Becker Muscular Dystrophy (BMD):
Table of Contents
What is Becker’s Muscular Dystrophy?
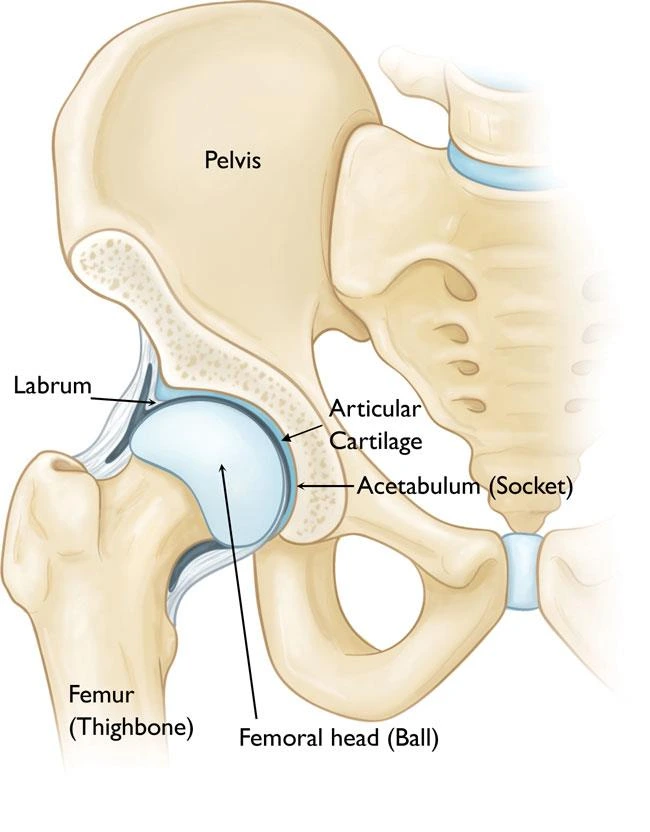
Becker muscular dystrophy affects the muscles of the hips, pelvic site, thighs, shoulders, and heart.
It is one of 9 types of muscular dystrophies, degenerative diseases primarily affecting voluntary muscles, and a group of genetics. BMD is similar to DMD but allows the voluntary functions of muscles better than in DMD.
BMD is a group of dystrophinopathies including Duchenne muscular dystrophy (DMD) and an intermediary form between DMD and BMD.
Becker muscular dystrophy has a later onset and mild symptoms compared to DMD.
In both BMD and DMD, the heart muscle can be affected similarly.
The heart muscle can be affected similarly to the way it can be in DMD.
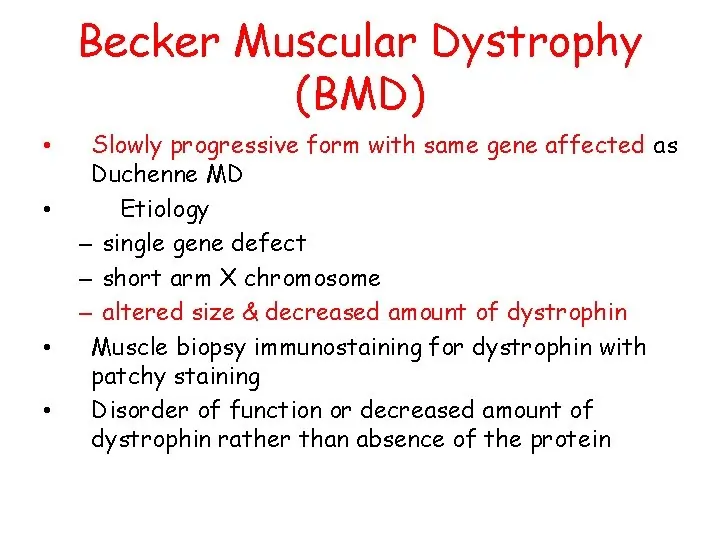
What are the Causes of Becker Muscular Dystrophy (BMD)?
Becker muscular dystrophy is caused by an alteration in a protein called dystrophin. The inadequate gene is located in the chromosomal, and the defect is inherited as an X-linked recessive trait. Patients without a clear X-linked pattern of patrimony may have defects in other genes, affecting the dystrophin-associated glycoproteins.
Inheritance
All individuals inherit two copies of most genes. The number of models of a gene that need to have a disease-causing variant impacts the way a disease is inherited.
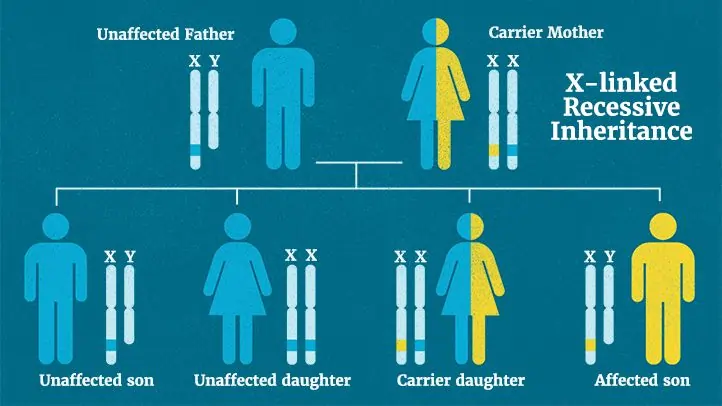
X-linked recessive inheritance:
X-linked means the gene is located on the X chromosome complement, one of two sex chromosomes. Genes, like chromosomes, usually come in pairs. Recessive means that when there are two copies of the accountable gene, both copies must have a disease-causing change (infective variant) in order for a person to have the disease. Variation is an older term that is still sometimes used to mean pathogenic variant.
Because women have two X chromosomes, an infective variant for an X-lined recessive disease generally needs to occur in both copies of the gene to cause the disease. Because men have one X chromosome and thus only one copy of the gene, a pathogenic variant in their one copy is enough to cause the infection.
A woman who bears one X-linked gene variant has a 50% (1 in 2) chance of having a son with the disease and a 50% (1 in 2) chance of having a daughter who is a carrier. A man with an X-linked recessive disease cannot pass on the disease to his boys, but all of his bear’s girls will be carriers. If a male child is the first person in a family with the disease, the infected variant may have been innate from the mother or may have occurred by chance for the first time in the child.
Signs and symptoms of Becker Muscular Dystrophy (BMD):
Some symptoms persistent with Becker muscular dystrophy are:
- Difficulty breathing.
- Muscle weakness gradually increased difficulty with walking.
- Severe upper extremity muscle weakness.
- Skeletal deformities of the chest, and back (scoliosis).
- Pseudohypertrophy of calf muscles.
- Muscle pain.
- Heart muscle problems.
- Elevated creatinine kinase levels in the blood.
Individuals with this disorder typically experience progressive muscle weakness of the leg and pelvis muscles, which is connected with a loss of muscle mass (atrophy). Muscle weakness also occurs in the arms, neck, and other regions, but is not as significantly severe as in the lower half of the body.
Calf muscles initially enlarge during the ages of 5-15 (an attempt by the body to compensate for the loss of muscle strength), but the enlarged muscle tissue is eventually replaced by fat and connective tissue (pseudohypertrophy) as the legs become less used (with use of a wheelchair).
Investigations:
Initial investigations:
Serum creatine kinase (CK) – shows a diminish-severe increase in BMD.
Raised CK levels in this scenario value specialist referral for further examination.
Further investigations:
Genetic examination.
Muscle biopsy- for dystrophin maculation.
Genetic tests and advice for the family.
Controlling for cardiomyopathy.
Differential Diagnosis:
Duchenne muscular dystrophy: More rigorous and initial onset than BMD. Prognostication is not good.
Polymyositis: The absence of distal pseudohypertrophy helps in distinguishing it from BMD.
Spinal muscular atrophy: The absence of dystrophin gene alteration in a DNA probe provokes spinal muscular atrophy as an alternative diagnosis.
Limb-girdle Muscular Dystrophy: This condition is hard to distinguish from BMD; however, calf muscle pseudohypertrophy is absent.
Dilated cardiomyopathy: cardiomyopathy is one of the most serious complications and the leading cause of death in dystrophies. But enlarged cardiomyopathy can be a separate existence with a different genetic etiology or from other causes apart from muscular dystrophy.
Emery-Dreyfuss muscular dystrophy: Early spasms and cardiac defects help to distinguish it from BMD.
Myasthenia gravis: Fluctuating skeletal muscle weakness spasms stimulate the clinical presentation of BMD, but facial weakness, ptosis, and diplopia are common.
Metabolic myopathies: Most patients complain about muscle weakness and pain during exercise rather than during rest.
Treatment of Becker Muscular Dystrophy (BMD):
Medical Management:
No medications are provided to patients for the particular treatment of BMD.
Medications are commanded to treat symptoms that are commonly associated with BMD (such as cardiac medications for heart disorder).
Corticosteroid medications are used to help particulars remain able to walk for as long as possible by delaying the inflammatory procedure.
Physiotherapy Treatment of Becker Muscular Dystrophy (BMD):

Patient and family education is significant in these cases.
Passive and Active stretching to enhance joint flexibility (ROM) and prevent or defer the development of contractures.
Activities such as riding a bicycle and swimming can be used to improve cardiovascular fitness and force exercise. However, care should be taken that these activities are not difficult or exhausting, as they can cause more harm to the muscles.
Respiration training – In the initial stages of the condition, the physiotherapist will be difficult to help keep the child active. During later phases of the condition, the physiotherapist will help more with respiratory problems as well by using a spirometer, positioning, huffing, and coughing in an effective way.
Improving the child’s motor experimental skills and helping him reach the significant event by using Proprioceptive Neuromuscular Functioning|PNF techniques, various approaches like Roods, Brunnstrom and Bobath
Progressive resistance exercises with minimum weights without fatiguing the muscles.
Massage can be done on muscles to reduce pain.
Orthosis: Movability concerns are addressed, including the need for devices to assist with mobility, such as a scooter or a fully altered wheelchair with a usage seat and back, custom supports, and electric power.
Speech Therapy: Dysphagia concerns may be assessed by a speech therapist. Clinical evaluation may result in the suggestion to avoid specific food textures and liquid viscosities, as well as avoid certain places during feeding.
Recreational Therapy: Avocational needs, passions, and hobbies can be pushed to promote the well-being and overall physical health of the individual. These activities should be assessed based on the child’s interests and abilities. The various musical mechanisms, dances, crafts, art as well as yoga can be learned or motivated in the child.
Aerobic Exercise for Becker Muscular Dystrophy (BMD):
Aerobic exercise increases the heart rate. Those with muscular dystrophy should be able to exercise while maintaining communication. Aerobic exercise will depend on condition, but low-impact exercises such as fast dancing, walking, cycling, and swimming, are options.
Ideally, 20 minutes of exercise a day between four and six times per week, but you might want to start by doing five or 10 minutes a day and building your fitness levels up slowly. Ensure warm-up is done gently before stretching and exercising muscles, it decreases the chance of injury.
Some exercises and stretches are adapted for muscular dystrophy patients.
Stretching and Strengthening Exercise:
Forearm Supination
Position: Supine
Instructions: Forearm holds just above the wrist and turns the arm to a palm-up position. Stabilize the elbow at the side of the body. Hold for 60 seconds and then reposition after repeating 60 seconds.
Achilles(Gastrocnemius) Stretch
Position: Supine
Instructions: patient position is supine lying, place a small roll under the knee. Grip the heel and pull to stretch the Achilles then flex the foot. Hold for 60 seconds and then reposition after repeating for 60 seconds.
Position: Self Stretch
Instructions: The patient’s position is one foot in front of the other foot while standing at a wall. Keep the back knee straight, Lean forward and toes pointed forward. Hold for 60 seconds and after than relax and again repeat.
Hamstring Stretch
Position: Supine
Instructions: Stabilize at the knee and flex the hip 90 degrees. Slowly raise the lower leg until a stretch is felt in the back of the thigh, with another hand. Hold for 60 seconds and then reposition after repeating for 60 seconds.
Position: Wall Self Stretch
Instructions: position at the corner of two walls and place a heel on the wall and the other leg along the wall on the floor. Until a stretch is felt, slowly move closer to the wall in the back of the thigh. Hold for 60 seconds and repeat 1-2 times.
IT Band Stretch and Iliopsoas
Position: Supine at the edge of the plinth.
Instructions: Hold the knee with, and Pull it up then toward the chest. Hold for 60 seconds and then reposition after repeating 60 seconds.
Neck Extensor

Position: Self Stretch
Instructions: patient position is a comfortable neck position looking forward. Insert (Tuck) the chin down while extending the back of the neck. Hold 5-10 seconds and repeat 5-10 times.
Soleus Stretch
Position: Prone
Instructions: Flex your knee 90 degrees, while lying on your stomach, Stabilize the lower leg. Grip the foot and heel and press down to stretch the calf. Hold for 60 seconds and then reposition after repeating 60 seconds.
Trunk Rotation
Position: Self Stretch
Instructions: Patient position is supine lying with knees bent, swing them to one side allowing the hips and lower back to rotate in the same direction. Keep shoulders down. Hold for 10-20 seconds and then repeat on the other side and after repeating each side 10-20seconds.
Wrist Extension Stretch
Position: Seated
Instructions: Patient position is sitting position, place palms down at your side. Slowly move your hands backward until feeling the stretch. Hold for 60 seconds and then reposition after repeating for 60 seconds.
Wrist and Finger Extension
Position: Seated
Instructions: Slowly extend the wrist, and hold the palm with the second hand. Continuing to extend the wrist and finger, move one hand towards the fingers. Hold for 60 seconds and then reposition after repeating for 60 seconds.
Bridging
position: Supine lying
Instruction: Patient potion is supine lying position with knee bend. Tighten your abdominal muscles. Hips are raised off the floor until your hips are aligned with your knees and shoulders. Hold for three deep breaths.
The main motive of gait training exercises is to strengthen the muscles or improve stability.
Gait Training Exercises
- Walking on a treadmill.
- Lifting your legs.
- Sitting down.
- Standing up.
- Stepping over objects.
Complications of Becker Muscular Dystrophy (BMD):
Complications may arise in the form of:
- Cardiomyopathy, increasing damage of pulmonary and liver acts, loss of ambulation, cognitive disability, and bone fractures.
- High chance of postoperative chest disease.
- Rhabdomyolysis leads to myoglobinuria and subsequent kidney defeat.
- Corticosteroids cause adrenal deficiency and immunosuppression.





One Comment