Lower Cross Syndrome
Table of Contents
What is a Lower Cross Syndrome?
The ‘Lower cross syndrome’ is sometimes referred to as the pelvic crossed syndrome, unterkreuz syndrome, or distal crossed syndrome. It occurs as a result of muscular strength imbalances in the lower body. These imbalances happen when muscles continue to shorten or lengthen in proportion to one another.
Muscle weakness and stiffness are prevalent in this syndrome, which crosses across the dorsal and ventral aspects of the body. Hyperactivity and tightness in hip flexors and lumbar extensors are evident in LCS. In this syndrome, the hamstring muscles are tense. This imbalance problem results in an anterior tilt of the pelvis, greater hip flexion movement, and lumbar spine hyperlordosis.
The name LCS comes from the cross pattern of afflicted muscle.
LCS is the most common compensatory pattern in the body, according to the National Academy of Sports Medicine (NASM), in other words.
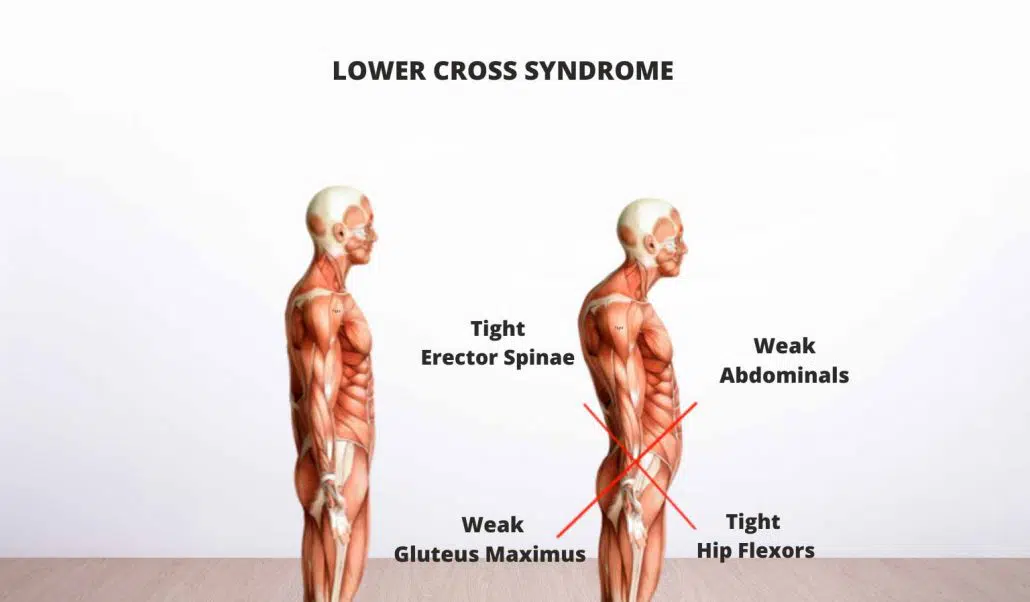
In this case, the abdominal muscles and the gluteus maximus muscles are weakened, which is the most significant muscle in the buttocks. LCS patients have tightened hip flexors and the lumbar erector spine (the collection of muscles that runs from the base of the cranium to the hip) to alter their posture and movement patterns. The person’s lower back arches and pelvis tilt forward to compensate for these difficulties.
In short, Lower Cross Syndrome happens when there is a muscular imbalance between weak and tight muscles. Tight muscles include the hip flexors and erector spinae, whereas weak muscles include the abdominals and gluteal muscles. The hip flexors become shorter, while the abdominal and gluteal muscles become weak.
Clinical relevant anatomy:
The lower crossed syndrome is characterized by weakness of the trunk muscles (rectus abdominis, obliques internus abdominis, obliques externus abdominis, and transversus abdominis), as well as gluteal muscle weakness (gluteus maximus, gluteus medius, and gluteus minimus). The superficial muscles are inhibited and substituted for when they are activated.
Overactivity and tightness of the thoracolumbar extensors muscles(erector spinae, multifidus, quadratus lumborum, and latissimus dorsi) and hip flexors muscles (iliopsoas and tensor fasciae latae) coexist.
The hamstrings compensate for an anterior pelvic tilt or a gluteus maximus that is inhibited.
Causes of LCS:
A sedentary lifestyle is the most common cause of LCS. Sitting for extended periods of time might result in muscle imbalance.
For example, if a person strengthens their hip flexors and back without focusing on their glutes and abdominals, this could lead to an imbalance.
Different muscle groups which are weak and tight can cause LCS.
Muscles that can become weak following:
The trunk muscles consist of:
- Rectus abdominis
- Obliques internus abdominis
- Obliques externus abdominis
- Transverse abdominis
The gluteal muscles consist of:
- Gluteus maximus
- Gluteus medius
- Gluteus minimus
Different muscle groups that can become tight following:
Thoracolumbar extensors include:
- Erector spinae
- Multifidus
- Quadratus lumborum
- Latissimus dorsi
Hip flexors include:
- Iliopsoas
- Tensor fasciae latae.
Lower Cross Syndrome is caused by poor posture, sedentary lifestyle, or leisure habits example working a desk job, watching a lot of television, spending a lot of time on the computer, or doing another activity in prolonged sitting. It is caused by an increase in stress on the particular muscles. Improper posture or form when exercising, or a lack of awareness of how to do daily chores, can cause muscles to experience one-sided stress or excessive tension in certain places.
Symptoms of LCS:
LCS can affect a person’s posture and restriction of movement and having pain in the whole body. People may also suffer from:
- Decreased mobility or stiffness in the lumbar spine, hip, pelvis, or pelvis.
- Pain occurs in the hip flexors, groin, spine, or gluteal muscles.
- An abdomen protruding from the lower back that is too arched.
- Tightness is present in the lower back and/or gluteal muscles.
- Postural changes include anterior pelvic tilt, lumbar lordosis, lateral lumbar shift, and external hip or knee hyperextension and rotation.
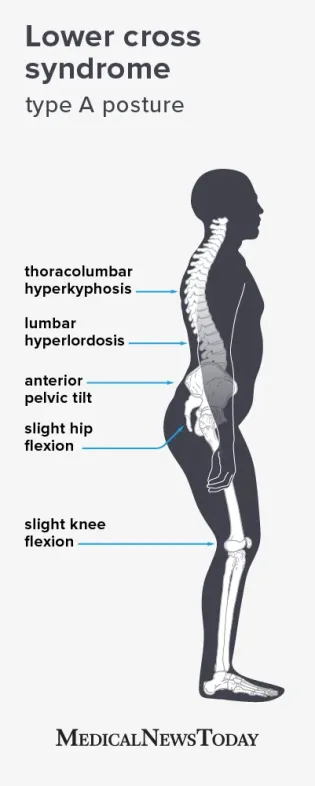
LCS may result in two types of posture, according to the American College of Osteopathic Medicine: type A and type B.
Features of type A posture:
- Hyperkyphosis: In this condition person’s upper back rounder
- Hyperlordosis: In this condition present excessive curvature of the lower back.
- Anterior pelvic tilt: It means the pelvis tilts backward side.
Type A: Posterior pelvic cross syndrome:
The type A subgroup is the posterior pelvic crossed syndrome. In this subgroup extensor muscles are dominant because the hip flexor muscles are shortened, the pelvis is tilted anteriorly and the hip and knee are slightly in the flexion position. Associated with an anterior translation of the thorax because of an increased thoracolumbar extensor activity. Hyperlordosis of the lumbar spine and hyperkyphosis in the thoracic to the lumbar spine.
This leads to a reduction in the quality of breathing and postural control. The more anterior and elevated position of the thorax will disturb the stabilization pattern of the Lower Pelvic Unit.
Example:
During the inspiration movement, the patient will lift the thorax which causes an upper chest breathing pattern. This means the active expiration will be difficult because the abdominal muscles fail to bring the thorax down and back into the more expiratory neutral position.
The abdominal muscles are not to create adequate intra-abdominal pressure so that the expiratory phase is shortened. This problem happens when the coordination and co-activation between the transverses and the diaphragm muscle are imbalanced. So the patient is forced to use the Central Posterior Clinch behavior, which results in hyperactivity of the psoas muscles.
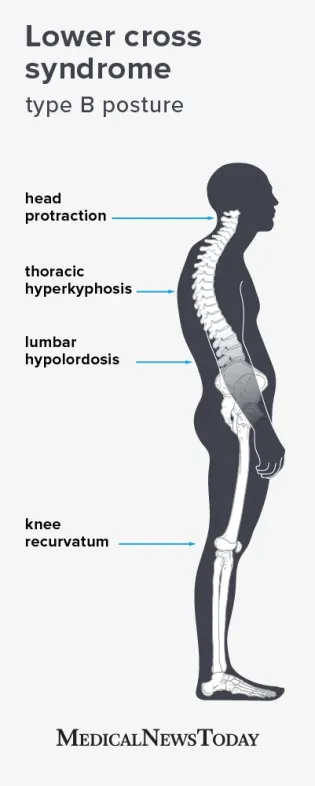
Type B: Anterior pelvic cross syndrome:
It is called ‘The Anterior Pelvic Crossed syndrome. The abdominal muscles are too weak and short in the type B posture. This is associated with a predominant flexor activity.
So that the hyperlordosis of the lumbar spine, a hyperkyphosis of the thoracic spine, and protraction of the head. The pelvis is anteriorly and the knees are in a hyperextension position(knee recurvatum).
Who are at Risk of Developing Lower Cross Syndrome?
The risk factors for developing Lower Cross Syndrome (LCS) can vary from person to person, but some common factors that contribute to its development include:
Sedentary lifestyle: Prolonged periods of sitting or inactivity can lead to muscle imbalances and tightness, particularly in the hip flexors. People who have jobs or lifestyles that require long hours of sitting may be at a higher risk.
Poor posture: Maintaining poor posture, such as slouching or sitting with an excessive curvature in the lower back, can contribute to LCS. Poor posture can result from habits, structural abnormalities, or muscle weaknesses.
Lack of exercise or physical activity: Inadequate physical activity or a lack of regular exercise can weaken the gluteal and abdominal muscles, which are essential for maintaining proper alignment and stability in the lower back and pelvis.
Muscle imbalances: Imbalances between opposing muscle groups can increase the risk of LCS. For example, if the hip flexors are consistently tight and overactive while the gluteal and abdominal muscles are weak and underactive, it can lead to the development of LCS.
Previous injuries or surgeries: Previous injuries or surgeries involving the lower back, hips, or pelvis can disrupt the normal muscle balance and contribute to LCS. For instance, a history of low back pain or hip-related issues may increase the likelihood of developing LCS.
Genetic factors: Some individuals may have a genetic predisposition to certain muscle imbalances or structural abnormalities that make them more susceptible to developing LCS.
Occupational or sports-related factors: Certain occupations or sports activities that involve repetitive movements, prolonged standing, or excessive stress on the lower back and hip muscles can increase the risk of LCS. Examples include jobs that require lifting heavy objects or sports that involve running or jumping.
It’s important to note that these risk factors do not guarantee the development of LCS, and individuals may experience the condition even without these factors. Additionally, the presence of risk factors does not necessarily mean that LCS will occur. Engaging in regular exercise, maintaining good posture, and seeking treatment for any underlying issues can help reduce the risk or alleviate the symptoms associated with LCS.
What dysfunctions are associated with Lower Crossed Syndrome?
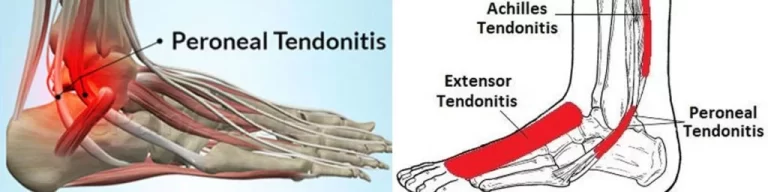
The lower cross syndrome can affect joint function and contribute to dysfunction everywhere throughout the kinetic chain of movement. It can impair function at the SI joint, L4-L5, L5-S1, and hip joints where the pattern crosses. It can also cause low back pain, iliotibial band syndrome, knee discomfort, ankle dysfunction, and plantar fasciitis.
When to see a doctor?
If a person has persistent lower back pain, they should consult a doctor. It could be caused by LCS or one of a number of other underlying disorders. This has the potential to induce lower back pain. Before beginning any new workout program, especially one that intends to assist rectify a person’s posture, it is also a good idea to consult with a doctor.
Diagnosis
Lower Crossed Syndrome Examination:
A lower cross syndrome is diagnosed using a variety of ways. A physical examination as well as specialised evaluations may be conducted to diagnose this condition.
The doctor will analyze your static posture during the physical examination, assessing whether you have an arched lower back and slanted shoulders.
The doctor checks the pelvis position. There is usually an increase in anterior tilting of the pelvis. It is also associated with increased lumbar lordosis.
Check the shape, size, and tone of the tightened or inhibit muscles.
Active examination:
Hip extension movement – It is examined to check the hyperextension phase of the hip during gait. Use lift the straight leg.
Hip abduction movement –The patient with LCS, will combine movement of the abduction with lateral rotation and flexion of the hip.
Trunk curl-up movement– It is tested to the interplay between the strong iliopsoas and the abdominal muscles.
Other special assessments are the following:
Overheard Squat:
In this assessment observe the lower back arch position.
when the patient does squat the lower back arch increase and the patient also do excessive forward bending during squatting.
Single-Leg Squat:
While performing a single leg squat, the doctor will see your trunk rotation and forward lean.
The doctor also observe the patient’s knee position, during this movement knee went into a valgus position in the LCS patient.
Pushup:
During the pushup assessment, the doctor will see an increase in the lower back arch and hip drops to the floor, this sign can indicate lower crossed syndrome.
Treatment of lower cross syndrome:
Medical treatment:
If the patient’s pain is severe, a doctor gives analgesics or a counter pain reliever and advises applying hot and cold packs on the affected area.
Patients should take medicine which is suggested by the doctor for lower back pain, any other kind of medicine should avoid.
For the LCS treatment mostly the exercise should effective to relieve the pain and strengthen the muscle which is tight and weak or affect in this condition.
Physiotherapy treatment in Lower Cross Syndrome:
The goal of treatment is to correct the person’s posture by retraining the muscular groups that cause this issue.
A therapist gives general guidance and creates an effective program for the person. The therapist gives the stretching exercise program by the use of instruments like foam roller or lacrosse, another is core stabilizing exercise and strengthening exercise.
The patient uses a foam roller or lacrosse ball for the exercise. Both things can help reduce muscle tension, especially with tight hip flexors. Depending on the degree of your injury or discomfort, you should always check with your doctor about the best treatment for you.
Relaxing technique for the muscles:
The muscle relaxation program is done by the use of Foam rollers and lacrosse balls. Foam rollers and lacrosse balls are popular tools when the muscles are imbalanced.
For example, they use a foam roller that patients roll over specific areas in the body. Once the patient found a specific tender area, the patient keeps the roller on that spot for 30 seconds or more. This exercise aims to reduce muscle tension.
Stretching Exercise:
A tight muscle should be released by the stretching technique. Stretching of particular tight muscles results in an increase in the strength of inhibited antagonistic muscles, worked by Sherrington’s law of reciprocal innervation.
This technique involves purely soft tissue which is repeatedly lengthened and relaxed. Stretch the specific muscle for a duration of 30 seconds and 3 repetitions. A five-week active stretching program effectively increases active and passive ROM in the lower extremity.
Iliopsoas muscle stretching:
The patient is in a kneeling position with the back in line with the buttocks and knees.
Place one leg in front of you, knee bent, foot flat on the ground, and toes facing forward.
Lean forward into a lunge position until you feel a gentle stretch in your hip flexor.
Hold the stretch for 15-30 seconds before repeating with the opposite leg.

Self-stretching of hip flexor muscle:
Erector spinae muscle stretching:

The patient is supine in the fetal position, knees to chest, arms wrapped over their knees, Exhale and stretch. Hold this position for 30 seconds.
This technique gives the norms of the imbalance of activity or functions in the body. These are the following:
- Reduce the detector points and remove muscular adhesions. Perform myofascial release and detector-point massage to the gluteus muscles, iliopsoas, and tensor fasciae latae muscle.
- recovering the normal lumbar flexion mobility
- Core exercises to strengthen the weak abdominal muscles.
- Re-education of posture and body operation.
- Retraining patient with Posterior Pelvic Crossed syndrome.
Activating and strengthening the muscles:
The patient performs a strengthening exercise with some resistance or little weight. The patient should hold these positions for 2 seconds and perform 10–15 repetitions for 1–2 sets.
Examples of some stretches which are performed in an activity are the following:
Bridge position:

In a supine position, the knees are bent, and the feet are flat on the floor. Keep the heels away from the buttocks. Extend the arms, shoulder relax, and fingers toward the feet.
Then lift the pelvis into the air or pelvis up from the surface, and make a straight line with the knees, pelvis, and shoulders.
Hold the position for a few seconds and perform it 10–15 times.
In this position, any type of external resistance is not required.
Quadruped hip extensions:

In this position the hands under the shoulders, the knees under the hips, and the neck in line with the spine.
Stretch the right arm and left leg, and the left hand and right foot against the ground.
Once you are balanced, raise your outstretched right arm and left leg until they are both parallel to your back.
The person must hold this before returning to the starting position and completing the repetitions.
The person performs this movement for at least 2 sets and 10 repetitions per set, holding the extension for 2 seconds.
Core stabilizing exercises:
Its aim is to help activate your underactive muscles. That includes the glute bridge, bird dog, and plank.
Lower Cross Syndrome Massage Treatment
Massage therapy can be a beneficial adjunct treatment for Lower Cross Syndrome (LCS) to help alleviate muscle tightness, reduce pain, improve circulation, and promote relaxation. When considering massage treatment for LCS, it’s important to work with a qualified and experienced massage therapist who is familiar with the condition. Here are some massage techniques that may be used to address LCS:
Swedish massage: This is a gentle and relaxing massage technique that involves long, gliding strokes, kneading, and circular motions. Swedish massage can help improve circulation, reduce muscle tension, and promote relaxation throughout the body.
Deep tissue massage: Deep tissue massage focuses on applying firm pressure and targeting the deeper layers of muscle tissue. It can help release chronic muscle tension, break up adhesions, and improve mobility. The massage therapist may focus on areas of tightness, such as the hip flexors and lower back muscles, to help alleviate muscle imbalances associated with LCS.
Myofascial release: Myofascial release is a technique that aims to release restrictions and tension in the fascia, the connective tissue that surrounds and supports the muscles. The massage therapist applies gentle sustained pressure and stretches to the fascia, helping to improve flexibility, reduce pain, and restore proper alignment.
Trigger point therapy: Trigger points are hyperirritable knots within muscle fibers that can refer pain to other areas of the body. Massage therapists can locate and apply pressure to these trigger points to release tension and alleviate pain. Trigger point therapy can be effective in targeting specific areas of muscle tightness commonly found in LCS, such as the hip flexors and gluteal muscles.
How might yoga work in lower-crossed syndrome?
Yoga can help to improve the flexibility of the body by lengthening muscles and retraining long and weak muscles to become active again. if you have the low back syndrome in yoga, pay attention to lengthening the hip flexors and hamstrings to balance the tension in the pelvis in the direction of forward-backward.
If you have lengthened these muscles, yoga can help you regrow previously long muscles. You can help the muscle-building process activate, stabilize and re-support.
Activating a muscle is not the same as strengthening it, at least not by any means. ie. add short stretch muscles on top of the pattern where is already unbalanced, we just add a more complex overall imbalance. First, lengthen the short muscles. Then use functional movement activities like yoga that help retrain previously long muscles to actively support different body movements.
How to Prevent Lower Cross Syndrome?
If a person lives a sedentary lifestyle, they should not do more physical activity in their daily routine. so that they can note the following advice to prevent back pain and lower cross syndrome.
For example, a person might take a break from sitting every half-hour or every hour, stand while you work at the standing desk, or get a simple workout before or after your day’s work. Practice good form and posture, and frequently do the movement of underactive muscles.
Summary
Lower Cross Syndrome (LCS) is a postural imbalance characterized by tight hip flexor muscles and weak gluteal and abdominal muscles. It can lead to lower back pain, hip and groin pain, poor posture, and reduced stability and functional movement.
To prevent LCS, it is important to maintain good posture, engage in regular exercise to strengthen core and hip muscles, stretch regularly, and take frequent breaks from sitting. Practicing ergonomics, avoiding prolonged static positions, listening to your body, and maintaining a healthy weight are also beneficial.
If LCS symptoms arise, seeking appropriate treatment such as physiotherapy, which may involve manual therapy, stretching exercises, strengthening exercises, postural retraining, and education on self-management, can help address the condition effectively.
FAQs
What causes lower cross syndrome?
Lower cross syndrome occurs due to an imbalance in muscular strength in the hip, lower back, and pelvis. Typically, this happens when the hip flexors, the adductor muscles, the upper and lower back extensor muscles, and the calves are overactive and tight.
What is the difference between lower-crossed and upper-crossed syndrome?
The upper cross syndrome refers to the upper part of the body, including the neck/upper back/chest/shoulder areas. The lower cross syndrome refers to the lower part of the body surrounding the pelvis/lower back/abdominal/upper thigh areas.
Which exercises are best for lower cross syndrome?
The following exercises are best to cure the Lcs and release the symptoms.
Pelvic Tilt Exercises.
Squat Exercises.
Bridge Exercises.
Plank Exercises.
Quadricep Stretch Exercises.
Lunge Stretch Exercises.
Hip Flexor Stretch Exercises.





2 Comments