Cervical Vertebrae
Table of Contents
What is a Cervical Vertebrae?
The cervical spine, made of 7 cervical vertebrae also called to as C1 to C7 is divided into two major parts: the craniocervical junction (CCJ) and the subaxial spine.
The function of the cervical vertebrae is to protect your spinal cord and creates a neck movement that helps to do day-to-day activity and also takes the weight off your Head. The seven bones joined together to form a bony tunnel for your spinal cord to travel through. The articulation of 2 vertebrae creates a small hole, called a foramen, through which your peripheral spinal nerves passed.
Introduction
The spine, or vertebral column, is a segmental pair of thirty-three bones and connected soft tissues that comprise the subcranial portion of the axial skeleton.
There are 7, 12, and 5 articulating vertebrae in the cervical, thoracic, and lumbar spine. While somewhat equal in terms of bone morphology, these 3 regions variably balance spinal rigidity with flexibility and motion and articulate in a particular fashion that contributes to the overall S-shaped curvature of the spine. In spite, the sacrum and the coccyx are 2 sets of fused vertebrae at the caudal aspect of the spine that convey no movement. 5 fused vertebrae typically create the sacrum, with 4 creating the coccyx.
The entire cervical spine, constructed of seven cervical vertebrae directed as C1 to C7, is split up into two major segments: the craniocervical junction (CCJ) and the subaxial spine. The CCJ involves the occiput and the 2 most cephalad cervical vertebrae, identify as the atlas (C1) and the axis (C2). The subaxial spine involves the 5 most caudal cervical vertebrae (C3-C5). As a whole, the cervical spine is accountable for supporting the weight of the cranium and allowing movement of the head and neck.
Structure and Function
- The typical vertebrae have hallmark anatomic structures that are preserved across the cervical, thoracic, and lumbar regions.
- All vertebra is mainly developed through a ventral vertebral body containing mostly trabecular cancellous, and a denser, usually cortical dorsal vertebral arch.
- The vertebral body is the main form of intervertebral articulation and load-bearing.
- Every vertebral body is connected to its cranial and caudal counterparts by an intervertebral disk.
- The 2 laminae join at the midline and generate a dorsal projection known as the spinous process.
- The pedicles, laminae, and dorsum of the vertebral body form the vertebral foramen, an entire osseous ring that closes the spinal cord.
- Its important role is to protect the spinal cord and its connected vascular structures.
- In addition, the transverse processes and the superior and inferior articular processes are available around the junction of the pedicles and the laminae.
- In the cervical spine, the costal process compliments the anterior part of the transverse process that encompasses the vertebral artery foramen.
Unique Features of the Cervical Spine
- Despite displaying the most typical vertebral hallmarks, a particular amount of anatomical variation is present within the cervical spine.
- The main function of the cervical spine is to support and give the motion of the head and neck.
- Large vertebral bodies are not important, considering the relatively tiny weight-bearing load at this level.
- Thus, an improved range of movement takes priority over vertebral size and rigidity.
- However, the extra movement and flexibility can carry an increased risk for injury to the spinal cord and its connected neurovascular structures.
- All 7 cervical vertebrae have transverse foramen within their transverse processes, where a set of vertebral arteries goes through cranially through the vertebrae starting at C6 before coursing medially over the arch of C1 on the way to the foramen magnum.
- The spinous processes of the C2 to C6 vertebrae are bifurcated, C1 has a posterior tubercle in reverse a spinous process, and C7 has a much bigger and singular spinous process, identified as the vertebra prominence, which is equal to those in the thoracic vertebrae.
Upper Cervical Spine (Atlas (C1) – Axis (C2))
- The upper cervical part of the cervical spine includes C1 and C2, which are more usually referred to as the atlas and the axis, respectively.
- The main function of the atlas is to assist and cradle the base of the occiput at the atlantooccipital articulation.
- As such, there are too many features, especially in the atlas not shared with the rest of the spine.
- Most crucial, the atlas lacks a vertebral body and instead forms a big ring-shaped fusion of anterior and posterior arches that allows C1 to assist the spinal cord as it exits the foramen magnum.
- The atlas has pronounced concave and medially facing articular facets which assist the convex occipital condyles.
- This morphology helps the joint contribute an estimated fifty percent of flexion-extension of the neck but limits lateral displacement of the occiput.
- These joints gain more stabilization from strong soft-tissue ligaments that give tight adherence to the occiput.
- The hallmark part is its odontoid process, or dens, a bony projection enlarging cranially from the vertebral body.
- It develops from the body of the atlas and serves as the main attachment point for the soft tissues that stabilize the atlantoaxial junction.
- In contrast to the atlantooccipital joint, the atlantoaxial junction is in charge of about 50 percent of the rotational movement of the cervical spine.
- The junction has 3 articulations: a midline Atlanta-odontoid (or Atlanta-dental) joint and a form of the atlantoaxial facet joint.
- The Atlanta-odontoid joint allows the anterior arch of the atlas to rotate on the odontoid process.
- The lateral facet joints concern the articulation of the atlas’ inferior facets and the superior facets of the axis; these joints are dispassionately shallow to authorize significant movement.
- The 2nd cervical vertebra, the axis, has a more significant bony protrusion that points up from its vertebral body and fits into the ring-shaped atlas above it.
- The atlas can rotate near the axis, forming the atlantoaxial joint.
- More rotational range of movement happens at this joint compared to any other, with some estimates being that nearly half of the head’s rotation happens at this joint.
The Subaxial Cervical Spine – C3 to C7
- All 5 vertebrae in this region share around identical morphological and functional features and, as compared to the upper cervical spine, share most elements with the typical vertebral anatomy.
- All these upper vertebrae possess uncinate processes, which are bony prominences on the lateral edges of the vertebral body that are eloquent at Luschka joints to confer extra stability and prevent vertebral listhesis.
- There also live some tiny features of C7 that distinguish it from the rest of the subaxial region.
- The transverse foramen of C7 is slightly smaller than the leftovers of the region and typically does not house the vertebral arteries.
- The vertebra also has a somewhat bigger vertebral body.
Typical Vertebrae: C3, C4, C5, and C6
Vertebrae from C3 to C6 are known as typical vertebrae however they share equal basic elements with most of the vertebrae throughout the rest of the spine. Typical vertebrae have:
Vertebral body
- This thick bone is cylindrical-shaped and situated at the front of the vertebra.
- The vertebral body takes most of the load for a vertebra.
- At most levels of the spine, an intervertebral disc sits between two vertebral bodies to give cushioning and help absorb the shock of daily motions.
Vertebral arch
- This bony arch muffles around the spinal cord toward the back of the spine and consists of two pedicles and two laminae.
- The pedicles are connected with the vertebral body in the front, and the laminae transition into the spinous process (a bony hump) in the back side of the vertebra.
Facet joints
- Every vertebra has a pair of facet joints, also identify as zygapophysial joints.
- These joints, situated in the middle of the pedicle and lamina on each side of the vertebral arch, are lined with smooth cartilage to enable fixed movement in the middle of 2 vertebrae.
- Spinal degeneration or injury to the facet joints is among the most usual causes of chronic neck pain.
Unique Vertebra: C7
- The 7th cervical vertebra also identifies as the vertebra prominences, is generally considered a unique vertebra, and has the most prominent spinous process.
- When feeling the back of the neck, the C7 vertebra’s spinous process (bony hump) attaches more than the other cervical vertebrae.
Embryology
- The cervical vertebrae are the seven vertebrae that make up the neck region of the spinal column.
- They play a crucial role in supporting the head and providing mobility to the neck.
- During embryonic development, the cervical vertebrae form from the mesoderm, which is the middle layer of the developing embryo.
- The mesoderm gives rise to the somites, which are the segmented structures that eventually form the vertebrae.
- In the developing embryo, the cervical vertebrae begin to form around the fourth week of gestation.
- They initially develop as a set of somites in the head region of the embryo, which eventually migrate to the neck region.
- The somites then divide into two parts, the sclerotome, and the dermomyotome.
- The sclerotome gives rise to the vertebral bodies and the intervertebral discs, while the dermomyotome gives rise to the muscles and skin of the neck.
- The vertebral arches and processes, which are the bony structures that surround and protect the spinal cord, also develop from the sclerotome.
- As the cervical vertebrae continue to develop, they undergo various morphological changes to accommodate the unique functional demands of the neck.
- For example, the first cervical vertebra, or atlas, has no vertebral body and is designed to support the weight of the head.
- The second cervical vertebra, or axis, has a specialized process called the odontoid process, which allows for the rotation of the head.
Overall, the embryology of the cervical vertebrae is a complex process that involves the coordinated development of multiple tissues and structures. This process ultimately gives rise to the fully formed cervical vertebrae that are essential for proper neck function.
Blood Supply and Lymphatics
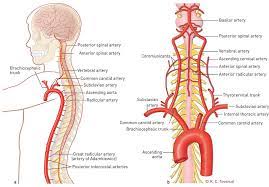
- The cervical vertebrae, like all other bones, require a blood supply and have lymphatic vessels to maintain their function and health.
- The blood supply to the cervical vertebrae comes from branches of the vertebral arteries, which are a pair of arteries that originate from the subclavian arteries in the chest and run up the back of the neck through the vertebrae.
- The vertebral arteries give off branches that supply blood to the cervical vertebrae, spinal cord, and surrounding muscles and tissues.
- In addition to the vertebral arteries, the cervical vertebrae also receive blood supply from branches of the ascending cervical artery, a branch of the inferior thyroid artery.
- This artery runs up the front of the neck and supplies blood to the anterior muscles of the neck and the cervical vertebrae.
- The lymphatic vessels of the cervical vertebrae drain into the deep cervical lymph nodes.
- These lymph nodes are located along the internal jugular vein and receive lymphatic drainage from the cervical spine, thyroid gland, and other structures in the neck.
- The deep cervical lymph nodes then drain into the thoracic duct, which is the largest lymphatic vessel in the body, and ultimately into the venous system.
Overall, the blood supply and lymphatic drainage of the cervical vertebrae are important for maintaining the health and function of the neck and surrounding structures.
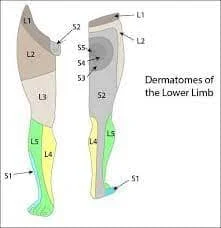
Nerves
The cervical spine works as bony protection of the spinal cord as it is life at the cranium. In spite of the presence of 7 cervical vertebrae, there are 8 pairs of cervical nerves, termed C1 to C8. C1 to C7 exit the spine cranially to its associate vertebrae, while C8 exits caudally to C7.
- Direct innervation of the spinal column is highly difficult, yet 3 discrete innervation sources have been identified in the ventral compartment of the cervical spine such as
- branches of the sympathetic trunk
- sympathetic rami communicates
- perineural vascular plexus of the vertebral arteries
- Meanwhile, the posterior aspect of the cervical spine gets innervation by the medial branch of the posterior primary rami.
- Coursing through the intervertebral foramen with the vertebral arteries, the vertebral nerves are thought to supply extra sympathetic innervation.
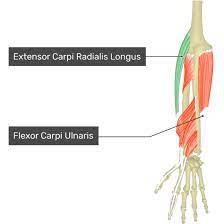
Muscles
The cervical vertebrae are connected by muscles, ligaments, and tendons, which help to support and move the head and neck. Some of the major muscles associated with the cervical vertebrae include:
Sternocleidomastoid-
This muscle runs from the base of the skull to the sternum and clavicle and helps to rotate and flex the neck.
Splenius muscles-
The splenius muscles are a group of muscles that extend from the upper thoracic vertebrae to the base of the skull and help to extend and rotate the neck.
Erector spinae muscles-
These muscles run along the length of the spine and provide support and stability to the vertebral column.
Semispinalis muscles-
These muscles extend from the upper thoracic vertebrae to the base of the skull and help to extend and rotate the neck.
Scalene muscles-
The scalene muscles are a group of muscles that run from the cervical vertebrae to the first and second ribs and help to elevate the ribs during inhalation.
These muscles work together to provide stability and movement to the cervical spine, allowing for a range of motion in the neck and head. Dysfunction or injury to these muscles can result in neck pain, stiffness, and reduced range of motion.
Physiologic Variants
Several physiological variations can occur in the cervical vertebrae.
Cervical ribs:
This is a rare condition in which an extra rib forms on the seventh cervical vertebrae. It occurs in less than 1% of the population and is usually asymptomatic.
Vertebral foramen size:
The size of the vertebral foramen, which is the opening through which the spinal cord passes, can vary from person to person.
The shape of spinous processes:
The spinous processes, which are the bony protrusions on the back of the vertebrae, can have different shapes and sizes. This variation is usually not clinically significant.
Fusion of vertebrae:
Sometimes, two or more cervical vertebrae can fuse. This is usually asymptomatic, but in some cases, it can cause problems with neck movement or nerve function.
Cervical lordosis:
The cervical spine normally has a slight curve called lordosis. However, some people may have an exaggerated or reduced curve, which can lead to neck pain or stiffness.
It is important to note that these physiological variations are usually not problematic, and many people can live their whole lives without even knowing they have them. However, if you experience neck pain or other symptoms, it’s always a good idea to consult a medical professional.
Surgical Considerations
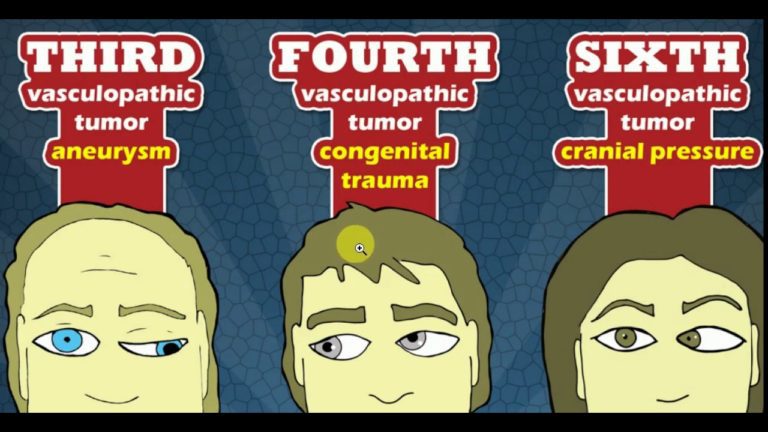
- The cervical spine is close to many important structures in the head and neck.
- Most surgical interventions in the cervical spine are either done via an anterior approach or a posterior midline approach.
- The anterior approach to the cervical spine is utilized to expose vertebral bodies from C2 to T1.
- It is examined for anterior cervical diskectomy and fusion, corpectomy and fusion, cervical disk replacement, tumor resection, fracture, and infection.
- Physician preference dictates the side of access.
- A left-sided approach is frequently favored since the recurrent laryngeal nerve demonstrates a less variable course as compared to the right side, and injury to this nerve may result in vocal cord paralysis and hoarseness.
- However, clinical significance stays controversial.
- The exterior dissection either divides or transects the platysma muscle at the desired level.
- The sternocleidomastoid muscle is then recognized and retracted laterally, protecting the carotid sheath and leaving the strap musculature medially. In this layer, careful dissection is necessary to avoid injury to the structures within the sheath.
- Deeply, the trachea and esophagus are retracted medially to permit access to the longus colli muscles.
- The longus colli is further divided longitudinally and retracted laterally, reveal the anterior longitudinal ligament that located on the vertebral bodies and disks.
- Careful retractor placement and dissection are necessary to avoid any kind of injury to the trachea, esophagus, and stellate ganglion, typically situated near the lateral border of the longus colli muscles at the level of C6. I
- Injury of this sympathetic structure may result in Horner syndrome, characterized by ptosis, anhydrosis, miosis, enophthalmos, and loss of ciliospinal reflex on the affected side.
- Postoperative lateral X-ray of the cervical spine is important in diagnosing any soft tissue swelling.
- The soft tissue shadow anterior to the cervical spine should be less than ten mm at the level of C1, less than five mm at C3, and less than fifteen to twenty mm at the level of C6.
- The posterior approach to the cervical spine utilizes a midline plane in the middle of the paraspinal musculature.
- Adequate hemostasis and retractor placement at the time of this approach is again necessary to reduce bleeding from the muscles.
- This approach permits access to the posterior elements of the cervical spine and is utilized for multiple procedures, incorporating laminectomy, laminoplasty, foraminotomy, and posterior cervical instrumentation.
- The particular anatomy of the cervical spine does not permit the safe placement of pedicle screw fixation; this is primarily because the pedicles of C3 to C6 are tiny and near the vertebral arteries.
- Rather, lateral mass screw placement is preferred.
- Careful placement of lateral mass screws frequently achieved with radiographic navigation is suggested to reduce the risk of injury to the vertebral arteries.
- The safe placement of pedicle screws is generally possible in C2 and C7.
- Fractures of the upper thoracic spine are more often accessed via a posterior approach.
- The rare anatomy of this spinal segment begets particular risks that warrant consideration at the time of surgical intervention.
- At the time of placement of lateral mass screws at the level of the atlas, dissection of the posterior arch should not incorporate more than 1.5 cm of lateral exposure from the midline to reduce the risk of injury to the vertebral arteries.
- When fixing C1 lateral mass screws, the screw should be angled 10 to 15 degrees medially to keep away the laterally passing vertebral artery.
- Trans articular screw placement at the junction of C1-C2 also brings a risk of vertebral artery injury as the screw passes the pars interarticularis of C2.
- Apart from this, C2 pedicle screw placement carries minimal risk of vertebral artery injury, but based on screw length, it does confer some risk of internal carotid artery injury.
- In cases that include the fusion of the upper cervical spine, the surgeon must teach the people about the risk of potential loss of half of the movement in the rotational and flexion-extension planes of the cervical vertebrae.
Clinical Significance
- Specific literature has shown that upwards of ten percent of the adult population suffers from ”frequent” episodes of neck pain, described as at least 3 instances of pain in a year.
- While this number alone would constitute far-reaching prevalence, it can be a conservative estimate.
- Other research has found the prevalence of neck pain to be the 4th leading cause of global disability, with an annual prevalence rate of neck pain as high as thirty percent. As such, neck pain exists as a significant socioeconomic burden.
- It is often classified depending on time (acute, subacute, or chronic) or mechanistically (mechanical, neuropathic, or referred).
- Neck pain can also come about secondary to rheumatologic conditions.
- Acute neck pain frequently comes from trauma or sports injury.
- Make sure the stability of the cervical spine is paramount to stop any further deleterious consequences.
- A greater range of pathology in the upper cervical spine may result, incorporating fractures of the occipital condyle, the atlas, and the dens or atlas of C2.
- Other diagnoses incorporate dislocations involving the craniocervical and atlantoaxial junctions.
- Likewise, in the subaxial cervical spine, there is a similarly greater variety of acute-injury pathology.
- Regardless of location, the specific features of cervical spine injury dictate its management and treatment.
- Missed or incorrect diagnoses may have serious long-term costs, given the high neurological stakes.
- Thus, cross-table radiography and computed tomography (CT) scans are invaluable tools for evaluating fractures or altered spatial relationships between vertebrae, whereas MRI is preferable in cases incorporating the potential spinal cord and soft tissue injury.
- Subacute and chronic neck pain also share different etiology.
- Arthritis of cervical facet joints is a usual cause of mechanical neck pain.
- However, Pinched nerve roots, slipped intervertebral disk, and cervical spinal canal stenosis is the most common peripheral neuropathic condition related to cervical- neck pain.
- A comprehensive history and physical examination may assist in differentiating between neuropathic and mechanical neck pain.
- In some cases, patients can benefit from diagnostic imaging and further workup to produce a proper diagnosis and treatment plan.
FAQ
The most important anatomical features of a typical cervical vertebra that dispatch it from other forms of vertebrae are
tiny size, transverse foramina, saddle-shaped part, and bifid spinous process. The atlas (C1) does not have any kind of body or spinous process.
The cervical spine consists of the first 7 vertebrae in the spine. It gives support for the weight of the head, surrounds and protects the spinal cord, and permits a wide range of head motions.
The cervical spine, comprised of 7 cervical vertebrae referred to as C1 to C7, is divided into 2 major segments: the craniocervical junction (CCJ) and the subaxial spine. The CCJ involves the occiput and the 2 most cephalad cervical vertebrae, identify as the atlas (C1) and the axis (C2).
The 1st cervical nerve emerges from the vertebral canal between the occipital bone and the atlas and is therefore known as the suboccipital nerve; the eighth issue between the 7th cervical and 1st thoracic vertebræ.
C3 root compression is very infrequent and can come with pain and numbness around the mastoid and pinna. C4 root compression can cause pain and numbness in the backside of the neck, over the scapula, and sometimes the anterior chest.



One Comment