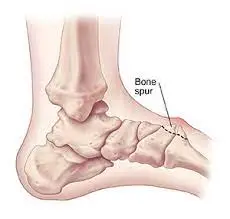
Bone Spur on the top of the Foot
Table of Contents
Description
A bone spur on the top of the foot, also known as a dorsal exostosis, is a bony outgrowth that can develop on the upper surface of the foot. This condition typically occurs at the joints or tendons, often in response to prolonged stress, friction, or pressure.
Bone spurs are usually a result of the body’s attempt to repair itself, leading to the growth of extra bone tissue. While bone spurs themselves may not cause significant discomfort, they can lead to pain, inflammation, and restricted movement if they impinge on nearby soft tissues or nerves.
A bone spur on the top of the foot tends to be a bony outgrowth that generates on the upper side of a bone in the foot, especially on the rearward( upper) side. It generally creates in response to nonstop pressure, disunion, or stress on the bone.
Bone spurs may get pain and discomfort, especially when walking or wearing shoes, and can require medical diagnosis and treatment if they come problematic. However, it’s necessary to consult a healthcare professional for a better diagnosis and operation, If a person finds they have a bone spur.
Anatomy of foot
The anatomy of a bone spur on the foot includes the following factors
Bone-
The spur comes from a bone in the foot, generally because of repetitious stress or disunion. The most usual bones involved are the metatarsal bones, which are long in the forefoot.
Cartilage-
As time passes time, as a response to the stress, the bone can produce changes in the cartilage covering its face, leading to the formation of a bone spur.
Ligaments and Tendons-
Ligaments and tendons attach to the bones in the foot. However, they may contribute to the formation of bone spurs, If these structures are under strain or inflammation.
Soft tissue-
The formation of a bone spur can be told by soft tissue near the affected area, similar to muscles and fascia.
It’s necessary to note that bone spurs themselves might not generally become symptoms. still, if impingement on the surroundings tendons, or soft tissue they may lead to pain, swelling, and discomfort. Better diagnosis and treatment by a physician may help manage the condition effectively.
Epidemiology of bone spurs on the top of the foot
Bone spurs on the foot may be in people of all periods but are more usual as individuals get aged. The liability of developing bone spurs increases with age, as wear and tear on the bones and joints over time may tend to their formation. Many factors can contribute to the threat of developing bottom bone spurs, including
Age-
As mentioned before, bone spurs come more current with age.
Physical exertion-
Individuals who engage in repetitious conditioning or sports that put stress on their bases, such as running or dancing can be at an advanced threat.
Footwear-
Ill-fitting or inadequately probative shoes may contribute to the development of bone spurs.
Foot Conditions –
Many foot conditions, likely plantar fasciitis or arthritis, may improve the threat of bone spurs.
Genetics –
There might be an inheritable predilection to developing bone spurs.
It’s necessary to flash back that people’s experiences may vary, and not everyone with threat factors will develop bone spurs. However, it’s better to seek medical evaluation from a well-known physician for accurate opinion and applicable treatment, If a person suspects they have a bone spur or are passing foot pain.
Causes of a bone spur on top of the bottom
Bone spurs on the bottom can develop due to colorful factors, including
Aging-
As people age, the cartilage in their joints may tear down, leading to the development of bone spurs as a natural part of the aging process.
Repetitious Stress-
Nonstop pressure and stress on the bones and joints of the foot can affect conditioning similar to running, jumping, or dancing. Over time, this repetitious stress can lead to the formation of bone spurs.
Footwear Wearing-
Ill-fitting or unsupportive shoes can get abnormal pressure on certain areas of the foot, contributing to the development of bone spurs.
Foot Injuries –
Former foot injuries, fractures, or surgeries can produce an environment where bone spurs are more likely to form.
Foot scars-
Structural abnormalities in the foot, similar to flat bases or high bends, may alter the distribution of pressure and get bone spurs to develop.
Arthritis-
Certain types of arthritis, similar to osteoarthritis or rheumatoid arthritis, can lead to common degeneration and bone spur conformation.
Tendinitis or Plantar Fasciitis-
Habitual inflammation of tendons or the plantar fascia( a ligament-like structure on the foot of the bottom) can stimulate the formation of bone spurs in response to ongoing stress.
- It’s necessary to note that not everyone who feels these factors will create bone spurs.
- Some people may be more genetically fitted to their conformation or may be more susceptible due to a combination of factors.
- However, it’s better to seek medical evaluation from a healthcare professional for accurate opinion and applicable treatment, If you suspect you have a bone spur or are passing bottom pain.
Symptoms of a bone spur on top of the bottom
The symptoms of a bone spur on the foot can vary depending on its position and whether it affects near tissue or nerves. Common symptoms may include
Pain-
Persistent or intermittent pain in the affected area of the foot especially during walking or when putting pressure on the bottom.
Swelling-
The presence of swelling or tenderness around the bone spur.
Redness-
In some cases, the skin over the bone spur may appear red.
Limited Range of Motion –
Difficulty moving the affected foot or a dropped range of motion in the near joint.
Corns or Calluses-
Bone spurs can get increased pressure on specific areas of the foot leading to the development of corns or calluses.
Tingling and numbness-
If the bone spur presses on near nerves it may lead to sensations of chinking, impassiveness, or weakness in the foot.
Stiffness –
Stiffness in the foot or near joint, especially after ages of rest.
- It’s important to remember that some people with bone spurs may not witness any symptoms at each, while others may have severe pain and discomfort.
- However, it’s necessary to seek medical evaluation from a healthcare professional for accurate opinion and applicable treatment, If you suspect you have a bone spur or are passing foot pain.
- They can recommend the best course of action based on your condition and medical history.
Differential diagnosis of bone spurs on the top of the bottom
The symptoms of a bone spur on the foot can be similar to other foot conditions. A healthcare professional will perform a thorough evaluation and consider various different judgments to directly identify the beginning issue. Some possible situations that may be considered in the differential diagnosis of a bone spur of the foot include;
Plantar Fasciitis-
Inflammation of the plantar fascia, a thick ligament- like structure on the top of the foot, can cause heel pain.
Metatarsalgia-
Pain and inflammation in the ball of the foot, are frequently due to increased pressure on the metatarsal bones.
Morton’s Neuroma-
A thickening of the tissue around a nerve between the toes, leading to pain, burning, or thickening sensations.
Tendinitis-
Inflammation of a tendon in the foot, which can get localized pain and limited range of motion.
Arthritis-
Different types of arthritis, similar to osteoarthritis or rheumatoid arthritis, can affect the joints of the foot and get pain and stiffness.
Stress Fractures-
Small hairline fractures in the bones of the foot are frequently caused by repetitious stress or overuse.
Gout-
A type of inflammatory arthritis is performed from the buildup of uric acid chargers in the joints, leading to unforeseen and severe pain, swelling, and greenishness.
Bursitis-
Inflammation of the bursae, a fluid-filled cushion that cushion and reduce disunion between bones, tendons, and muscles.
Nerve compression-
Compression of nerves in the foot or ankle region can get colorful symptoms, similar to pain, thickening, and numbness of a bone spur on top of the foot.
Diagnosis of the bone spur on the top of the foot
The diagnosis of a bone spur of the foot generally involves a combination of medical history, physical examination, and imaging studies. Then is how the process generally unfolds.
Medical History-
Your healthcare provider will begin by asking about your symptoms, including the location and nature of the pain when it started, and any conditioning that may worsen or palliate the pain.
Physical Examination-
The physician will perform a thorough physical examination of your foot checking for areas of tenderness, swelling, or redness. They will also assess your foot’s range of motion and check for any abnormalities.
Imaging Studies-
X-rays are generally used to confirm the presence of a bone spur and give a detailed view of the bone structures in the foot. X-rays can help identify the size, shape, and position of the bone spur, as well as assess its impact on near tissue and joints.
Other diagnostic tests-
In some cases, fresh imaging studies like MRI or CT reviews may be recommended to get a more detailed view of the bone and surroundings soft tissue.
Differential diagnosis-
As mentioned before, the physician will consider other possible conditions with similar symptoms to rule out indispensable causes of foot pain.
- Once the opinion is verified, the healthcare provider will discuss the findings with you and recommend applicable treatment options.
- Treatment may include conservative measures similar to rest, physical remedies, orthotic devices, and pain operations.
- In severe cases or when conservative measures are ineffective, surgical treatment of the bone spur may be considered.
It’s essential to seek professional medical advice for an accurate opinion and substantiated treatment plan grounded on your specific condition and medical history.
Treatment of the bone spurs on the top of the foot
Medical treatment for a bone spur on the top of the leg usually involves a combination of conservative measures to relieve symptoms and manage the condition. Below given are some of the more common ones;
Medical treatments:
Rest and activity:
Avoid activities that make the pain worse and give the foot time to rest and heal.
Pain:
Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may help reduce pain and decrease inflammation.
Ice pack:
Using ice on the involved area may help decrease swelling and reduce pain. Cover the skin with a sheet or cloth and apply ice for about 10-20 minutes every few hours as needed.
Shoe changes:
Comfortable, well-fitting shoes with adequate support can help reduce pressure in the sphere of influence.
Orthotics:
Custom or over-the-counter shoe inserts can provide additional support and cushion to the foot, reducing pressure on the socket.
Physical therapy:
A physical therapist can recommend exercises and stretches to improve leg strength and flexibility, which can help reduce pain and prevent further complications.
Corticosteroid injections:
In some cases, a doctor may give a corticosteroid injection to reduce inflammation and pain in the affected area.
Immobilization:
A temporary brace, splint, or cast may be recommended to immobilize the leg and promote healing.
If conservative treatment does not provide adequate relief, or if the bone mass significantly impairs daily activities and causes severe pain, surgical removal of the bone mass may be considered. Surgery is usually a last resort and is performed by an orthopedist or foot surgeon.
Physiotherapy treatment
Physical therapy can play a vital role in the treatment of bone spurs on the top of the foot. A physical therapist can create a personalized treatment plan to address the symptoms and causes of the condition. Below given are some of the more common ones;
Stretching exercises:
A physical therapist may prescribe specific stretches to improve flexibility in the leg and surrounding muscles. Stretching can help reduce tension and relieve pressure on the bone spur.
Toe curls:
- Begin with sitting or standing with the feet on the floor.
- Bend your toes inward, trying to grab the floor, then release.
- Repeat this movement 1o times.
Toe Stretch:
- Start with sitting in a chair and cross one ankle over the opposite knee.
- Gently pull the toes of the crossed leg back toward the calf until you feel a stretch in the upper leg and ankle.
- Keep for 10-15 seconds and change to the opposite leg.
Plantar Fascia Stretch:
- Start with standing facing a wall with your hands against it.
- Step back with one foot, keeping it on the ground, and slightly bend the front knee.
- Bend forward, pushing your hips toward the wall until you feel a stretch along the back arch of your foot.
- Keep for 10 to 20 seconds.
Calf stretch:
- Start with standing against a wall with your hands against it.
- Step one leg back and keep it straight by bending the front knee.
- Press your back heel down to the floor until you feel a stretch in the calf of your back leg.
- Maintain for 10-20 seconds and change to the other leg.
Achilles Tendon Stretch:
- Similar to calf stretch, but this time keep the back and knee straight.
- Lean against the wall until you feel a stretch in the back of your ankle and lower leg.
- Maintain for 10-20 seconds and switch to the other leg.
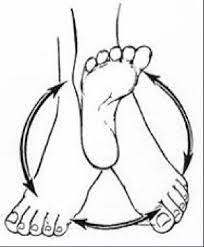
Ankle circles:
- Start with sitting in a chair with your feet slightly off the ground.
- Rotate the ankles in both clockwise and counterclockwise circular motions.
Foot roller:
- Start with sitting in a chair and placing a tennis ball or foam roller under your foot.
- Using light pressure, roll the foot over the ball or roller to massage the bottom of your foot.
- Remember to take these stretches easy and slowly.
- Avoid forcing or extending the movement to the point of pain.
- If you have an existing foot or ankle condition or experience pain during these stretches, it is important to consult a doctor or qualified physical therapist before continuing with these exercises.
- They can offer personalized advice and modifications to suit your needs.
Strengthening exercises:
Targeted exercises can strengthen the muscles that support the foot and ankle, providing better stability and reducing stress on the affected area. Exercises to strengthen feet and ankles can help improve stability, support, and overall function. Here are some effective exercises to strengthen your foot and ankle muscles:
Toe standing:
- Start with standing with your feet on the ground.
- Slowly lift your heels off the floor, placing your weight on the balls of your feet.
- Lower your back slowly.
- Repeat 10 times.
Toe Grips:
- Place a towel or small cloth on the floor while sitting or standing.
- Crumple the fabric with your toes and grab it by pulling it towards you.
- Release and repeat.
Ankle Alphabet:
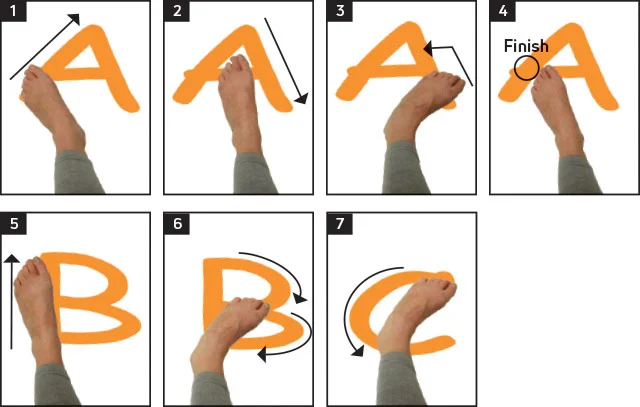
- Start with sitting in a chair with your legs extended.
- Imagine that your big toe is a pencil and “write” the alphabet in the air using your foot and ankle movements.
Resistance Band Ankle Flexion:
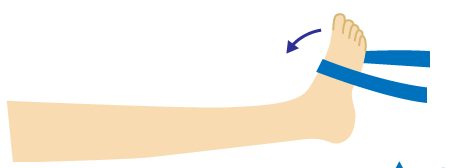
- Sit down on the floor with your legs outstretched to start.
- Wrap the resistance band around the ball of one foot and hold the ends with your hands.
- Bend your ankle against the resistance of the strap.
- Release slowly and repeat.
Resistance band ankle extension:
- Similar to the previous exercise, this time wrap the band around the back of your leg and bend your leg against the resistance.
Ankle twist and turn:
- Start with sitting in a chair with your feet slightly off the ground.
- Turn the leg inward (inversion) and then outward (rotation) against resistance.
- You can use your hand or a resistance band to add resistance.
Picking up marbles:

- Place marbles or small objects on the floor, pick them up on your toes, and move them to the container. Heel.
Walking on heels:
- Walk on your heels, lifting your toes off the ground with each step.
- This exercise targets the front leg muscles.
Towel Curls:
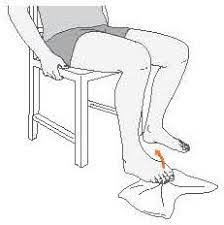
- Start with sitting on a chair with your feet on the floor.
- Place a small towel under your toes and use your toes to crumple and curl the towel toward you.
- Do these strengthening exercises regularly, aiming for 2-3 sets of 10-15 repetitions for each exercise.
- Slowly increase the resistance or weight as your strength enhances.
- If you have foot or ankle problems or experience pain during these exercises, it is important to consult a doctor or qualified physical therapist for guidance and modifications.
- They may deliver personalized advice tailored to your specific needs and circumstances.
Foot mobilization techniques:
Gentle mobilization techniques can help improve joint mobility and reduce leg stiffness. Foot mobilization techniques are hands-on manual therapy techniques used to improve joint mobility, reduce stiffness and promote proper alignment of the foot and ankle. These techniques are usually performed by a qualified physician such as a physical therapist or chiropractor. Some common leg mobilization techniques include:
Joint glides:
Gentle sliding movements on the foot joints to improve and reduce their movement restrictions.
Joint distraction:
Applying traction or traction to a joint to create space and relieve pressure, promotes joint mobility.
Joint compressions:
Apply light pressure to the joint to encourage fluid movement in the joint capsule and improve joint mobility.
Passive range of motion:
The therapist moves the foot and ankle through a range of motion without the active participation of the patient to improve joint flexibility.
Soft tissue mobilization:
The therapist uses his hands to compress and stretch the soft tissues around the leg, such as muscles, tendons, and ligaments.
Joint techniques:
These include rhythmic vibration or gentle shaking applied to the foot and ankle to improve joint mobility.
Mulligan Concept:
A special mobilization technique that uses manual gliding to improve joint alignment and function.
Muscle Energy Techniques:
Techniques in which the patient actively contracts certain muscles while the therapist mobilizes the joint to improve joint movement.
Taping:
Application of special tapes or straps to support and stabilize the foot and ankle, promoting proper alignment and mobility.
Foot mobilization techniques are often used in conjunction with other physical therapy procedures to create a comprehensive treatment plan based on the needs and conditions of the individual. These techniques must be performed by trained professionals to ensure safety and effectiveness. If you have foot or ankle sprains, it is important to seek the guidance of a qualified healthcare provider for proper evaluation and appropriate treatment.
Manual Therapy:
Hands-on techniques, such as massage and joint mobilization, can help reduce pain and improve circulation in the affected area. Massage can be beneficial for foot spurs by reducing muscle tension, increasing blood flow, and promoting relaxation. However, it’s essential to approach massage with caution and avoid direct pressure on the bone spur itself to prevent exacerbating the condition. Here are some massage techniques that can help with foot spurs:
Effleurage:
Use gentle, gliding strokes along the top and bottom of the foot to warm up the tissues and prepare them for deeper work.
Petrissage:
Perform kneading movements on the muscles of the foot, focusing on the calf muscles and the plantar fascia, but avoiding direct pressure on the bone spur.
Circular Frictions:
Use circular movements with your thumbs or fingers to target specific areas of tension, but avoid direct pressure on the bone spur.
Trigger Point Release:
Locate trigger points (knots in the muscles) in the foot and apply sustained pressure to release tension. Again, avoid direct pressure on the bone spur.
Toe Stretching:
Gently stretch and wiggle the toes to improve flexibility and relieve tension in the foot.
Heel Squeezes:
Gently squeeze the heel with your hands to release tension in the plantar fascia.
Ankle Circles:
Perform circular movements with your hands around the ankle joint to improve mobility and reduce stiffness.
- Remember, the main goal of the massage is to provide relaxation and alleviate muscle tension in the foot and ankle.
- Avoid putting direct pressure on the bone spur, as it may worsen the symptoms.
- If you’re experiencing foot pain or have a bone spur, it’s essential to consult with a healthcare professional or a qualified massage therapist who is familiar with foot conditions to make sure safe and effective massage techniques are tailored to the specific requirements.
- They can help you determine the most suitable massage approach for your condition.
Gait Analysis:
The physiotherapist may assess your walking or running gait to identify any abnormalities that could contribute to the development of the bone spur. Correcting gait mechanics can alleviate pressure on the affected area.
Ultrasound or Electrical Stimulation:
These modalities may be used to provide pain relief and promote healing in the affected tissues.
Footwear Advice:
The physiotherapist can recommend appropriate footwear with adequate support and cushioning to reduce pressure on the bone spur.
Activity Modification:
Modifying or avoiding certain activities that worsen the symptoms can help in the healing process.
Home Exercise Program:
The physiotherapist may provide you with a set of exercises and self-management strategies to continue your rehabilitation at home.
- The goal of physiotherapy is to reduce pain, improve function, and enhance overall foot health.
- It’s essential to follow the recommended treatment plan consistently and communicate with the physiotherapist about your progress and any concerns.
- If conservative measures do not yield satisfactory results, the physiotherapist may work in collaboration with other healthcare professionals to explore other treatment options, including medical interventions or surgery, if necessary.
FAQ
Degenerative diseases involving osteoarthritis and rheumatoid arthritis are frequently to blame for bone spurs on the top of the foot. These conditions weaken joint cartilage, resulting in bone-on-bone contact. Bone spurs grow as a consequence of the improved strain on the bones.
Once formed, heel spurs are endless. Surgery is the greatest way to release a heel spur. Since heel spurs usually don’t hurt, treating the condition that caused the heel spur should help ease the heel pain.
This method may result in scar tissue accumulation and over many years may build up causing bone spurs and permanent damage. Good Vitamin K2 levels help control the buildup of calcium in these damaged tissues. Vitamin K2 production in the body is conditional on healthy gut flora and the consumption of fermented food.
Insufficient calcium and other bone-building minerals put the bones at risk for osteoporosis, fractures, and bone spurs.