Knee Mobilization exercise
Table of Contents
What is Mobilization for the knee joint?
- Knee Mobilization is a passive, skilled, manual therapy approach applied to joints and related to the soft tissue at various speeds and amplitudes taking physiological or accessory movement for therapeutic purposes
- small amplitude force applies at a fast velocity, and a large amplitude force applies at to slow velocity
- it is a manual technique that includes appealing to the target forces on a painful, stiff or otherwise negotiated jointly with regard to improving its overall function. Which is not appropriate in all situations, joint mobilizations help improve the range of motion, reduce pain, and reduce stiffness.
- Knee Joint mobilization is a hands-on treatment that is frequently executed by physical therapists healthcare professionals who specialize in rehabilitation for movement disorders and chiropractors, health professionals treating disorders of the musculoskeletal system that involve bones, muscles, and soft tissue
Introduction of knee joint
- The knee joint is a synovial joint that cemented three bones; the femur, tibia, and patella. It is a complex joint hinge variety composed of two fabrics; the tibiofemoral and patellofemoral. The tibiofemoral joint is a connection between the tibia and the femur, while the patellofemoral joint is a connection between the patella and the femur.
- The knee joint is the largest and feasibly the most tensed joint in the body. The arrangement of the bones in the joint provides a fulcrum that converts the actions of the flexor and extensor muscles of the knee. The structure of the extracapsular and intracapsular ligaments, as well as extensions of muscles that encompass the knee joint, provide the much-needed stability that counters the significant biomechanical stress brought upon the joint. As a hinged joint, the knee joint primarily permits movement along one axis in terms of flexion and extension of the knee in the sagittal plane. It also permits slight medial rotation during flexion and the last stage of extension of the knee, as well as lateral rotation when “unlocking” the knee.
- Tibiofemoral joint: Synovial hinge joint; uniaxial
- Patellofemoral joint: Plane joint
The articular surface of the knee joint
The tibiofemoral joint
- The tibiofemoral joint is cemented in the middle of the lateral and medial condyles of the distal end of the femur and the tibial plateaus, both of which are covered by a thick layer of hyaline cartilage.
- The lateral and medial condyles are two bony considerations positioned at the distal end of the femur, which have a smooth convex surface, and are separated posteriorly by a deep groove termed the intercondylar fossa. The medial condyle is larger, more narrow, and further considered than its lateral counterpart, which accounts for the angle between the femur and the tibia. The roughened outer surfaces of the medial and lateral condyles are termed medial and lateral epicondyles, respectively. Along the posterior aspect of the distal femur, there are paired rough elevations overhead the medial and lateral epicondyles addressed as the medial and lateral supracondylar ridges.
- The tibial plateaus are the two slightly concave superior surfaces of the condyles positioned at the proximal end of the tibia and are separated by a bony protuberance termed the intercondylar eminence. The medial tibial cemented surface is somewhat oval-shaped along its anteroposterior length, while the lateral articular surface is more circular in shape
- The cemented surfaces of the tibiofemoral joint are generally in conflict so compatibility is determined by the medial and lateral meniscus. These are crescent-shaped fibrocartilaginous structures that permit a more even distribution of the femoral pressure on the tibia
The patellofemoral joint
- The patellofemoral joint is a saddle-variety joint established by the fabrication of the patellar surface of the femur (also termed the trochlear groove of the femur) and the posterior surface of the patella. The patellar surface of the femur is a canal on the anterior side of the distal femur, which extends posteriorly into the intercondylar fossa.
- The patella is a triangular-shaped bone, with a curved proximal base and a considerable distal apex. Its articular surface is determined by medial and lateral facets which are concave cemented surfaces covered with a thick layer of hyaline cartilage and separated by a vertical ridge. Medial to the medial facet is a third minor facet, termed the ‘odd’ facet which deficiency of hyaline cartilage.
- Being a sesamoid bone, the patella is tightly inserted and held on behalf of the tendon of the quadriceps femoris muscle. On the distal part of the patella, an extension of the quadriceps femoris tendon configuration a central band termed the patellar ligament. It is a strong, thick ligament that elongates from the patellar apex to the superior area of the tibial tuberosity.
The joint capsule of the knee joint
- The joint capsule of the knee joint is of a compound nature, chiefly hammered by muscle tendons and their expansions, hammering a thick ligamentous sheath surrounding the joint. The capsule is relatively weak and connects to the margins of the femoral and tibial articular surfaces. The anterior portion of the capsule features an opening, whose margins connect to the borders of the patella. A second gap is also present in the lateroposterior portion of the capsule to give space to the tendon of the popliteus muscle.
- The capsule is hammered from an outer fibrous layer (which is continuous with adjacent tendons) and an inner synovial membrane that grease the cemented surfaces, decreasing friction along with providing nourishment to the cartilage. The joint capsule hammers several fluid-filled pouches termed bursae, that decrease friction within the knee joint. mention the bursa of the knee joint include the:
- Suprapatellar bursa – positioned superior to the patella between the femur and the tendon of the quadriceps muscle
- Prepatellar bursa- stay in front of the patella between the patella and the skin
- Infrapatellar bursa – positioned under the patella between the patellar ligament and the tibia
Ligaments of the knee joint
- The ligaments of the knee joint can be classified into two groups; extracapsular and intracapsular. These ligaments connect the femur and tibia, grasping them in place, giving stability, and inhibiting dislocation.
- Extracapsular ligaments are obtained outside the joint capsule and involve the patellar ligament, fibular (lateral) and tibial (medial) collateral ligaments, and oblique and arcuate popliteal ligaments. Intracapsular ligaments are obtained inside the joint capsule, with the cruciate ligaments being the most popular of this subgroup
Patellar ligament
- The patellar ligament is a strong, thick fibrous band that is a distal expansion of the quadriceps femoris tendon. It is found superficial/anterior to the infrapatellar bursa and expands from the apex of the patella to the tibial tuberosity.
- Along its outer edge, the patellar ligament combination with the medial and lateral patellar retinacula, which are an expansion of the vastus medialis and lateralis muscles, respectively, together with the overlying fascia. The patellar ligament plays the utmost role in stabilizing the patella and preventing its displacement.
fibular collateral ligament
- The fibular collateral ligament is a strong ligament that arises from the lateral epicondyle of the femur, just posterior to the proximal connection of the popliteus, and extends distally to connect on the lateral surface of the fibular head.
- As it connects to the fibular head, the ligament division of the tendon of the biceps femoris muscle is in two. The fibular collateral ligament is obtained deep in the lateral patellar retinaculum, and superficial to the tendon of the popliteus muscle, which divides the ligament from the lateral meniscus.
Medial (tibial) collateral ligament
- The tibial collateral ligament is the strong, flat ligament of the medial aspect of the knee joint. The tibial collateral ligament, along with its fibular counterpart, acts to protect the knee joint and inhibit excessive sideways movement by limiting external and internal rotation of the extended knee. The tibial collateral ligament has sometimes divided the literature into superficial and deep parts:
- The superficial part arises just proximal to the medial epicondyle of the femur. This ligament has two connection points; a proximal connection on the medial condyle of the tibia, and a distal connection on the medial shaft of the tibia. Anteriorly, the superficial part combined with the medial patellar retinaculum and the medial patellofemoral ligament, which courses from the medial femoral condyle to connect onto the medial border of the patella.
- Deep part: a vertical thickening of the knee joint capsule obtained at the bottom of the superficial part of the tibial collateral ligament. It arises from the area of the distal femur then connects to the medial meniscus, and terminates on the proximal tibia. These two parts of the ligament are termed meniscofemoral and meniscotibial ligaments
Oblique popliteal ligament
- The oblique popliteal ligament (Bourgery ligament) is an extension of the semimembranosus tendon which arises posterior to the medial tibial condyle and reverses superiorly and laterally to connect to the lateral condyle of the femur.
- As it spaces the intercondylar fossa, the oblique popliteal ligament emphasizes the posterior part of the joint capsule and connects with its central portion.
Arcuate popliteal ligament
- The arcuate popliteal ligament is a thick, fibrous band that arises on the posterior aspect of the fibular head and arches superiorly and medially to connect on the posterior side of the joint capsule of the knee joint. The arcuate popliteal ligament emphasizes the posterolateral part of the joint capsule, and combine with the oblique popliteal ligament, inhibits hyperextension of the knee joint.
Cruciate ligaments of the knee joint
- The paired cruciate ligaments gain their name as a result of the fact that they encompass each other obliquely within the joint in a way. They encompass the joint capsule but remain external to the synovial cavity. The cruciate ligaments are separated as follows:
- Anterior cruciate ligament: arises from the anterior intercondylar area of the tibia just behind the connection of the medial meniscus, and expands posterolaterally and proximally to connect on the dorsal part of the medial surface of the lateral condyle of the femur. As it encompasses the other side of the knee joint, the ligament passes the bottom of the transverse ligament and connects with the anterior horn of the lateral meniscus. The anterior cruciate ligament is important to prevent posterior rolling and displacement of the femoral condyle during flexion, along with preventing hyperextension of the knee joint.
- Posterior cruciate ligament: arises from the posterior intercondylar area of the tibia and expands anteromedially and proximally to connect to the anterior part of the lateral surface of the medial femoral condyle. This ligament is almost twice as strong and has a better blood supply than the anterior cruciate ligament. The posterior cruciate ligament has the adverse function of the anterior cruciate ligament, serving to prevent anterior rolling and displacement of the femoral condyle during extension, along with preventing hyperflexion of the knee joint.
Menisci of the knee joint
- The menisci are fibrocartilaginous crescent-shaped plates obtained between the articular surfaces of the femur and tibia and serve to provide their correspondence and shock absorption. The menisci are thick and circularized in their outer one-third part, while their inner two-thirds parts are thinner and avascular. the inner two-thirds parts contain radially formulated collagen bundles, whereas the outer third part consists of larger circumferentially arranged bundles. the inner portion is more fittable for weight-bearing and limiting compressive forces, while the outer portions are perfect for resisting tensional forces. The menisci are classified as follows:
- Medial meniscus: a C-shaped, almost semicircular fibrocartilaginous plate that looms over the surface of the medial tibial plateau. Its anterior horn connects to the anterior intercondylar area of the tibia and blends with the anterior cruciate ligament. Its posterior horn is connected to the posterior intercondylar area of the tibia, between the connection of the lateral meniscus and the posterior cruciate ligament.
- Lateral meniscus: an almost circular fibrocartilaginous plate that looms over the surface of the lateral tibial plateau. Its anterior horn also connects to the anterior intercondylar area of the tibia and partially in combination with the anterior cruciate ligament. Similarly, its posterior horn connects to the posterior intercondylar areas anterior to the posterior horn of the medial meniscus.
- The menisci are adhered in place by several ligaments, involving the transverse ligament, meniscofemoral ligaments, and meniscotibial (coronary) ligaments. By stabilizing the menisci, these ligaments are also indirectly included in inhibiting displacement of the knee joint.
- The transverse ligament connects the menisci anteriorly expanding from the anterior margin of the lateral meniscus to the anterior horn of the medial meniscus. Its definite role is uncertain but these ligaments stabilize the menisci during knee movements and decrease tension created in the longitudinal circumferential fibers.
- Meniscofemoral ligaments are the superior portions of the distal tibial collateral ligament expanding from the posterior horn of the lateral meniscus to the lateral aspect of the medial femoral condyle. They are classified into two ligaments; an anterior meniscofemoral ligament that courses anterior to the posterior cruciate ligament; and a posterior meniscofemoral ligament that runs posterior to the posterior cruciate ligament.
- Meniscotibial ligaments: are the inferior portions of the distal tibial collateral ligament, extending between the margin of the lateral meniscus and the peripheral area of the tibial condyles. It is constituted of a medial and lateral meniscotibial ligament.
- Patellomeniscal ligament: comprised of a medial and lateral patellomeniscal ligament, often called simply medial and lateral ligaments. These ligaments run from the inferior third of the patella to embed on the anterior portion of the medial and lateral meniscus
- Ligamentum mucosum: consists of two alar folds that connects onto the infrapatellar fat pad, grasping it in position. This structure is an embryonic remnant that divides the medial and lateral compartments of the knee.
- Popliteofibular ligament: positioned on the posterolateral aspect of the knee joint, expanding from the popliteus muscle to the medial aspect of the fibula.
- Fabellofibular ligament: arises from a small sesamoid bone on the posterior aspect of the lateral supracondylar ridge of the femur and inserts distally on the posterolateral edge of the styloid process of the fibula.
Nerve supply of the knee joint
- The knee joint achieves nerve supply from the femoral nerve, via the saphenous nerve and muscular branches. The joint also achieves contributions from the tibial and common fibular (peroneal) nerves and the posterior division of the obturator nerve.
Blood supply of the knee joint
- The knee joint has a rich vascularization stemming from the genicular anastomosis invented by several arterial blood vessels. There are roughly ten arteries included in the creation of genicular anastomosis:
- Descending branches of the lateral circumflex femoral artery, descending genicular branch of the femoral artery.
- Ascending branches of the circumflex fibular branch of the posterior tibial artery, anterior and posterior tibial recurrent branches of the anterior tibial artery.
- Branches of the popliteal artery are as follows lateral superior and inferior genicular arteries, the medial superior and inferior genicular arteries, and the middle genicular arteries.
Muscles and Movement acting on the knee joint
- Flexion is performed by Biceps femoris, semitendinosus, and semimembranosus; initiated by popliteus; assisted by gracilis and sartorius
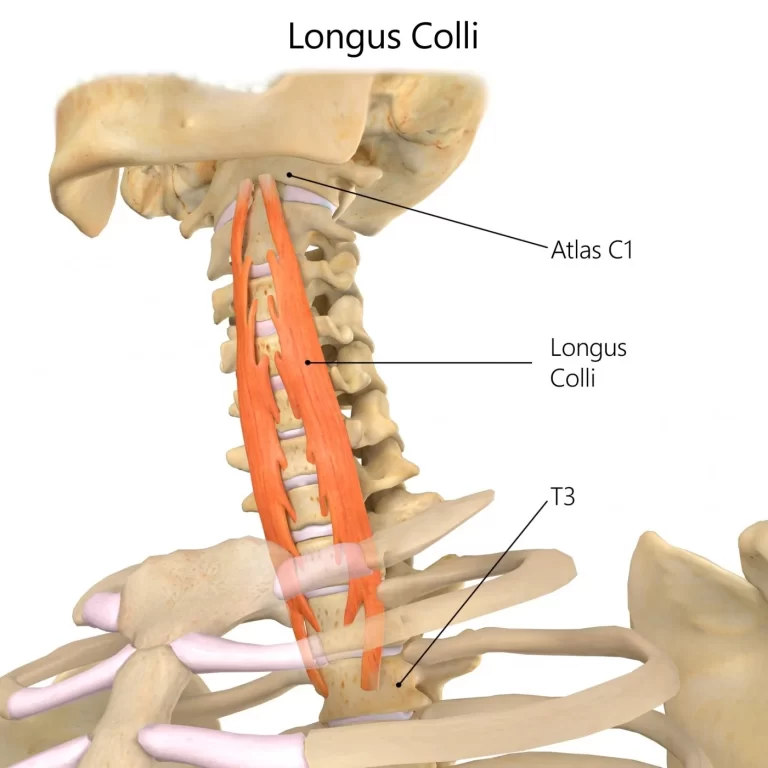
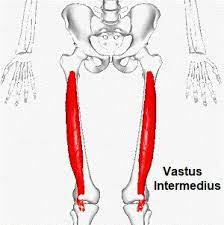
- The extension is performed quadriceps femoris (rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius) compensated by tensor fasciae latae
- Medial rotation is performed by Popliteus, semimembranosus, and semitendinosus, compensated by sartorius and gracilis.
- Lateral rotation is performed by the Biceps femoris
- The prime flexors of the knee joint are biceps femoris, semitendinosus, and semimembranosus, whereas popliteus triggers flexion of the “locked knee” and gracilis and sartorius help as weak flexors.
- The primary extensor of the knee joint is the quadriceps femoris, compensated by the tensor fasciae latae. Quadriceps femoris of four muscle bellies; rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius, all supplied by the femoral nerve.
The condition needs the mobilization of the knee joint
- chondromalacia patellae
- Osgood Schlatter
- osteoarthritis
- ACL tear
- patellofemoral pain syndrome
- patellar tendinitis
- knock knee
- bow legs
- genu recurvatum
- jumper’s knee
- sports injury
The surgical procedure needs mobilization of the knee joint
- total knee replacement
- ACL ligament repair
Goals for knee joint mobilization exercise
pain, muscle guarding, and spasm
- painful joint, reflex, muscle guarding, and muscle spasm can be treated with slight joint play techniques to stimulate neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and distraction movement are acclimated to stimulate mechano receptors that may inhibit the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- small amplitude distraction or gliding movement of the joint is used to cause synovial fluid movement, which is a vehicle for carrying nutrients to avascular portions of the articular cartilage
- rhythmic joint play techniques help to maintain nutrient exchange and prevent the painful and degenerating effects of statis when the joint is swollen or painful, and can not go through a range of motion
- when adapted to treat pain, muscle spasms, and muscle guarding these techniques should not place stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be mediated with progressively vigorous joint play stretching procedure to elongate hypermobile capsular and ligamentous connective tissue
- sustained or distraction stretch forces helped to distend the shortened tissue mechanically
Positional faults/subluxations
- A faulty position of one bony partner with regard to its opposing surface may outcome in limited motion or pain
- positional faults can occur with traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be conserve
- by maladapted neuromuscular control across the joint
- during attempting an active range of motion, faulty tracking of the joint surface results in pain or lessened motions
Progressive limitations
- diseases that progressively restrict movement can be treated with joint play techniques to maintain available motion or lessen the progressive mechanical reduction
- the patient’s response manner the dosage of distraction or glide to treatment and the state of the disease
Functional immobility
- when the patient can’t functionally locomote a joint for a longer period of time
- the joint can be treated with nonstretch gliding or distraction procedure to maintain available joint play and inhibit the degenerating and reducing effect of immobility
Grades of mobilization of the knee joint
Non-thrust oscillation techniques
- the oscillation could also be performed using physiological movement
- grade 1:small amplitude rhythmic oscillation is put at the start of the range, rapid oscillation like manual vibration
- grade 2:large amplitude rhythmic oscillation is completed within range, not reach the limit, perform 2 or 3 seconds for 1 to 2 minutes
- grade3:large amplitude rhythmic oscillation is initiated up to an available range of motion, stress into tissue resistance, perform 2 or 3 seconds for 1 to 2 minutes
- grade4:small amplitude rhythmic oscillation is executed at the available range of motion, the strain in tissue resistance, rapid oscillation like manual vibration
- grade 1 and a couple of are used to treat joint limitation of movement by pain or muscle guarding
- grade3 and 4 are useful for stretch maneuver
Nonthrust sustained joint play techniques
- This system interprets only joint play procedures that distribute (distract) or glide the joint surface
- grade 1(loosen): small amplitude distraction is applied when no stress is placed on the capsule, it equalizes cohesive force, muscle tension, and air pressure acting on joint
- grade2(tighten): limitless distraction or glide is applied to tighten the tissue surrounding the knee
- grade3(stretch): a distraction or glide is put with an amplitude large enough to place a stretch on the joint capsule surrounding the periarticular structure
- grade 1 distraction is given with all glide movements
- apply intermittent distraction for 7 to 10 seconds with some seconds of rest in between several cycles
- grade 2 distraction is useful to determine the sensitivity of the joint, once the joint reaction is understood treatment dosage increases and decreases
- gentle grade 2 distraction applied periodically won’t prevent pain and maintain joint play when ROM is not allowed
- grade 3 distractions or glides are needed to stretch joint structure, elevate joint play motion
- for limited joints apply a minimum of 6 seconds of stretch force followed by partial release (grade 1 or 2)
- reps:3 to 4-second intervals
Tibiofemoral mobilization
- resting position: 25-degree flexion
- treatment plane: the treatment plane is along the surface of the tibial plateaus, therefore it moves with the tibia as the knee angle change
- stabilization: the femur is stabilized with the belt or by the table
Tibiofemoral distraction

patient position
- sitting, supine, prone, or beginning with the knee in the resting position
- progress to positioning the knee at the limit of the range of motion of flexion or extension
- rotation of the tibia may be added prior to applying the traction force
- use an internal rotation at the end range of flexion and an external rotation at the end range extension
hand placement
- grasp around the distal leg, proximal to the malleoli with both the hands
mobilizing force
- pull on the long axis of the tibia to separate the joint surface
Tibiofemoral posterior glide

- patient position: supine with the foot resting on the table
- the position of the drawer test can be used to mobilize the tibia either anteriorly or posteriorly
- although grade 1 distraction can be applied with the glides in the supine position
Therapist position and hand placement
- sit on the table with your thigh fixating on the patient’s foot, with both hands grasped around the tibia, the finger pointing posteriorly and the thumb pointed anteriorly
mobilizing force
- extend your elbow and lean your body weight forward push the tibia posteriorly with the thumb
- tibiofemoral posterior glide is used for increased flexion
Alternate position
patient position

- sitting with the knee flexed over the edge of the treatment table, begin with the starting position
- progress to near 90-degree flexion with the tibia positioned in internal rotation
- when the knee flexes past 90 degrees position the patient to prone,
- place the small rolled towel proximal to the patella to minimize compression force against the patella during the mobilization
Therapist position and hand placement
- when in the resting position, stand on the medial side of the patient’s leg
- hold the distal portion with your distal hand and place the palm of your proximal hand along the anterior border of the tibial plateaus
- when reaching nearly 90 degrees, sit on a low stool, stabilize the leg between your knees
- place one hand on the anterior border of the tibial plateaus
- when prone position, stabilize the femur with one hand and place the other hand along the border of the tibial plateaus
mobilizing force
- extend your elbow and lean your body weight onto the tibia, gliding posteriorly
- when progressing medial rotation of the tibia at the end range of flexion
- the force is applied in a posterior direction against the medial side of the tibia
Tibiofemoral anterior glide

patient position
- prone lying, begin with the knee in the resting position
- progress to the end of the available range of motion
- place a small pad under the lower femur to prevent patellar compression
- the drawer test can also be used
- the mobilizing force comes from the finger on the posterior tibia as you lean backward
Therapist position and hand placement
- grasp the backside of the tibia with the hand closer to the tibia
- put the palm of the proximal hand on the posterior aspect of the proximal tibia
mobilizing force
- apply gliding force with the hand on the proximal tibia in an anterior direction
- the force may be directed to the lateral or medial tibial plateau to stabilize one side of the joint
Alternate position and technique
- if the patient can’t be positioned prone position him/her supine with a fixation pad under the tibia
mobilizing force
- placed the force against the femur in a posterior direction
Patellofemoral mobilization
Patellofemoral distal glide mobilization

patient position
- supine with knee extended progress to positioning at the end of the available range in flexion
Therapist position and hand placement
- stand beside the patient’s thigh facing the patient’s feet
- place the palmar space of the hand that is closer to the thigh around the superior border of the patella
- use the other hand for reinforcement
mobilizing force
- glide the patella in a backward direction, parallel to the femur
- do not press the patella into the femoral condyles while performing this glide
patellofemoral medial glide

patient position
- supine with the knee extended
- side lying perhaps used to apply a medial glide
Therapist position and hand placement
- place the heel of your hand along with the medial aspect of the patella
- stand on the opposite side of the treatment table to position your hand along the medial border and
- on the same side of the treatment, table to position your hand along the lateral border
- place the other hand below the femur to stabilize it
mobilizing force
- glide the patella in the medial direction against the restriction
Patellofemoral lateral glide

patient position
- supine with the knee extended
- side lying perhaps used to apply a medial glide
Therapist position and hand placement
- place the heel of your hand along with the lateral aspect of the patella
- stand on the opposite side of the treatment table to position your hand along the medial border and
- on the same side of the treatment, table to position your hand along the lateral border
- place the other hand below the femur to stabilize it
mobilizing force
- glide the patella in the lateral direction against the restriction
Tibiofibular joint mobilization
proximal tibiofibular anterior glide

- patient position: side-lying, with the trunk and hip rotated partially towards prone
- the top of the leg flexed forward so the knee and lower leg are relaxing on the treatment table or supported on a pillow
Therapist position and hand placement
- stand behind the patient, placing one hand under the tibia to stabilize it
- place the palm of your other hand posterior to the head of the fibula, wrapping your fingers anteriorly
mobilizing force
- apply the force against the palm of your hand against the posterior aspect of the fibular head in Antero lateral direction
- this glide is used to increase the movement of the fibular head to reposition a posteriorly subluxed head
distal tibiofibular anterior or posterior glide

- patient position: supine or prone
Therapist position and hand placement
- stand a the end of the treatment table, place the fingers of the more medial hand under the tibia and the thumb over the tibia to stabilize it
- place the palm of your other hand over the lateral malleolus with the fingers at the bottom of the lateral malleolus
Mobilizing force
- press against the fibula in an anterior direction when in the prone position and in a posterior direction when supine
Precaution for knee joint
- suspected cancer in the treatment area
- pregnancy
- after knee arthroplasty
- blood clotting therapy
- skin rash, wounds treatment area
- connective tissue disorder
- bone diseases
- long term use of corticosteroids
- Never cross your legs on sitting, standing, or lying down
- Avoid bending your operated leg beyond 90 degrees
- When sitting or standing in distinction to a chair, bed, or toilet you must ensure that extend your operated leg in front of you. Avert sitting on chairs that are too low, use a pillow if necessary
- do not cross your legs
- Do not ever bend, squat, or arrive for anything while taking shower. Use a shower sponge with a long handle and have someone wash the part of your body that is difficult for you to reach.
- assure you use a raised toilet seat. It will be more difficult to get up safely if the toilet seat is too low.
- When stair climbing upward, step first with the unaffected leg
- When descending, step first with the operated leg.
- assure you use your crutches or walker until your doctor or physiotherapist tells you it is OK to stop using them
- Do not lift up over the amount of weight your doctor or physical therapist advice you to lift on the operated knee
Hypermobility
- the joint of a patient with probable necrosis of the ligaments or capsules should not be mobilized with stretching techniques
Joint effusion
- the joint effusion due to trauma or disease
- rapid swelling of the joint generally points out bleeding in the joint and may occur with diseases aspiration of the blood to lessen the necrotizing effect on the articular cartilage
- slow swelling for more than 4 hours generally points out serious joint effusion or edema on the joint due to mild trauma irritation or disease such as arthritis
- do not stretch the inflamed joint with mobilization because the capsule is already stretched by being expanded to accommodate the extra fluid
- the limitation of motion is in distinction to extra fluid and muscle response to pain, not from shortened fibers
- gentle oscillating motion that does not stress or stretches the capsule may help to block the transmission of a pain stimulus so it is not perceived and may help to accelerate fluid flow while maintaining available joint play movement
- if the patient’s response to slight techniques is increased pain or joint irritability
- the techniques were applied too strenuously or should not be done with the current state of pathology
Inflamation
- whenever inflamation is present, stretching elevate pain, and muscle guarding result in greater tissue damage
- gentle distraction movements may temporarily decrease the pain response
FAQS
- How much time is taken for mobilization after total knee arthroplasty?
After 1 or 2 months of POP, mobilization is applied because the synovium formation of bone takes time to attach the bone
- When do we use joint mobilization for the knee?
The main goal of joint mobilization of the knee is to regain the normal joint play movement that might have been a concession by damage or injury. Normal movement of the affected joint will be regained faster if it is concession early in the treatment program. Also, mobilization is beneficial in cases when the range of motion is the not presence
- Why is early mobilization important after an injury?
In patients with acute limb injuries, early mobilization decreases pain and swelling and improves functional outcomes correlated with cast immobilization
- How long do you do joint mobilization for the knee joint?
Typical treatment of a knee joint may add a series of three to six mobilizations carried on up to 30 seconds, with one to three oscillations or glide per second
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation is start within range, not reaching the limit of movement, apply the glide for 2 or 3 seconds for 1 to 2 minutes
that passes center way into the joint range of motion, attending any part of the range and yet not reaching the end range. This technique can be given to treat joint stiffness by accelerating the range of motion and joint pain