Jacobsen Syndrome
Table of Contents
What is the Jacobsen Syndrome
Jacobsen Syndrome is a rare genetic disorder caused by the deletion of genetic material from the end of chromosome 11 (11q deletion disorder). It is characterized by developmental delays, intellectual disabilities, distinctive facial features, bleeding disorders (due to platelet dysfunction), heart defects, and growth delays.
The severity of symptoms can vary, and the condition is typically diagnosed through genetic testing. Supportive therapy and early treatment can help control symptoms and enhance quality of life.
- An uncommon chromosomal condition known as Jacobsen syndrome is caused by the loss of genes from chromosome 11, which contains band 11q24.1. This condition is congenital. The condition is also known as 11q terminal deletion disease since the loss occurs on the q arm of chromosome 11. There might be anywhere between 5 million and 16 million DNA base pairs removed. The amount of deletions determines how severe the symptoms are; the more deletions, the more severe the symptoms are likely to be.
- Serious intellectual difficulties, Dysmorphic features, delayed development, and a host of medical issues, including heart anomalies, are all present in people with Jacobsen syndrome. Nearly 88.5% of individuals with Jacobsen syndrome have Paris-Trousseau syndrome, a bleeding disease.
Signs and Symptoms
- Intellectual difficulties, which vary from mild to moderate depending on the number of chromosomal gene deletions, affect nearly all children with Jacobsen syndrome. Simple tasks like sitting, standing, and walking are challenging for the majority due to delayed development, which includes delayed speech, motor impairments, and lack of coordination. The majority of kids ultimately begin talking, although language usage is severely limited in people with significant intellectual disabilities.
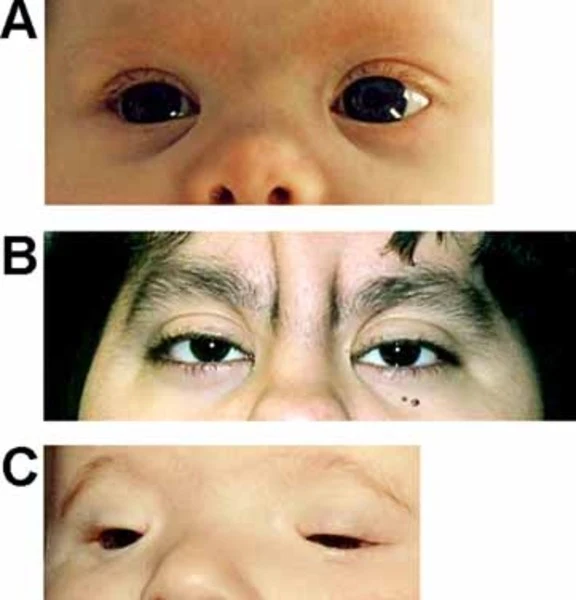
They have unique facial characteristics such as:
- tiny head, or microcephaly
- forehead that is pointed (trigonocephaly)
- Low-set ears that are little
- Eyes spread far apart (hypertelorism)
- Eyelid drooping (ptosis)
- wide nasal bridge
- Extremely narrow lips
- The mouth’s down-turned corners
- Children with Jacobsen syndrome are very likely to have heart defects
88.5% of those with the disorder have Paris-Trousseau syndrome, a bleeding disorder that causes abnormal bleeding and bruising to occur throughout life due to platelet dysfunction; other symptoms may include eye problems, ear and sinus infections, hearing problems, bone deformities, growth hormone deficiency, gastrointestinal issues, kidney malfunctions, etc. Some children also have behavioral issues such as distractibility, hyperactivity, impaired communication, and social skills, which qualify them for an ASD and ADHD diagnosis.
Cause
- Genetic material from the long arm of chromosome 11 is deleted in Jacobsen syndrome. Although the number of deletions may differ from patient to patient, it usually happens at the end terminal of chromosome 11’s q arm. The deletion might take place in one of three ways:
- De novo deletion is a chance occurrence that occurs when genes from chromosome 11 are erased during the development of the sperm, egg, or cell division in the embryonic stage.
- In this situation, a parent with a balanced translocation or another kind of chromosomal rearrangement may pass these genes on to their offspring, leading to an even more unbalanced translocation. Along with some additional genetic material from another chromosome, the impacted offspring have deletions on chromosome 11.
- Ring chromosome 11: in this instance, the genetic material from the chromosome’s long and short arms is removed, and the remaining portion combines to form a shape resembling a ring. In this case, the affected individual would have symptoms linked to 11q and 11p deletion.
What are the risk factors for Jacobsen Syndrome?
The specific risk factors for Jacobsen Syndrome are still unclear since the disorder arises from a spontaneous loss during cell division. However, it’s important to remember the following:
- Five to ten percent of individuals with the hereditary type of the syndrome may be at higher risk if they have a family history.
- Given that around 65% of people with Jacobsen Syndrome are thought to be female, being a woman may be considered a risk factor for the condition.
- It is important to realize that simply possessing a risk factor does not ensure that the ailment will manifest. One is more likely to acquire a disease than someone without a risk factor. Different risk factors are more or less important.
How is Jacobsen Syndrome diagnosed?
- In certain situations, diagnosing Jacobsen syndrome might be challenging. This is because it is an uncommon and inherited disorder. To establish a diagnosis of Jacobsen syndrome, genetic testing is required.
- Magnified chromosomes are examined under a microscope during genetic testing. To make them look like a “barcode,” they are discolored. You will be able to see the broken chromosome and the removed genes.
- During pregnancy, Jacobsen syndrome can be identified. Additional tests might be performed if an ultrasound reveals anything unusual. The mother might have a sample of her blood drawn and examined.
Differential Diagnosis
- Some of the clinical symptoms of children with Jacobsen Syndrome are shared with Turner and Noonan syndrome, such as a short and broad neck, small height, ptosis, pulmonary or aortic stenosis, and down-slanting palpebral fissure.
- Because of their short stature, unusual palpebral fissures, mental retardation, and finger pads, some children with JS have been clinically diagnosed with Kabuki syndrome.
Medical Management
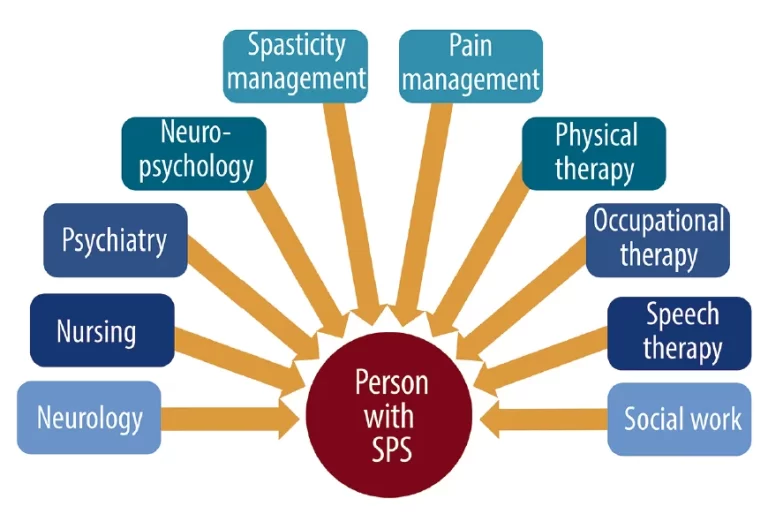
- A multidisciplinary team of a pediatrician, cardiologist, neurologist, physical therapist, ophthalmologist, and others must conduct a thorough assessment following diagnosis. JS-diagnosed newborns frequently need extra care and support. Drugs can be used to treat platelet abnormalities and heart defect consequences.
- Surgery may also be necessary for children with JS, particularly if they have heart abnormalities, and preoperative evaluation of hematologic problems is necessary.
Physiotherapy Management
Children with Jacobsen syndrome (JS), a chromosomal condition, will exhibit delayed motor and verbal milestones as well as overall developmental abnormalities. To overcome motor developmental impairments, individuals with JS should be sent to physical and/or occupational therapy for early intervention. Children with JS can benefit from physical therapy by becoming more mobile and coordinated.
Each child’s unique movement expression and potential to increase their movement efficiency should be evaluated throughout physical therapy. Because treatment must constantly adjust to the individual’s growth, it cannot be monotonous or stereotypical.
It has been demonstrated that including play in neurodevelopmental therapy (NDT) improves developmental delay in several ways. By offering suitable, interesting tasks, NDT may enhance cognitive and perceptual abilities and serve as a stimulant for typical movement patterns.
For a play activity to be effective, children must be adapted to action. That includes:
- Modifying the material’s size, shape, and consistency.
- adjusting the play activity’s protocol and guidelines.
- repositioning the youngster and the materials.
- regulating the level of communication between people. To accommodate the child’s evolving demands, the cognitive demand must be reduced if the motor demand is strong.
How can Jacobsen Syndrome be prevented?
- There are presently no recognized prevention strategies or guidelines for Jacobsen syndrome because it is a hereditary disorder.
- Prenatal diagnostics, which includes genetic testing of the expectant parents (and their near relatives) and molecular testing of the fetus during pregnancy, may help individuals better understand the hazards of pregnancy.
- If there is a family history of the issue, genetic counseling will assist in assessing risks before pregnancy.
Complications:
- A dangerous yet frequent side effect of Jacobsen syndrome is platelet problems, such as Paris-Trousseau Syndrome.
- Heart disorders: anomalies on the left side of the heart, hypoplastic left heart syndrome, gaps between the left and right lower chambers
- Kidney problems: having a single kidney, twin ureters (the tubes going from the kidneys to the bladder), hydronephrosis, or swollen cysts
- Because of a constricted or obstructed passageway from the stomach to the intestines, gastrointestinal disorders such as pyloric stenosis result in violent vomiting. Additional issues include constipation, intestinal blockage, narrowed or obstructed anus, missing GI tract segments, and irregular gut placement.
- Cataracts
- Sinus and ear infections
FAQ
What are Jacobsen Syndrome Symptoms?
A broad nasal bridge, down turned corners of the mouth, a thin upper lip, a short lower jaw, small and low-set ears, widely set eyes (hypertelorism) with drooping eyelids (ptosis), and skin folds covering the inner corner of the eyes (epicanthal folds) are some examples.
What causes Jacobs Syndrome?
The most prevalent cause of Jacobs syndrome, which is not inherited, is an extra Y chromosome in the resulting sperm that occurs during the father’s meiosis II. 46, XY/47, XYY mosaicism is a different and less prevalent type of this disease that develops in the early stages of embryonic development.
Is Jacobsen Syndrome a disability?
A rare genetic illness primarily characterized by craniofacial dysmorphism, congenital heart disease, intellectual disability, Paris Trousseau bleeding disorder, structural kidney problems, and immunodeficiency is caused by deletions in the long arm of chromosome 11 (11q).
Is Jacobsen Syndrome male or female?
both prevalence and incidence. There are now about 200 occurrences of Jacobsen syndrome globally, making it a rare hereditary disease. According to estimates, the prevalence of JS is 1 in 100,000 infants, with a 2:1 female-to-male ratio.
How is Jacobsen Syndrome detected?
During pregnancy, Jacobsen syndrome can be identified. Concerns may arise from an early pregnancy ultrasound scan that reveals, for instance, nuchal thickness (at the back of the neck), and subsequent abnormality scans may reveal heart or kidney issues. Additionally, oligohydramnios, a low amount of amniotic fluid, has been discovered.
References
- Wikipedia contributors. (2025, February 9). Jacobsen syndrome. Wikipedia. https://en.wikipedia.org/wiki/Jacobsen_syndrome
- Gotter, A. (2017, July 9). Jacobsen Syndrome. Healthline. https://www.healthline.com/health/jacobsen-syndrome#causes
- Gotter, A. (2017, July 9). Jacobsen Syndrome. Healthline. https://www.healthline.com/health/jacobsen-syndrome#causes
- https://www.physio-pedia.com/Jacobsen_Syndrome
- Gupta, N. (2023, May 1). Jacobsen Syndrome: Symptoms, causes, diagnosis, and treatments – Jaipur Hospital. Jaipur Hospital. https://jaipurhospital.in/jacobsen-syndrome/
- Gupta, N. (2023b, May 1). Jacobsen Syndrome: Symptoms, causes, diagnosis, and treatments – Jaipur Hospital. Jaipur Hospital. https://jaipurhospital.in/jacobsen-syndrome/