Heel Bursitis
Table of Contents
What is a Heel Bursitis?
Heel bursitis is a condition characterized by inflammation and swelling of the bursa located at the back of the heel. The bursa is a small fluid-filled sac that acts as a cushion between the bone and the surrounding tissues, such as tendons and muscles. Bursitis can occur in various joints throughout the body, including the heel.
The bursa between the heel bone and Achilles tendon is afflicted by the painful ailment known as heel bursitis. The ability to move the ankle or foot may be impacted.
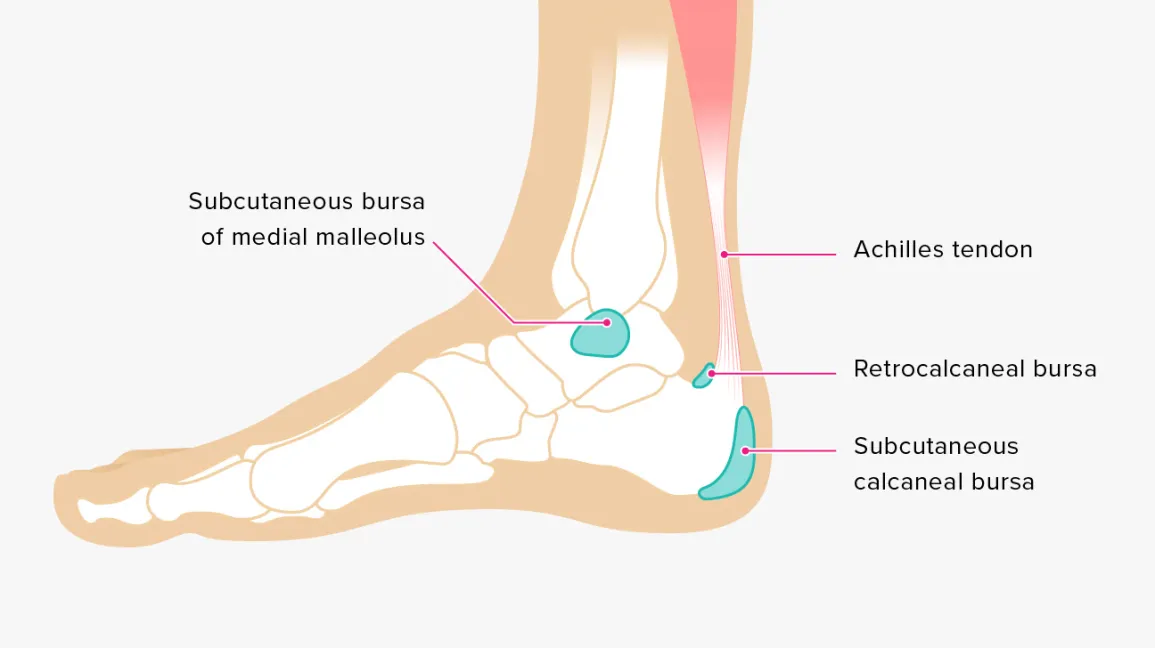
Heel anatomy:
The anatomy at the rear of the heel is not straightforward; in fact, it is somewhat complicated.
The calcaneus, a big heel bone, is the first. The thick Achilles tendon attaches to this bone from above. Two heel bursae—the larger retrocalcaneal bursa beneath the Achilles tendon and the smaller, more superficial retro-Achilles bursa above the tendon close to the skin—protect the tendon. Next to the deeper bursa is a sizable fat pad known as Kager’s fat pad. Last but not least, the fat pad and tendon are sandwiched by the rear of the ankle joint. Is it any wonder that we experience issues like Achilles bursitis, tendonitis, or heel bursitis given how complex our anatomy is?
What exactly is heel bursitis?
A body contains a bursa, which is a tiny, slick sac that contains fluid. Bursae, the plural version of bursa, serve as a lubricant and a cushion. They guard against the sliding or rubbing of bones against tendons, muscles, or skin. These sacs prevent the bones from rubbing against one another and cushion your joints. When a bursa becomes irritated, bursitis develops.
Behind each of the ankles, close to the calcaneus, is a bursa. It’s located where your Achilles tendon and heel bone meet. The bursa is commonly referred to as the retrocalcaneal (heel-back) bursa.
Bursitis develops when a bursa is inflamed and painful. The bursa in the heel is only affected by heel bursitis. It hurts the heels and feet.
In the heel area, close to the Achilles tendon, are bursae. The calf muscle is joined to the heel bone’s back via the Achilles tendon. Different types of heel bursitis can result from bursae irritation.
- Retrocalcaneum: The calcaneus is the name of the heel bone. Inflammation of the bursa located between your Achilles tendon and heel bone is known as retrocalcaneal bursitis. This kind is also known as Achilles tendon bursitis or ankle bursitis.
- Bursa subcutaneous to the calcaneus: Subcutaneous refers to beneath the skin, therefore this kind of bursitis affects the area between your heel’s skin and the Achilles tendon. A different name for it is posterior Achilles tendon bursitis.
What Are the Causes of Heel Bursitis?
A bursa serves as a lubricant and cushion for muscles or tendons moving across the bone. Around the majority of the body’s main joints, including the ankle, there are bursas.
By the heel, the retrocalcaneal bursa is situated at the back of the ankle. The area is located underneath the thick Achilles tendon that joins the calf muscles to the heel bone.
This bursa may irritate and inflame if the ankle is overused or used repeatedly. It could be brought on by excessive running, walking, or leaping.
Achilles tendinitis is frequently associated with this ailment. Achilles tendonitis and retrocalcaneal bursitis can occasionally be confused.
Injuries to the heel and repeated overuse are the usual causes of heel bursitis. It frequently occurs to runners or usually from donning the incorrect footwear. Running for extended periods of time in constrictive footwear or while sporting high heels put pressure on and restricts your heel bone, which may result in inflammation.
Other runners that may experience heel bursitis include:
- Overtrain
- Increase the distance of a run.
- Not warming up and stretching completely
- Run a lot of hills
- Starting a rigorous exercise regimen
- Without the proper training, abruptly increasing activity level
- Alterations in activity level history of inflammatory arthritis
Additionally, several inflammatory joint conditions might lead to heel bursitis. These consist of:
- Arthritis rheumatic: A form of arthritis in which your organs and joints are attacked by your immune system.
- Gout: It is a form of arthritis that develops when uric acid levels in the joints rise.
- Arthritic psoriasis: A form of arthritis that can strike some sufferers of the inflammatory disease psoriasis.
- Ankylosis Spondylitis: A chronic inflammatory condition where some bones gradually fuse together.
Sometimes infections or a disease known as Haglund deformity, which results in a bony lump on the back of your heel, can also cause heel bursitis. The bursa located between the Achilles tendon and heel may become compressed by the bump. However, activity, overtraining, and tight shoes are factors in the majority of cases.
Causes of heel (retrocalcaneal) bursitis:
- Tight calf muscles
- Arthritis
- Abnormality of the foot
- Activities such as running or walking
- Sports injuries
- Strenuous calf muscles
- Foot abnormality Arthritis
- Exercises like running or walking
- Athletic injuries
Why does heel bursitis occur?
There are numerous factors that might lead to heel bursitis:
- A lot of standing, moving, moving quickly, or jumping.
- Accelerating the pace of your workouts or hobbies.
- Not stretching enough.
- Shoes that fit tightly.
- Infection.
Who is affected by heel bursitis?
People who abuse their ankles without adequate training are most frequently affected. Heel bursitis can be brought on by a sudden increase in walking, jogging, or leaping.
It’s crucial to wear the right shoes, especially whether exercising or playing a sport. Shoes that are too tight can result in heel bursitis.
Bursitis of the heel can be painful. Some actions may be challenging if you have heel bursitis. Running, jumping, and walking could be unpleasant.
Additionally, individuals with additional conditions, such as:
- Haglund’s deformity
- Rheumatoid arthritis.
- Ankylosing spondylitis (AS).
- Psoriatic arthritis.
- Reactive arthritis (formerly known as Reiter’s syndrome).
- Pseudogout
- Gout.
- Infection.
How common is heel bursitis?
Bursitis of the heel is a common ailment. Athletes that run a lot are prone to it. Athletes who engage in repetitive foot-and-ankle motions, such as dancing, are also affected.
Symptoms:
Pain in the foot and heel is the predominant symptom. Pressure and movement pain when the sacs are irritated and inflamed.
Other signs of bursitis include:
- Swelling of the ankle or foot
- Discomfort behind or in the heel.
- Fever – If the patient develops a temperature, bursitis may have developed into septic bursitis. If this is the case, you should see a doctor every once.
- The foot or ankle may be painful or tender; commonly, heel bursitis causes pain that, if left untreated, becomes intolerable.
- Difficulty walking
- Discomfort when standing on your toes
- Tenderness
- Your heel’s warm and irritated skin
- Making a crackling sound with the foot flexed
- Difficulty wearing shoes
- Suffering when one stands
- The skin tone surrounding the heel changes.
- A lack of motion
- Calf muscle aches when running or walking
- Uncomfortable in shoes
Risk factors for heel (retrocalcaneal) bursitis:
Heel bursitis risk factors include:
- Age: the bursa’s shock absorption lessons as people age.
- Prior conditions: Gout, pseudogout, gout, osteoarthritis, and rheumatoid arthritis are all examples of prior disorders that can increase your risk of developing heel bursitis.
- Footwear: Donning shoes that are uncomfortable to wear and dig into the heel.
- Long-distance running: People who run or walk long distances are more likely to develop heel bursitis.
You may be more susceptible to getting retrocalcaneal bursitis if you:
- A person who is above 65
- Play sports with a high level of activity
- Improper stretching before to exercise
- Possess tense muscles
- Have a work that necessitates constant motion and puts strain on the joints
Diagnosis:
A doctor will do a physical examination and ask about the medical history. A foot and ankle will be palpated or squeezed, and look for any signs of swelling and gauge how well a person can move the foot.
They might inquire about your level of exercise, the type of shoes a person wears, and whether or not a person spends a lot of time standing at your job.
The foot and heel will be examined by a doctor to look for any indications of discomfort, redness, or heat. To rule out a fracture or a more serious injury, they might utilize an X-ray or an MRI. Your doctor may occasionally sample fluid from the swollen spot to check for an infection.
In some circumstances, your doctor may prescribe imaging tests like an X-ray to search for bone fractures or an MRI to check for bursa inflammation. These tests aren’t typically required, though. Bursitis is frequently easy to identify by your doctor just by feeling your foot and asking you about your symptoms.
How is heel bursitis determined to exist?
Before performing a foot examination, a medical professional could inquire about various things, such as:
- Do you frequently stand?
- What kind of workout do you undertake?
- What kinds of shoes wear you?
- Have you ever experienced heel bursitis?
Your foot will be examined by a medical professional. When they:
- Look for any swelling.
- Make a note of any sore or painful spots.
- Verify the range of motion of your foot.
- Ask you to flex your feet or stand on your tiptoes.
If your doctor believes you have a bacterial infection, they might:
- Inquire about your chills.
- Take a temperature.
- With a syringe, aspirate some liquid from the heel bursa (bursal aspiration). They will check the fluid for bacteria before using it.
If an orthopaedic specialist or primary care physician suspects the patient has heel bursitis, they will conduct a thorough physical examination and may request an x-ray, MRI, or ultrasound. The patient’s heel bone abnormalities or bone spurs where the Achilles attaches will be identified based on images from these modalities.
Tests for diagnosis:
Your healthcare professional can confirm heel bursitis using imaging studies. They may consist of:
- X-rays: A detailed image of your heel bone can be seen on an X-ray. Your doctor will look through the x-ray to look for any abnormalities in your heel bone. Your foot’s motion may be affected by anomalies. Your risk of getting heel bursitis can go up if you have an anomaly or another illness.
- Magnetic resonance imaging (MRI): An MRI can reveal whether another condition, such as Achilles tendinitis, is to blame for your heel pain in addition to heel bursitis.
Contact an orthopaedic doctor if the pain does not go away within a week or gets worse.
Treatment of Heel Bursitis
Home Treatment:
Home care aimed at lowering inflammation can successfully treat many cases of retrocalcaneal bursitis. Medical measures are necessary in more severe or persistent situations. Surgery is a rare necessity.
Heel bursitis is typically treatable at home. A few simple habits can be altered to reduce inflammation and promote bursa healing. Among the at-home remedies for heel bursitis are:
- Rest: Taking a break from regular walks or workouts may give the bursa time to recover and reduce inflammation.
- Ice compress: Two or three times a day, applying ice to the back of the ankle for about 20 minutes each time may help reduce swelling, discomfort, and inflammation. To protect the skin, wrap the ice in a towel.
- Supportive shoes: Wear more supportive, comfy footwear instead of heels and ankles with a hard structure.
- Retrocalcaneal bursitis sufferers may find relief from their symptoms by wearing shoes with an Achilles notch, a groove in the collar at the back of the shoe to protect the Achilles tendon. (Achilles notches are incorporated into the majority of running shoes.) Additionally, the Achilles tendon can be relieved of tension by wearing shoes with arch support, which reduces the likelihood that the tendon will uncomfortable rub against the retrocalcaneal bursa.
- Try wearing open-heeled shoes if you have calcaneal bursitis, which is frequently brought on by uncomfortably fitting shoes.
- Heel bursitis shoe inserts: The retrocalcaneal bursa’s discomfort can be decreased by using shoe additions such as heel wedges, which can promote improved foot mechanics. 1 Shoe inserts can be purchased from a store or created to order after a doctor’s prescription.
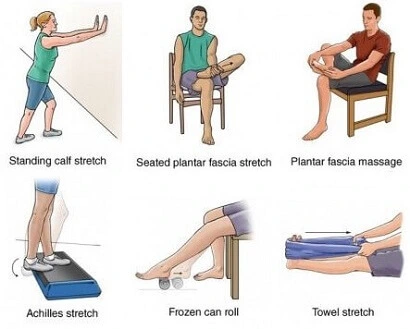
- Stretching causes heel bursitis:
The retrocalcaneal bursa will no longer feel pressure if a tight Achilles tendon is stretched. Gentle stretches without bouncing are best.- For calcaneal bursitis, which is less likely to be brought on by a tight Achilles tendon, stretching is not a typical treatment.
- Treatment for heel bursitis depends on the underlying cause but typically entails resting your foot to give it time to recover. You can stretch your Achilles tendon and get pain relief from other treatments.
- If shoe inserts and at-home remedies are ineffective, your doctor can suggest a steroid injection if it’s safe to do so. They’ll think about the dangers of injecting steroids here, such as Achilles tendon rupture.
- If you have Achilles tendonitis as well, your doctor may additionally advise you to wear a brace or cast. Strengthening the region around your heel and ankle can also be achieved with physical therapy. If other therapies don’t work, you might in very rare circumstances need surgery to remove the bursa.
Be careful to see a doctor if you have any of the following symptoms. These could be signs of a heel infection:
- Severe oedema or rash close to the heel
- Strong or shooting heel pain and a fever of more than 100.4°F (38°C)
Non-Surgical Treatment:
Pain and inflammation can be treated with:
- Rest: Avoid any activities, such as running or leaping, that aggravate or exacerbate discomfort. The bursa will have time to heal as a result.
- Ice: For up to 20 minutes, three to four times a day, apply an ice pack wrapped in a thin towel to your heel and ankle. Ice is recommended. If at all possible, take a rest, elevate your foot, and apply ice to it to assist reduce discomfort, swelling, and inflammation.
- Proper footwear: Avoid wearing heels with a tight grip or shoes that are excessively tight. To protect your Achilles tendon, put on footwear with an Achilles notch in the back collar. Your Achilles tendon will also be less stressed if your shoes have enough arch support.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs), like aspirin, ibuprofen, and naproxen, are available over the counter and can help with your heel bursitis’s discomfort and inflammation. It’s a good idea to speak with your healthcare professional before using an NSAID because not everyone can take them.
- Injections of steroids: If the inflammation in your heel bursitis doesn’t go down, your doctor may advise getting steroid injections.
- Replace your shoes: You might need to temporarily switch to a medium-height shoe if you wear high heels. Sometimes switching right away to flat shoes can exacerbate problems.
- A lower ankle profile or buying new shoes will assist if your running shoes are too tight around your ankle. For everyday wear, an open-back shoe can also relieve strain from your heel.
Treatment for heel bursitis is based on the source of your pain. A doctor might advise attempting further treatment options if symptoms continue after two or three weeks of home treatment. Treatment options include:
- Orthotics: Heel wedges promote appropriate walking form and lessen heel abrasion. Heel wedges are available to buy at stores. Additionally, your doctor can have heel wedges made specifically for your foot. With appropriate walking form, you can lessen the pain in your heel with the use of shoe inserts or insoles.
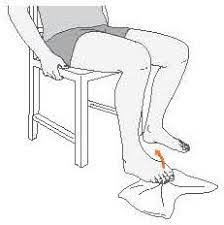
- Physical treatment: You can relieve pressure on your heel bursa by stretching your Achilles tendon. Stretches for the calves, toes on a wall, and heel drops might all be helpful. Stretching exercises for the calf muscle and Achilles tendon may relieve pressure on the bursae and reduce pain. Exercises for the ankle, foot, and calf strengthen the Achilles tendon and the surrounding muscles. Additionally, your bursa is relieved of pressure.
- Exercises and stretches can help the Achilles tendon stay healthy and relieve pressure on the bursa. Patients are advised to carry out these stretches and exercises at home even after their heel pain subsides in order to prevent further bursa flare-ups.
- Ultrasound therapy: Therapeutic ultrasound uses sound waves to vibrate the skin, which could promote healing and blood flow. The majority of individuals do not experience any pain during this heel bursitis treatment. A medical professional, podiatrist, or physical therapist could administer ultrasound therapy.
- Aspiration: Pressure at the back of the heel can be relieved and pain reduced by draining bursal fluid. The enlarged bursa is drained of fluid using a needle and syringe. For this procedure, the term “bursal aspiration” is used.
- A local anaesthetic can be used to do bursal aspiration in a hospital or doctor’s office. The needle may be precisely guided into the enlarged bursa of the heel using ultrasound imaging (different from therapeutic ultrasound).
- Cortisone injection: Cortisone, a hormone produced by humans, can reduce inflammation in the body. The irritation brought on by retrocalcaneal bursitis may be swiftly reduced by a cortisone injection in the heel.
- While cortisone injections may successfully relieve uncomfortable symptoms, other research contends that they are linked to Achilles tendon damage. Patients are recommended to temporarily refrain from stretching, squatting, and jogging to reduce the chance of a tendon injury. A cast may be suggested by some medical practitioners to temporarily immobilize the heel and safeguard the Achilles tendon and associated enthesis.
- Newer treatments, such as platelet-rich plasma and other methods of regenerative medicine, are occasionally advised instead of cortisone because it may cause tissue damage. Ongoing research is being done to determine how well these treatments work.
- Additionally, due to the tiny danger of introducing germs, which can result in septic bursitis, many specialists urge caution when thinking about corticosteroid injections.
- In extremely rare circumstances, your doctor might administer a corticosteroid injection to your heel. Inflammation will be lessened by this.
- Oral antibiotics: will be recommended by your doctor if an infection caused your bursitis. Antibiotics for infected heel bursitis. Antibiotics are necessary for the treatment of septic bursitis. Antibiotics taken by mouth are usually effective. Hospitalization and intravenous antibiotics may be required for more complicated cases.
- Surgery: Rarely is surgery necessary. However, you might need to consult a foot and ankle surgeon if your discomfort hasn’t subsided in six to 12 months. The damaged bursa may be surgically removed (bursectomy).
Physical Therapy:
Ice can be administered to the rear heel and ankle numerous times each day when the condition is acute.
In the acute stage of retrocalcaneal bursitis, the patient should be advised to apply ice to the posterior heel and ankle. A few times a day, for 15-20 minutes each, icing can be done. Additionally, some clinicians support the use of contrast baths.
The Achilles tendon can be gradually stretched out in the following ways to reduce impingement on the subtendinous bursa:
- Place the foot that is injured flat on the ground and stand in front of a wall. As soon as you feel a slight stretching in the ipsilateral Achilles tendon, lean forward and toward the wall.
- After holding the stretch for 20 to 60 seconds, release it.
- Both with the knee extended and then again with the knee flexed, perform the stretches.
- Repeat the techniques above for numerous stretches every set, several times a day, to get the most out of the stretching routine. Steer clear of ballistic (i.e., sudden, jerky) stretches.
- Microcurrent therapy and injections of corticosteroids into the retrocalcaneal bursa are further treatment possibilities.
Exercises Such as:
- Toe raise
- Toe curl
- Toe extension
- Marble pick up
- Tennis ball roll
- Sand walk
- Achilles stretch
Heel (Retrocalcaneal) Bursitis Surgery:
A surgical procedure to remove the problematic bursa may be used to treat very difficult cases of retrocalcaneal bursitis. Bursectomy surgery is not frequently required.
A new retrocalcaneal bursa may form following surgery. The new bursa should be less prone to inflammation, one hopes.
Surgery can be beneficial, although it can be difficult to operate on this bony area. Potential dangers include infection, Achilles tendon injury, poor recovery, and persistent heel pain.
Additional surgical techniques:
It is possible to combine a bursectomy with additional surgical procedures. For instance, a surgeon may correct a Haglund deformity by removing a small piece of bone from the rear of the heel to change the way the foot moves and lessen future friction. You could also get rid of bone spurs.
Regardless of the method of therapy, it’s crucial to wait until all discomfort and swelling at the heel’s back have subsided before starting new activities. It can take a few weeks.
It is advised to resume regular activities gradually and cautiously. Too soon after stopping an activity, heel bursitis symptoms may return.
Prevention:
The following actions can be taken to avoid the issue:
- To help prevent this issue, maintain appropriate flexibility and strength around the ankle.
- To reduce the risk of damage, stretch the Achilles tendon.
- Wear shoes with adequate arch support to reduce stress on the tendon and bursa irritation.
- Use good form when working out.
Summary:
Depending on the severity of the ailment, recovery time for patients with heel bursitis can range from a few days to many months.
Patients who are healing from heel bursitis should be especially aware of the shoes they are wearing to make sure they are comfortable and aren’t adding to the heel’s pressure.
To determine when they can resume their regular activities, patients should consult carefully with their orthopaedic doctor.
FAQs:
Will a heel bursa go away?
Home care aimed at lowering inflammation can successfully treat many cases of retrocalcaneal bursitis. Medical measures are necessary for more severe or persistent situations. Surgery is a rare necessity.
How serious is heel bursitis?
Septic bursitis may be present if the skin on the back of the heel feels unusually heated to the touch. An infection is the root of this illness. Despite its rarity, septic heel bursitis is a serious illness, and patients should get treatment to prevent the infection from spreading or worsening.
What triggers bursitis?
Bursitis is typically brought on by an accident or excessive use. It may also result from an infection. Other issues are connected to bursitis. These conditions include thyroid dysfunction, gout, tendonitis, diabetes, and arthritis.
What is a good home remedy for bursitis?
Use heat that is dry or wet, like a heating pad or a warm bath. Take an over-the-counter pain reliever such as ibuprofen (Advil, Motrin IB, etc.) or naproxen sodium (Aleve, etc.) to reduce inflammation and relieve discomfort. Some can be applied directly to the skin.
How long does heel bursitis last?
Depending on the severity of the ailment, recovery time for patients with heel bursitis can range from a few days to many months. Patients who are healing from heel bursitis should be especially aware of the shoes they are wearing to make sure they are comfortable and aren’t adding to the heel’s pressure.



One Comment