized and subsists of sensory nerves, particularly on their posterior and lateral surfaces. These ligaments arise fairly from the ligament Flava, fairly from the reciprocal vertebral laminae, and fairly from the caudal aspect of the spinous process. The lumbar Interspinous ligament is fairly thicker and bears to be more sparkler and quadrilateral in nature and in general, happens in pairs. The lumbar Interspinous ligament is usually blocked out with a fiber direction passing obliquely or/and horizontally in an anterior-posterior direction from the superior margin of the caudal spinous process to the cranial spinous process.
- The Interspinous ligament is part of the posterior ligamental complex, and the ligament acts as a stabilizer of the thoracic spine and assists to limit spine flexion.
nerve supply
- The lumbar interspinous ligaments access a nerve supply from the medial branches of the lumbar dorsal rami and experimental stimulation of the interspinous ligament provides low back pain and referred pain in the lower limbs. nerve devotes the interspinous ligament as a captivating source of low back aches.
blood supply
- The interspinous ligament is well supplied by small blood vessels and/or sensory nerves, then after, chiefly in its posterior part and/or on its lateral surfaces.
- movements The role of the interspinous ligament is to restrict flexion bending forwards by prohibiting the division of the spinous processes of the vertebral column.
anterior longitudinal ligament
- A strong strap like a band of fluctuating thickness and/or width glazes the anterior side of the vertebral bodies and intervertebral discs the whole length of the vertebral column. in distinction to superficial to its deep layer ligamentous fibers run differing lengths:
- the nethermost fibers are short intersegmental fibers
- the intermediate fibers adjoining 2 to 3 vertebrae
- the superficial fibers adjoining 3 to a vertebrae
- It is thick, yet narrow, among the vertebral bodies where it is loosely adjoining to the periosteum. At the levels of the intervertebral disc, the anterior longitudinal ligaments broaden and the fibers strongly affix to the fibrocartilage disc the hyaline cartilage in vertebral end plates, and the margin of the vertebra
- A primary spine stabilizer besieges one inch broad, and the Anterior longitudinal ligament travels the all-over length of the spine in distinction to the base of the skull, by the cervical, thoracic, and lumbar spine to the sacrum. It associates the anterior side anterior of the vertebral body with the front of the annulus fibrosis.
- posterior longitudinal ligament affixed to the upper and lower boundary of the particular vertebral body.
- decrease the extension of the vertebral column and marked out the intervertebral disc.
- the boundary on the anterior surface of the vertebral bodies is the vertebral column.
animation
- The anterior longitudinal ligament is vivid by recurrent branches of rami communicantes.
posterior longitudinal ligament
- The posterior longitudinal ligament is one of the most important ligaments that distribute stability in the lumbar spine. It gorge along with the posterior aspect of the vertebral body and the inner side of the vertebral canal from the body of the axis to the sacrum. The posterior ligament is a series of longitudinal fibers that are opaquer than the anterior longitudinal ligament. nonetheless, like the anterior longitudinal ligament, the dim fibers are deeper and affix to one vertebra while the superficial fibers affix to 3 to 4 vertebrae. The superficial layer is an elongation of the tectorial membrane at the axis of the posterior longitudinal ligament, and the deep layer is an arisen of the cruciform ligament at the Atlas.
- The fibers are wide at the intervertebral spaces and are more disciple to the annulus fibrosus of the intervertebral discs rather than at the vertebral body where fibers of the posterior longitudinal ligaments are thinner. This eccentricity is more in the posterior ligament rather than in the anterior. Therefore, the posterior longitudinal ligament is much more courtly rather than the anterior longitudinal ligament, which is constraining for the disc herniation deriving posterolateral.
- The Posterior longitudinal ligament adds superficial and deep connective tissue layers, The superficial layer is the more dorsal side, with its elongation from the dura mater often being difficult to identify. the superficial layer subsists of a central band of fibers 8 to 10 mm broad expanding beyond many vertebral segments. because of its major adjoining with the intervertebral disc, it has been known as being ‘‘feeble’’, granting a craggy appearance over every vertebral body. This craggy look turns more probable in the lower thoracic and lumbar parts, where the superficial layer is of more decent width.
- connotation alteration even within the lumbar part, where both the central fibers and the ‘‘fan-like’’ part favor a decrease in width in the center of L1 and L5 vertebrae. The deep layer, which is disciple to the superficial layer in the midline, is of more decent diameter whole its length, being 2 to 3 mm wide at its precarious point. It also has a craggy appearance.
- In the cervical part, the Posterior longitudinal ligament is a broad band-like structure of equal width betwixt both the intervertebral disc and vertebral body, however more inferiorly, it is made acceleratingly craggy, with its fastest part being betwixt the intervertebral disc The division fibers of the superficial and deep layers were difficult to analyze at the level of the intervertebral disc, but the intervertebral disc affixation to the boundary of the vertebral bodies and intervening annulus fibrosus was clear.
- The fibers of each and every layer came to emphasize, hammering standard affixation. Both the superficial and deep layers of the posterior longitudinal ligament are affixed to a midline of the bony septum on the posterior surface of the vertebral body in the middle of the superior and inferior boundary. The association was only sometimes cultivated because of not sufficient in the septum in the central 3rd of the vertebral body. The adaptation of fibers within the posterior longitudinal ligament was constant at all levels, with the fiber in the central portion of the superficial layer being more vertical than those of the ‘‘fan-like’’ part. even if the deep layer was observable over the superficial layer
- The posterior longitudinal ligament has a more inimical than supportive role. The observable pattern of movement of inimical materials like masses and bony fragments following a vertebral fracture into the vertebral canal advises that the Posterior longitudinal ligament acts as a supporter for the spinal cord and from displaced disc material.
- Fibers of the superficial layer will prohibit forward flexion, while the oblique fibers of the deep layer will prohibit lateral flexion and rotation. fibers from superficial and deep layers subsist in all movements, with the elevating number of fibers enrolled with elevating pressure. The craggy looks of the Posterior longitudinal ligament in the lower thoracic and lumbar parts may be due to the raised rotational and lateral flexion forces bore out in the lower area correlated to the upper part of the vertebral column of the spine. The presence of elastin protein in the Posterior longitudinal ligament benefit that it has a role in the many movements of the spine. observed patterns of disc fragment migration following vertebral burst fractures announce that the Posterior longitudinal ligament also preserves the consists of the vertebral canal.
Blood supply
- The dominant supply of blood to the spinal cord is in distinction to a single anterior spinal artery and the two posterior spinal arteries. Two posterior spinal arteries are the branches of the vertebral artery in the spine. Posterior arteries supply the blood to the posterior part of the spinal cord, and the anterior part obtains blood supply from the anterior spinal artery. neighboring to the spinal arteries, there are other arteries also available at each and every spinal segment designated radicular spinal arteries, which derive from the body wall arteries. The small penetrating arteries emanate off via both anterior and posterior spinal arteries that hammers interrelate in the spinal cord.
- The radicular spinal arteries send the blood to the ventral and dorsal parts of the spinal cord. The bilge of blood from the spinal cord snippet the place with the aid of anterior and posterior spinal veins. The anterior and posterior spinal veins aqueduct into the internal and external venous plexus. over the venous plexus, the blood aqueduct into the main venous system with the help of azygos veins, lumbar veins, and hemizygous veins
nerve supply
- The prime origin of the nerve supply of the posterior longitudinal ligament is the meningeal branch employed from the spinal nerve. It unison ascending and descending branches in the vertebral column of the lumbar spine. There are transverse roots hammered by the mixture of ascending and descending nerve roots. The compound of the transverse branches from the antagonist side creates affixation of nerve fibers superficially, which animates the posterior longitudinal ligament in the vertebral segment of the lumbar spine. The posterior part of the annulus fibrosus is furious by the nerve fibers hammering a network deeply in the intervertebral part of the posterior longitudinal ligament
- There is no innervation of the deep layer of the nucleus pulposus or/and annulus fibrosus due to the shortcoming nerve fibers and nerve boundary. some nerve boundaries are available in the middle part of the nucleus pulposus, but in the peripheral zone, there are bulky nerve fibers. The heavy nerve fibers in the peripheral part act as a needle part in the regulation of movement and posture in the vertebral column of the spine.
muscle
- There are 3 groups of muscle in the posterior of the lumbar spine; superficial, intermediate, and deep muscle layers. The superficial layer sustained two muscles the splenius cervicis and splenius capitis. muscles act as the needed part in the extension of the neck and the movement of the shoulder.
- The intermediate muscle group sustains the longissimus, iliocostalis, and/or spinalis muscles. longissimus, iliocostalis, and spinalis muscles of the intermediate group have the same tendinous innervation. The intermediate groups of muscles benefit from the flexion of the head and the upper vertebral column and the movement of the thoracic cage. The deep layer sustains the semispinalis, rotatores, and multifidus. The major function superficial intermediate and deep muscle group is the stabilize the vertebral column and manage an upright posture. The intermediate group of muscle in the lumbar spine also assist in balance and proprioception
variants
- the posterior longitudinal ligament is smaller and sluggish. It has an egg shape that fluctuates from 2 to 2.25 mm in thickness at the level of L5-S1. From the L5 vertebrae upwards, the ligament hammers a slim band, which widens samely at the level of each disc. The fibers of the annulus fibrosus and the boundary of the vertebral body of the lumbar spine are the sites of association of the ligament, but in some cases, not all, it is associated with the posterior aspect of the vertebrae.
- The posterior longitudinal ligament bear to be most established at the level of the L3 and L4 vertebrae, where its median thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker mid-segment almost approx 2.5 to 4 mm thickness all over the length of the ligament. The posterior longitudinal ligament in the mid-part of every vertebral body envelops the vascular foramina
Anterior atlanto axial ligament
- The anterior atlantoaxial ligament is a strong membrane, fixed, beyond, the lower border of the anterior arch of the atlas; under the front of the body of the axis.
- It is strengthened in the midline by a rounded cord, which affixes to the tubercle on the anterior arch of the atlas to the body of the axis, and is an elongation upward of the Anterior longitudinal ligament.
- The ligament is in neighboring, in front, with the long capitis.
movements and ligaments in the lumbar spine
- Anterior Atlantoaxial Extension
- Posterior Atlantoaxial Flexion
- Ligamentum Nuchae Cervical Flexion
- Anterior Longitudinal Axis – Sacrum Extension & emphasize the front of the annulus fibrosis
- Posterior Longitudinal – Sacrum Flexion & emphasize back of annulus fibrosis
- Ligamentum Flavum – Sacrum Flexion
- Supraspinous ligament Thoracic & Lumbar Flexion
- Interspinous ligament Lumbar Flexion
- Intertransverse ligament Lumbar Lateral flexion
- Iliolumbar ligament Sacroiliac joints Stability & few motions
- Sacroiliac joints Stability & few motions
- Sacrospinous ligament Sacroiliac joints Stability & few motions
- Sacrotuberous ligament Sacroiliac joints Stability & few motions
muscle of the lumbar spine
- multifidus
- quadratus lumborum
- psoas major
- longissimus
- spinalis
- iliocostalis
- musculus iliocostalis lumborum
- inter spinalis
- levator scapulae
- serratus posterior inferior
- intertransversarii
- transversospinalis
- rhomboid major
- longissimus cervisis
- semispinalis thoracic
- semispinalis cervicis
- longus capitis
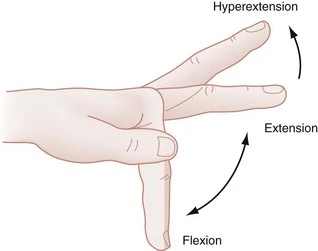
- Flexion 50 degrees
- Extension 15 degrees
- Right lateral flexion 20 degrees
- Left lateral flexion 20 degrees
- Right rotation 5 degrees
- Left rotation 5 degrees
What conditions and disorders affect the spine?
Vertebrae and disks of the lumbar spine can wear downward with age, causing pain. Other conditions that affect lumbar spine health involve:
- Arthritic conditions, such as ankylosing spondylitis
- lumber spondylolisthesis
- intervertebral disc prolapse (PIVD)
- Back strains and sprains.
- Birth defects such as spina bifida.
- Bone spurs rugged the ends of the vertebrae that put pressure on the spinal cord and nerves.
- spine curve like lordosis
- Neuromuscular diseases, such as amyotrophic lateral sclerosis, pseudo bulbar palsy, progressive bulbar palsy
- Nerve injuries like spinal stenosis, sciatica, and pinched nerves.
- Osteoporosis weak bone.
- Spinal cord injuries, including spinal fractures, herniated disks, bulging disks, and paralysis, paraparesis.
- Spine tumors and cancer.
- Spine infections like meningitis and osteomyelitis.
Goals for spine mobilization
pain, muscle guarding, and spasm
- painful lumbar spine, reflex, muscle guarding, and muscle spasm can be observed with slight joint play tasks to stimulate neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and/or distraction movement are used to inspire mechano receptors that may prohibit the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- little amplitude distraction or gliding for movement of the lumbar spine is used to create synovial fluid movement, which is an agent for obtaining nutrients to avascular portions of the articular cartilage
- musical joint play task assists to maintain nutrient exchange and prohibits the painful and degenerating effects of statis when the lumbar spine is swollen or/and painful, and can not go over a range of motion
- when adjusted to treat pain, muscle spasms and muscle guarding small amplitude tasks should not apply stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be observed with a progressively vigorous joint stretching task to elongate hypermobile capsular and ligamentous connective tissue
- uninterrupted or/and distracted stretch forces assisted to distend a shortened tissue mechanically
Positional faults/subluxations
- A faulty or/and incorrect position of one bony companion in addition to its antagonizing surface may affect the outcome in limited motion or/and pain
- positional faults can eventuate with the traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be conserve
- by maladapted neuromuscular control across a joint
- during observing an active range of motion, faulty tracking of the joint surface outcome in pain or/and lessened motions
Progressive limitations
- diseases that progressively restrict movement can be observed with joint play tasks to maintain available motion or/and lessen the progressive automated deduction
- the patient’s response to the motion is necessary for the dosage of distraction or/and glide to treatment and the state of the disease
Functional immobility
- when the patient can’t functionally turn the lumbar spine for a longer period
- the lumbar spine can be observed with nonstretch gliding or/and distraction tasks to maintain available joint play and prohibit degenerating and reduce the effect of immobility
Grades for lumbar spine mobilization
- grade 1 small amplitude oscillations are necessary for pain, modulation, typically during the acute stage of injury
- grade 2 large amplitude oscillations are used for pain modulation, dosage, and indication same for grade 1
- grade 3 large amplitude oscillation that goes up to the restrictive joint limit,
- grade 3 is designed to improve joint ROM and is used only during the subacute, chronic stage of healing
- grade 4 small amplitude oscillation that goes up to the limitive joint limit,
- grade 4 is designed to improve joint ROM and is used only during the chronic stage of healing
- grade 5 high-velocity thrust and low amplitude thrust applied at the physiologic limit of joint motion
- grade 5 is performed only one time and solely improves from
Lumbar spine mobilization
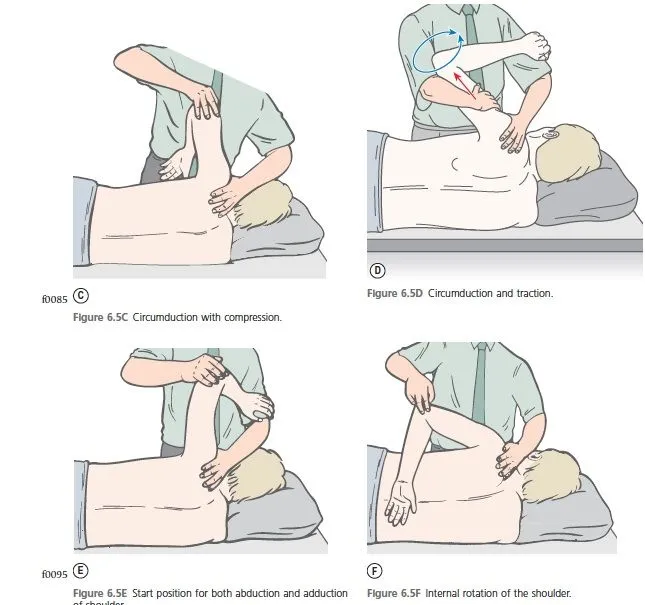
lumbar spine extension

- patient position: prone lying, put a pillow beneath the abdominal part for patient comfort and to provide a neutral lumbo sacral curve
Therapist position and hand placement
- place your pisiform bone hypothenar eminence away from the spinous process
- relax your hand on the patient’s back
Mobilizing force
- give thrust with your hypothenar eminence in an anterior direction
- proper alignment of your trunk directly above the part, so the direction of force is directed downward and not an angle
Lumbar spine rotation

- patient position: prone lying, put a pillow beneath the abdominal part for patient comfort and to provide a neutral lumbo sacral curve
Therapist position and hand placement
- put your pisiform hypothenar eminence beyond the transverse process on the side to reveal the direction of motion you wish to encourage
- if wanting to prompt left rotation, place your hypothenar eminence on the right transverse process
- relax leisurely with your hand supported on the patient’s back
mobilizing force
- apply thrust with your hypothenar eminence in an anterior and medial direction
lumbar spine side bending

- patient position: side-lying with the affected side downwards
- position the patient closer to the margin of the bed as possible
- flexes both the hip and knees to 90 degree
Therapist position and hand placement
- stand facing the patient
- place the tip of your caudal hand on the superior spinous process to observe the motion
- passively rotate the patient’s trunk backward side to “take up the feeble” until just before feeling the vertebral part move
- now put the tip of the finger of your cephalad hand on the superior spinous process to observe the motion
- flex both the hips of the patient until just before you feel the vertebral part move
- the patient’s leg can be assisted either on the plinth or with your thigh
mobilizing force
- bear the patient’s leg into the hip rotation, causing the lumbar spine to side bend
HVT lumbar roll

- patient position: side lying with reduced side upward,
- position the patient closer to the boundary of the bed as possible
- flex the hip and knee 90 degrees
- give a pillow for the patient to hold the position and act as a physical barrier
Therapist position and hand placement
- stand facing the patient
- place the fingertip of your cephalad hand on the inferior spinous process to observe the motion
- move the patient’s top side of the leg into hip flexion until just before you feel the inferior vertebral area move
- maintain the hip flexion by stabilizing the leg in the middle of the therapist’s body or/and the treatment table
- move the cephalad hand to the superior spinous process to monitor the motion
- passively rotate the patient’s trunk backward to “take up the feeble” until just before feeling the superior vertebral part move
- rest of the forearm relax on the patient’s body part
- the therapist’s hand should be directly over the segment to be manipulated
Mobilizing force
- therapist applying the downward rotational thrust in front of the treatment table with the cephalad forearm and hand while applying a rotational force over the caudal forearm by grasping the patient’s lower trunk toward your body
Precaution for lumbar spine mobilization
- if a mobilization task creates a change in sensation or an elevated pain to radiate down an extremity or/and if a patient reports a feeling of dizziness or lightheadedness or does not perform additional manipulation
- use exaggerated precaution if the patient reports either a current history of corticosteroid use or excessive pain
Joint effusion
- the lumbar spine effusion occurs due to trauma or disease
- rapid swelling of the lumbar spine generally designate
- bleeding in the lumbar spine and may happen with diseases aspiration of the blood to lessen the necrotizing effect on an articular cartilage
- slow swelling for more than 4 hours generally designates serious lumbar spine effusion or edema on the lumbar spine due to mild trauma irritation or disease
- do not stretch the inflamed or injured spine with manipulation because the joint capsule is already stretched by being expanded to accommodate the extra fluid
- the reduction of motion is, in addition, to add extra fluid and muscle response to pain, not from shortened fibers
- gentle oscillating motion that does not stress the capsule may help to block the transmission of a pain stimulus so it is not perceived and may help to initiate fluid flow while maintaining available cooperative movement
- if a patient’s response to a slight task is increased pain or spine irritability
- the method of glide was exercised too strenuously or should not be done with the current state of pathology
Inflamation
- whenever inflamation is present, stretching raises pain and muscle guarding conclusion in greater tissue damage
- gentle distraction movements may temporarily delegate the pain response
hypermobility
- the lumbar spine of the patient with probable necrosis of ligaments or/and capsules should not be manipulated with stretching task
FAQS
- How long do you do joint mobilization for the lumbar spine?
Typical treatment of the lumbar spine joint may add a series of 3 to 6 manipulation clasps on up to 30 seconds, with 1 to 3 oscillations or/and glide per second
- When do we use joint mobilization for the lumbar spine?
The major goal of lumbar spine mobilization is to re-achieve the normal spine lumbar movement that might have been negotiated by damage or/and injury. Normal movement of the affected/operated lumbar spine will be re-achieved faster if it is negotiated early in the treatment program. Also, mobilization is effective in cases when the range of motion is absent in the lumbar spine
- how much time mobilization is given for the lumbar spine ??
soft tissue mobilization was applied three times a week and home program exercises were recommended which consists of the positioning of the lumbar spine
- Why is early mobilization necessary after an injury?
In patients with acute lumbar spine injuries, early mobilization prohibits pain and swelling and appreciates functional outcomes correlated with cast immobilization
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation begins rangeless, untaken the limit of movement, apply the glide for 2 or 3 seconds for 1 to 2 minutes
that goes center directly into the range of movement, attending each part of the range and till not arriving at the end range movement. This task can be given to treat stiffness by elevating the range of movement and pain