Iliopsoas Tendonitis
Table of Contents
What is a Iliopsoas Tendonitis?
- This iliopsoas muscle is the strongest hip flexor and assists in the external rotation of the femur, playing an important role in maintaining the strength and integrity of the hip joint and also acting as a stabilizer of the lumbar spine and pelvis. Pathologic conditions of the iliopsoas have been shown to be a significant cause of hip pain and dysfunction and include asymptomatic snapping hip syndrome, tendonitis, bursitis, or impingement. Additionally, conditions related to the iliopsoas muscle have been implicated in lumbopelvic disorders, such as low back or gluteal pain, intense groin pain particularly in the athletic population, or even anterior thigh and knee pain.
- Iliopsoas tendinopathy refers to a condition that affects the insertion of the muscle on the femur or can occur with repetitive hip flexion and other deficits of the biomechanical system resulting in chronic degenerative changes of this tendon. Due to the close proximity of the Iliopsoas tendon or the related bursa, inflammation of one of these structures inevitably causes inflammation of the other. The iliopsoas tendinitis or iliopsoas bursitis is commonly described synonymously, as the clinical presentation, evaluation, and management are nearly identical.
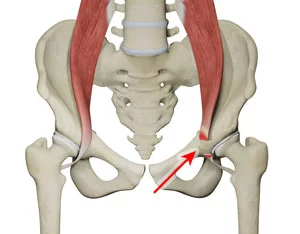
Clinically Relevant Anatomy:
The iliopsoas muscle complex is made up of three muscles that include the iliac, psoas major, and psoas minor.
- Origin: The iliopsoas muscle has its origin in the fusion of the psoas major and muscles. This fusion occurs at the level of L5-S2, and both muscles pass from the pelvis to the thigh under the inguinal ligament.
- Insertion: This iliopsoas muscle inserts into the lesser trochanter of the femur to the psoas tendon.
- Bursa: The longest bursa of the hip joint is the iliopsoas bursa which is located deep in the iliopsoas musculotendinous junction and anterior to the hip joint capsule. This bursa has been reported to communicate with the hip joint in ~15% of patients.
- Innervation: femoral nerve branch of the lumbar plexus (psoas part).
- Vascular supply: Iliolumbar artery or medial femoral circumflex artery.
- Function: Flexor of the thigh or trunk; Assists in external rotation of the femur; and Lateral flexor of the lower vertebral column.
Epidemiology:
- In common iliopsoas pathologic conditions, such as tendinitis, bursitis, snapping, and impingement, have been deemed to be the main cause of chronic groin pain in roughly 12-36% of athletes or in 25-30% of athletes with acute injury to the groin region.
- Most commonly present in kicking athletes such as soccer players, however, it may also occur in the nonathletic population The commonly reported effect young adults (the peak age group is in the 30s) Mildly many prevalent in females.
What is iliopsoas?
- This iliopsoas is the of muscles: the psoas. These muscles join together to form a single tendon commonly referred to as the iliopsoas or “hip flexors”.
What are the hip flexors that cause hip snapping? Why is hip snapping?
- Yes! When the muscles are excessively tight, its tendon may rub and even produce an audible snapping sound when passing over the underlying bony landmarks (2-6). When painless, the condition is mostly termed “asymptomatic internal snapping hip”. When accompanied by pain and dysfunction, the condition is also known by a variety of terms, including; painful internal snapping hip, internal coxa, iliopsoas tendinitis, iliopsoas tendinosis, iliopsoas tendinopathy, iliopsoas bursitis, and iliopsoas syndrome.
Is it bursitis and tendonitis?
- The diagnoses of tendinitis or bursitis are essentially synonymous, as inflammation in one inevitably generates inflammation in the neighboring counterpart– with nearly identical presentation, evaluation, and treatment.
How does the iliopsoas tendonitis get irritated?
- The iliopsoas tendon can be irritated by either acute injury or repetitive micro-trauma. Acute injuries involving the hip or pelvis typically result from direct trauma. Like other tendinopathies, chronic injuries occur when repetitive microtrauma exceeds the body’s ability to repair itself.
How does iliopsoas tendonitis typically occur?
- Psoas tendinopathy often arises from the repeated flexion (bending) of an externally rotated hip joint (think toes pointed out).
What activities and sports contribute to iliopsoas tendonitis?
- This condition is commonly termed “dancer’s hip” and “jumper’s hip”, as movements associated with these activities predispose participants to injury. Psoas tendinopathy is particularly common in ballet dancers – with more than 90% reporting clicking and snapping. This condition is also seen in athletes who participate in resistance training, rowing, track, and field, running (especially uphill), soccer, gymnastics, and hurdling. Teens may be at greater risk during growth spurts due to the relative inflexibility of the hip flexors.
What are the Causes of Iliopsoas Pain?
- Iliopsoas tendinitis is predominately caused by repetitive hip flexion and overuse of the hip area, resulting in inflammation.
- Iliopsoas syndrome, on the other hand, is caused by a sudden contraction of the iliopsoas muscle, which results in a rupture and tear of the muscle, usually at the point where the muscle and tendon connect.
- Athletes at risk include runners, jumpers, and participants in sports that require a lot of kicking. Also at risk are those who participate in strength training or weight-lifting exercises that require a lot of bending or squatting.
Signs or Symptoms of Iliopsoas Tendonitis:
- The common signs or symptoms of iliopsoas tendonitis include:
- Initial Symptoms
- Anterior hip and groin pain associated with specific sports-related activities, such as running, jogging, or kickingAudible snap or click in the hip and groin
- Progressive Symptoms
- Hip and groin pain during simple day-to-day activities pain that radiates decreased from the anterior thigh towards the knee Pain even at rest.
Diagnosis:
Radiography
- Typically not indicated for soft-tissue disorders or findings are unremarkable in cases, however, radiographs may be used as an initial imaging study if another bony pathology is suspected (i.e., loose bodies, osteitis pubis, etc.) and in the presence of “red flags”.
- Slipped capital femoral epiphysis should be ruled out in a child and adolescent presenting with hip pain.
Ultrasonography
- Diagnostic ultrasound is a noninvasive and accessible option to evaluate muscles and tendon injuries. Findings typically reveal a thickened tendon. Iliopsoas bursitis is associated with an excessive amount of fluid in the iliopsoas bursa, which is usually visualized in the US. The US allows a dynamic view of the muscle, therefore will reveal any “snapping” of the tendon that may be present.
- The US is used for needle guidance with lidocaine and corticosteroid injections (discussed below). Not always an optimal test for diagnostic accuracy as this imaging is highly user-dependent.
Magnetic Resonance Imaging (MRI)
- MRI is the “criterion standard” when evaluating symptoms relating to the hip and pelvis.
- In one study that looked at imaging to determine the causes of hip pain in endurance athletes, radiographs, radionuclide bone scans, and MRI scans were compared. The results revealed the MRI report to be the most sensitive imaging modality.
- Provides the accurate assessment of the iliopsoas tendon and bursa.
MRI findings when evaluating musculotendinous injuries:
- Spin-echo T2-weighted images will show the increased signal intensity that is associated with swelling and inflammation. A musculotendinous injury of greater severity with associated hemorrhage will display high signal intensity with T1-weighted images and T2-weighted images.
Peritendinitis evaluation
- The issue will display improved fluid that is detected on the spin-echo T2-weighted images or short T1 inversion recovery (STIR) sequence as a focus of high-signal intensity surrounding a normal tendon.
- Tendinosis the spin-echo T1-weighted images will demonstrate improved signal intensity with the tendon that is associated with myxoid degeneration or proliferation. The spin-echo T2-weighted images may show abnormal signals (usually less than that seen on the T1-weighted images) or a normal signal.
Lidocaine Challenge Test
- This test is performed if the causes of your hip and pelvic pain are not quite clear. In this test, your doctor will inject a 1% lidocaine test into your hip joints, targeting the iliopsoas tendon under ultrasound guidance. you experience relief from the hip pain this confirms the diagnosis of iliopsoas tendonitis.
Differential Diagnoses:
- Hip labral tear
- Sports hernia
- Iliopsoas bursitis
- Inguinal hernia
- Osteitis pubis
- Abdominal muscle tendinopathy/strain
- Adductor tendinopathy/Groin injury
- Osteoarthritis
- Obturator nerve entrapment
- Neoplasm
- Other reported causes of anterior hip pain:
- Inflammatory synovitis
- Infection (septic joint)
- Crystal-induced synovitis (“gout”)
- Stress fracture of the femoral neck
- Avascular necrosis of the femoral head
- Tendon avulsion
- Muscle Contusion
- Femoral Acetabular Impingement (FAI)
- Rectus femoris strain
- Tight iliotibial band
- Referred from the lumbar spine (L1, L2)
- Myalgia paresthetica
- Slipped Capital Femoral Epiphysis (SCFE)
Treatment of Iliopsoas Tendonitis:
Conservative management
- Conservative management of psoas tendinopathy support relative rest, activity modification as well as exercises.
- Soft tissue techniques such as myofascial release may be useful to assist in reducing muscle tightness and may be beneficial due to the proposed neuromodulatory effect.
- Manual therapy for the mobilization of the hip capsule, lumbar spine, pelvis, and other joint mobility deficits.
- Range of motion, stretching, or strengthening exercises should target the hip flexors and antagonistic muscle groups.
Acute Phase
- The main objective of the first phase is to decrease pain symptoms, reduce muscle spasms or decrease any swelling. If the patient has stopped engaging in activities of daily living, getting the patient back to these activities is an important goal of this first phase.
- The acute rehabilitation phases include relative rest (avoiding any pain-provoking activities), ice, medication, or light stretching.
- Ice: Apply for only 20 minutes, every few hours for the first 1 to 3 days.
- Medication: The Short-terms course of non-steroidal anti-inflammatory drugs (NSAIDs).
- Gentle stretching will aid in reducing muscle spasms To avoid over-stretching, do not stretch soon after a period of icing as icing may increase the individual’s pain threshold, making them less sensitive to pain.
- The chosen iliopsoas stretches are held for 20 seconds, followed by 30 seconds of rest, and repeated five times. The stretch should remain pain-free at all times and the patients should bring their awareness to taking dull, deep breaths while holding the stretch.
Recovery Phase
The primary goals of the second phase are to restore range of motion (ROM), strength, endurance, and proprioception, and Eventually, sports-specific activity is included.
ROM (Range of Motion):
- The stretching routine for the iliopsoas complex is continued and engaging in the proper warm-up or cool-down with exercise is emphasized.
- Injury to the iliopsoas muscles may be associated with increased lumbar lordosis and anterior pelvic tilt. Achieving neutral
- postural can be worked on by stretching or strengthening the appropriate muscle groups.
Stretching:
- Stretching the rectus femoris helps to bring an anteriorly-rotated pelvis into more neutral positions. Doing so will take tension off of the iliopsoas muscles, decreasing the likelihood of strain or spasms.
- All stretches in this phase are held as described in the acute phase hold for 20 seconds, relax for 30 seconds, or repeat 5x.
Strengthening:
- The improved strength of the hamstring muscle group will increase the posterior force on the pelvis, decreasing the stress of the iliopsoas pulling on the pelvis anteriorly.
- Abdominal strengthening exercises should be performed with knees or hips flexed to 90 degrees will allow the iliopsoas to relax and the pelvis to remain neutral.
- Gluteus maximus strengthening also plays a role in achieving neutral positions of the pelvis.
- Strengthening exercise is performed continuously (4 sets of 10 to 15 repetitions).
Endurance training:
- Increased muscular endurance of the iliopsoas can be achieved over time with repetitive movements (hip flexion or external rotation of the femur) performed at a low resistance. Some examples include cycling, walking, and machine stair climbing.
- Endurance exercises should result in no pain, or there should be sufficient periods of rest between endurance training sessions. Eventually, the individual should work up to performing endurance sessions continuously, improving the duration of the activity.
Maintenance Phase
- Continue stretching the iliopsoas and rectus femoris muscle.
- Gradually increased resistance used with strengthening exercises (i.e., seated iliopsoas strengthening with ankle weight, supine hip flexion (straight leg raise) with ankle weight, seated external rotation strengthening with the ankle weight, seated external rotation with resistance band).
- Advancing strengthening exercises for the iliopsoas or the hamstrings – gradually progressing resistance can be achieved by either improving the number of repetitions performed or improving the weight, as tolerated by the individual.
- i.e., Standing hip flexion (machine), prone and seated hamstring curls (machine), advanced lunges with step-ups (lunges are
- performed at a slower pace ensuring a smooth and controlled rhythm).
Return to Sport (RTS)
- The patients should be asymptomatic, or able to tolerate pain before considering RTS.
- Range of motion, flexibility, or strength of the hip flexors and antagonist’s muscles should be restored to the level of the contralateral side.
- Sport-specific activities should be relatively pain-free.
Surgical Intervention
- Surgical interventions are considered when minimal improvement is achieved with a prolonged trial of the nonoperative
- management, which includes:
- At least 3 months of the dedicated conservative care plan including rest, activity modification, physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroid injections.
- There are only two surgical techniques reported in the literature which include either a completed or partial release of the iliopsoas tendon. commonly, good outcomes have been reported with procedures, including reducing pain and with no significant residual weakness
Prognosis
- With the correction of underlying biomechanical deficits, the overall prognosis is very good.
- Identifying these deficits early can play a role in preventing the development of chronic symptoms or However, as previously mentioned, diagnosis of iliopsoas tendinopathy is made approximately two years after the development of symptoms, and Recovery may be delayed in these cases.
- The patient should not return to play until they have achieved a full or pain-free range of motion.
FAQ
Treatment includes stretching exercises, physical therapy, pain relief medications, or corticosteroid injections. Surgery is only recommended for severe cases of psoas tendonitis that doesn’t respond to conservative measures.
Iliopsoas bursitis is easy to treat in many cases. It usually requires rest or some minimal care to improve symptoms and heal the damage. Stretches or exercises that target the hips are helpful in preventing iliopsoas bursitis.
Your doctor advises limited activity during your recovery period, which can range from six to eight weeks to give your iliopsoas muscles and the bursae time to fully heal. Your doctor or physical therapist will work with you to develop an exercise or stretching program to get you ready for a full return to play.
The symptom of Iliopsoas tendinopathy/bursitis is: A deep aching pain felt in the front of your hip (in the crease of your hip). A clicking and clunking sensation and sound when flexing your hip (lifting your knee up). Sharp pain with sitting or standing, especially after prolonged sitting.