Foot Strain
Foot Strain occurs when the muscles, tendons, or ligaments in the foot are overstretched or overused, leading to pain, swelling, and difficulty walking. It’s commonly caused by excessive activity, poor footwear, or sudden increases in physical stress on the feet.
Table of Contents
What is the Foot Strain
An injury to the foot’s muscles or tendons is referred to as a foot strain.
It happens when excessive force, incorrect use, or sudden movement causes these soft tissues to become overstretched, ripped, or strained.
- Muscles provide you with stability and mobility.
- Bones and muscles are joined by a tendon.
Pain and restricted function may result from tiny rips or inflammation that form when these tissues are overextended.
Anatomy of the Foot
A highly specialized structure, the foot allows for balance, support, and movement. It serves as a flexible adaptor for uneven terrain as well as a hard lever for propulsion.
It is made up of blood vessels, nerves, muscles, tendons, ligaments, joints, and bones that all operate together.

The foot’s bones (26 bones)
Three zones are used to organize the bones:
Two bones in the hindfoot
The Talus
- articulates with the ankle joint (talocrural joint) via the tibia and fibula.
- transfers weight from the torso to the foot.
- Trochlea—upper surface.
- No attachments to muscles.
Calcaneus (bone of the heel)
- The largest foot bone.
- aids in supporting the talus.
- The Achilles tendon attachment point is on the posterior surface.
- forms the talus and subtalar joint.
Five bones at the midfoot
Navicular: Part of the medial arch; articulates with the talus and cuneiforms; medial side of the foot.
Cuboid: Lateral side; stabilizes lateral arch; articulates with calcaneus and fourth to fifth metatarsals.
Three cuneiforms—medial, intermediate, and lateral—form the transverse arch and articulate with the navicular and first three metatarsals.
Forefoot (bone number 19)
- The foot’s long bones, known as metatarsals, are numbered I through V (medial to lateral). Base → uses tarsals to articulate. Phalanges are used to articulate the head.
- Phalanges (14): Hallux (great toe): 2 (proximal & distal). Three of each of the other toes (proximal, middle, and distal). Permit toe extension and flexion.
Joints Of The Foot
Foot and Ankle Mobile Joints (Essential Joints):
- Tibiotalar joint, or ankle joint
- The subtalar joint
- TN joint, or talonavicular joint
- MTP joints, or metatarsophalangeal joints
Joints with Moderate Movement:
- Cuboid-calcaneal junction
- The fourth and fifth metatarsals’ cuboid-metatarsal joints.
- PIP, or proximal interphalangeal joint
- DIP, or distal interphalangeal joint
Non-essential joints (joints with little movement):
- Cuneiform-navigular joints
- Joints that are intercuneiform
- The “Lisfranc” joint (midfoot joint) is the tarsometatarsal (TMT) joint.
Ligament of the foot
Anterior TaloFibular Ligament (ATFL)
When an ankle is sprained, the most often damaged ligament is the anterior talofibular ligament. To link to the talus’ neck, the ATFL extends from the front side of the distal fibula (lateral malleolus) down to the outer front part of the ankle. Particularly when the ankle is plantar-flexed, it stabilizes it against inversion.
Calcaneo-Fibular Ligament( CFL)
The lateral side of the ankle also has the calcaneofibular ligament. It begins at the fibula’s tip and extends into the calcaneus and along the ankle’s lateral side. Inversion resistance is also present, although it is greater when the ankle is dorsiflexed.
Posterior Talo-Fibular Ligament
The posterior talofibular ligament extends into the outside back region of the calcaneus from the rear lower section of the fibula. The ankle and subtalar joints are stabilized by this ligament.
The Deltoid Ligament
On the medial side of the ankle lies a fan-shaped band of connective tissue called the deltoid ligament. It descends into the talus and calcaneus from the medial malleolus. The more superficial, larger portion of the ligament extends into the calcaneus, whereas the deeper branch is firmly attached to the talus. The purpose of this ligament is to prevent eversion.
Spring Ligament
The sustentaculum tali, a bony protrusion of the calcaneus on the medial part of the hindfoot, is where the spring ligament, a powerful ligament, begins. The talar head is supported and cradled by the spring ligament, which inserts into the plantar-medial portion of the navicular.
The Lisfranc Ligament
The tarsometatarsal joints are stabilized by a group of ligaments called the Lisfranc joint complex. These ligaments provide the arch of the foot a great deal of stability by limiting the amount of movement in the midfoot joints. The dorsal side ligaments are weaker than the plantar ligaments. A robust band of tissue called the Lisfranc ligament joins the base of the second metatarsal to the medial cuneiform.
The Ligaments Between the Metatarsals
At the base of the toes, these ligaments connect the metatarsal bones. They link the neck area of each metatarsal to the one next to it, and bind them together. The metatarsals remain in rhythm as a result. These ligaments can be torn, but they can also irritate the digital nerve as it passes through them, resulting in a Morton’s neuroma.
The Great Toe’s first MTP joint capsule
This ligament’s connective tissue is shaped like a capsule. It extends to the distal phalanx on the same side as the medial part of the first metatarsal head. This enables the medial side of the great toe to be stabilized by this ligament. The great toe shifts position and becomes angulated outward when a person develops a bunion, causing this band to extend out.
The Anterior Inferior TibioFibular (AITFL) Ligament
The tibia and fibula are held together by the anterior inferior tibiofibular ligament (Figure 4), which is located on the anterolateral part of the ankle joint. When the foot remains on the ground while the leg turns inward, it can cause high ankle sprains, which are injuries to this ligament.
Interosseous Membrane
Strong fibrous tissue makes up the interosseous membrane, which runs down the tibia and fibula and maintains the two bones’ joint motion.
Muscles of the Foot
Several smaller muscles are located deep within the foot. They improve in foot stability and toe movement. Since they are completely confined within the foot, they are collectively referred to as the intrinsic muscles of the foot. The extensor hallucis brevis and the extensor digitorum brevis are the only two of these muscles found on the dorsal portion of the foot.
The deep peroneal nerve innervates both of them. Their main function is to help in toe extension. This contrasts with the flexor digitorum brevis and flexor hallucis brevis. The great toe and the four lesser toes may be flexed with the help of these muscular tendon units, which are situated deep inside the plantar arch. The medial plantar nerve innervates them.
Nerves
Deep Peroneal Nerve
One of the peroneal nerve’s two components is the deep peroneal nerve. Directly behind the fibula’s head is the deep peroneal nerve. It runs from the front of the ankle to the dorsal surface of the foot and is in charge of regulating the muscles in the leg’s anterior compartment. It is in charge of providing sensation in the first web space, which is the little space between the first and second toes. This location won’t have any feeling if this nerve isn’t working. A condition called “drop foot” occurs when motor function is compromised, making it unable to raise the foot upward.
Superficial Peroneal Nerve
The deep peroneal nerve is partnered with the superficial peroneal nerve. It innervates the muscles of the lateral compartment and runs down the side of the leg behind the knee, beneath the fibula’s head. It divides into many branches on the dorsal portion of the foot after running down across the anterolateral aspect of the ankle. For the majority of its length, the superficial peroneal nerve contains both motor and sensory neurons; however, below the ankle, only sensory nerves are present. It is impossible to evert the foot if this nerve’s motor function is compromised, yet distal to the ankle, no motor function is lost.
Tibial Nerve
All of the deep and superficial posterior compartment muscles in the back of the calf, which are located behind the tibia and fibula, are controlled by the tibial nerve. The medial and lateral plantar nerves are the two branches of the tibial nerve, which extends into the deep inner region of the ankle. These two branches innervate all of the little muscles in the sole and give feeling to the whole sole.
The Sural Nerve
The sural nerve, another branch of the tibial nerve, is the fourth nerve of the foot. This nerve connects the lateral portion of the foot to just below the knee. At the level of the posterolateral ankle, it becomes a very superficial nerve that extends distally to provide feeling to the outside of the foot. Its motor function is nonexistent.
The Saphenous Nerve
The femoral nerve only gives rise to the fifth and final nerve. To give feeling to the inside of the foot, it extends from the medial aspect of the knee and crosses the anteromedial portion of the ankle joint.
Plantar Fascia
The plantar fascia is a robust fibrous tissue rather than a nerve, tendon, or muscle. This tissue extends to the base of each of the five toes and begins deep beneath the calcaneus’ (heel bone) plantar surface. The toes dorsiflex and pull on the plantar fascia as the foot glides off the ground when walking. By keeping the calcaneus and metatarsal heads apart, this action tends to tighten the plantar fascia, supporting the foot’s arch. This process is called the windlass mechanism. This tough, comparatively impermeable layer aids in protecting the foot’s sole muscles.
Causes of Foot Strain
- Excessive usage of repeated motions (dancing, running, and leaping)
- Poor arch support or worn-out shoes are examples of inappropriate footwear.
- Unexpected increase in activity (new workout regimen, for example)
- Standing for extended periods of time
- Running or walking over uneven terrain
- Unusual foot mechanics include high arches or flat feet.
- Trauma: abrupt foot twisting, tripping, or overextension
Symptoms of Foot Strain
- localized discomfort, usually on the top of the foot, heel, or arch.
- Tenderness or swelling
- Tightness or spasms in the muscles
- Bruising (in situations that are mild to severe)
- Pain with movement or when carrying weight
- Foot weakness
- Inability to stand or walk for extended periods of time
Diagnosis of Foot Strain
A physical examination of the patient and an assessment of the injury’s circumstances and symptoms are standard procedures for diagnosing foot strains. In order to confirm the diagnosis and rule out other issues, such as bone fractures, X-rays may also be required. Upon diagnosis, sprains and strains are categorized as I, II, or III based on the degree of function loss, discomfort, and injury severity.
Exercises For Foot Strain
Protocol for R.I.C.E.
- Rest: Keep away from painful activities.
- Ice: three to four times a day for 15 to 20 minutes.
- Compression: Support with an elastic bandage.
- Elevation: Maintain your foot elevated over your heart.
Toe raise
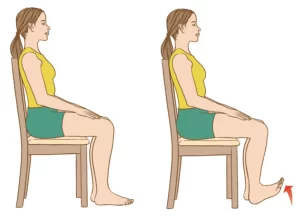
- Place your feet flat on the floor and sit up straight on a chair.
- Lift the heels while maintaining the toes on the ground. When just the balls of your feet are left on the ground, stop.
- Before lowering the heels, hold this stance for five seconds.
- Only the tips of the big and second toes should contact the ground during the second stage, so lift the heels and point the toes.
- Before descending, hold for five seconds.
- To ensure that just the tips of the toes touch the floor in the third step, lift the heels and curl the toes inward. For five seconds, maintain this posture.
- Ten repetitions of each step will increase your mobility and flexibility.
Towel Stretch

- Sit with your legs outstretched.
- Wrap a belt or cloth around your foot.
- Pull the cloth gently in your direction until your leg and arch feel stretched.
- Repeat three to five times every session, holding for 20 to 30 seconds.
- The Achilles tendon, plantar fascia, and calf are the targets.
Marble Pickups
- Put ten to fifteen marbles on the ground.
- Using your toes, pick up each marble and place it in a basin.
- Sets: two to three per day.
- Improves toe strength and fine motor control.
Toe curls
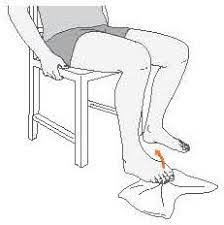
- Place your feet flat on the floor and sit up straight on a chair.
- With the short side toward the feet, place a small towel on the floor in front of the torso.
- On the short side of the towel, place one foot’s toes. Try to draw the towel toward you by holding it between your toes. Before moving on to the other foot, perform this exercise five times.
- Try using an object to weigh down the towel’s other end to make this workout more difficult.
Achilles stretch
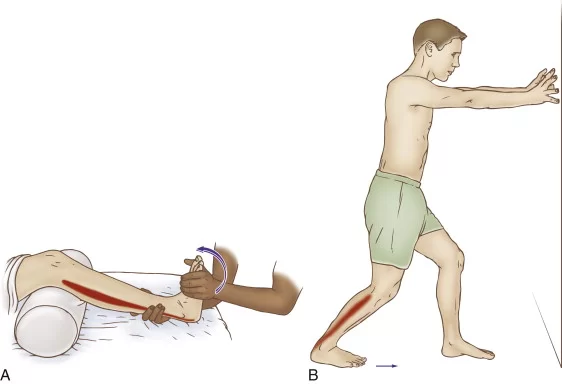
- Lift the arms till the palms of the hands are flat against the wall while facing the wall.
- Reposition one foot while maintaining a straight knee. Next, bend the opposing leg’s knee.
- Both heels should remain level on the ground.
- The calf muscles and Achilles tendon should feel stretched after pushing the hips forward.
- After 30 seconds of holding, switch sides. On each side, repeat three times.
- Push the hips forward and bend the back knee for a somewhat different stretch.
Ball Roll

- Place your feet flat on the floor and sit up straight on a chair.
- On the floor close to the feet, place a golf ball or a similar tiny, firm object.
- Press down as firmly as it feels comfortable while moving the ball with one foot on it.
- If there are no appropriate balls accessible, a frozen bottle of water might be a calming substitute.
Summary
- It’s a good idea to keep the ankles and feet healthy. The previously mentioned activities can help avoid discomfort, lessen the chance of damage, and soothe current pain.
- Exercises may be helpful for people with a diagnosed foot condition, such as plantar fasciitis or Achilles tendon strain.
- If at all possible, consult a healthcare provider before beginning a new stretching and exercise regimen.
FAQ
How do you treat a strained foot?
The R.I.C.E. technique is used to treat a foot strain: Rest the injured foot, elevate it above your heart, apply ice for 15 to 20 minutes several times a day, and use compression with an elastic bandage to reduce swelling (but not too tight). Acetaminophen or ibuprofen are examples of over-the-counter pain medicines that can be helpful, but if symptoms develop, you are unable to bear weight on the foot, or you see a noticeable deformity, you should visit a doctor.
How long does it take for foot strains to go away?
Minor foot strains can heal in a few days to weeks, but more serious instances may take six to twelve weeks or more. The healing period for foot strains varies greatly depending on the degree of the injury. A doctor may suggest crutches, a boot, or physical therapy for more serious injuries, while RICE (rest, ice, compression, and elevation) is the general protocol for moderate injuries. If the pain doesn’t go away, you can’t walk properly, or you have symptoms of a more serious injury,
How is a foot strain diagnosed?
We will evaluate the ankle or foot and obtain a history of the injury in order to determine the severity of the condition. To ascertain the severity of the damage, the physician may prescribe further examinations. These consist of: MRI stands for magnetic resonance imaging.
How to cure muscle strain in the feet?
Take frequent pauses to give your feet a moment. To reduce discomfort and swelling, apply cold packs. Spend twenty minutes each day soaking your feet in Epsom salts. To enhance circulation and lessen inflammation, put on compression socks.
What are three symptoms of a muscle strain?
Tenderness or pain.
bruises or redness.
restricted movement.
cramping in the muscles.
swelling.
Weakening of the muscles.
Refrences
- Anatomy Of The Foot Ankle – OrthoPaedia. (n.d.). OrthoPaedia. https://www.orthopaedia.com/anatomy-of-the-foot-ankle/
- Foot Sprains and Strains | Orthopedic Medical Center. (n.d.). https://www.orthomedctr.com/foot-sprains-and-strains.php
- Cadman, B. (2025, May 6). Best stretches and exercises for healthy feet. https://www.medicalnewstoday.com/articles/320964#flexibility-exercises