ARTHRITIS OF ANKLE AND FOOT
Arthritis is inflammation of one or more of your joints. It can cause pain and stiffness in any joint in the body, and is common in the small joints of the foot and ankle. There are more than 100 forms of arthritis, many of which affect the foot and ankle.
lthough there is no cure for arthritis, there are many treatment options available to slow the progress of the disease and relieve symptoms. With proper treatment, many people with arthritis are able to manage their pain, remain active, and lead fulfilling lives.

Table of Contents
Related Anatomy
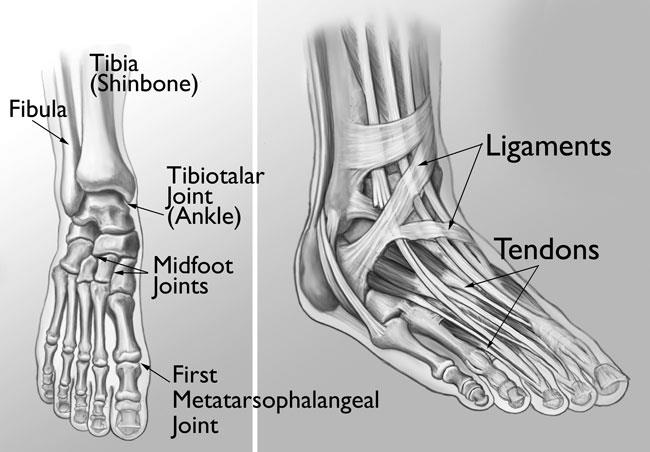
During standing, walking, and running, the foot and ankle provide support, shock absorption, balance, and several other functions that are essential for motion. Three bones make up the ankle joint, primarily enabling up and down movement. There are 28 bones in the foot, and more than 30 joints that allow for a wide range of movement.
In many of these joints the ends of the bones are covered with articular cartilage—a slippery substance that helps the bones glide smoothly over each other during movement. Joints are surrounded by a thin lining called the synovium. The synovium produces a fluid that lubricates the cartilage and reduces friction.
Tough bands of tissue, called ligaments, connect the bones and keep the joints in place. Muscles and tendons also support the joints and provide the strength to make them move.
Causes of Arthritis of Ankle and Foot
The major types of arthritis that affect the foot and ankle are osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
Osteoarthritis
Osteoarthritis, also known as degenerative or “wear-and-tear” arthritis, is a common problem for many people after they reach middle age, but it may occur in younger people, too.
In osteoarthritis, the cartilage in the joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful osteophytes (bone spurs).
In addition to age, other risk factors for osteoarthritis include obesity and family history of the disease.
Osteoarthritis develops slowly, causing pain and stiffness that worsen over time.
Rheumatoid arthritis is a chronic disease that can affect multiple joints throughout the body, and often starts in the foot and ankle. It is symmetrical, meaning that it usually affects the same joint on both sides of the body.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium covering the joint, causing it to swell. Over time, the synovium invades and damages the bone and cartilage, as well as ligaments and tendons, and may cause serious joint deformity and disability.
The exact cause of rheumatoid arthritis is not known. Although it is not an inherited disease, researchers believe that some people have genes that make them more susceptible. There is usually a “trigger,” such as an infection or environmental factor, which activates the genes. When the body is exposed to this trigger, the immune system begins to produce substances that attack the joints.
Posttraumatic Arthritis
Posttraumatic arthritis can develop after an injury to the foot or ankle. Dislocations and fractures—particularly those that damage the joint surface—are the most common injuries that lead to posttraumatic arthritis. Like osteoarthritis, posttraumatic arthritis causes the cartilage between the joints to wear away. It can develop many years after the initial injury.
An injured joint is about seven times more likely than an uninjured joint to become arthritic, even if the injury is properly treated. In fact, following an injury, your body may actually secrete hormones that stimulate the death of your cartilage cells.
Symptoms of Arthritis of Ankle and Foot
The symptoms of arthritis vary depending on which joint is affected. In many cases, an arthritic joint will be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There can be other symptoms, as well, including:
Pain with motion
Pain that flares up with vigorous activity
Tenderness when pressure is applied to the joint
Joint swelling, warmth, and redness
Increased pain and swelling in the morning, or after sitting or resting
Difficulty in walking due to any of the above symptoms
Physiotherapy Examination
Your doctor will discuss your overall health and medical history and ask about any medications you may be taking. He or she will examine your foot and ankle for tenderness and swelling and ask questions to understand more about your symptoms. These questions may include:
When did the pain start?
Where exactly is the pain? Does it occur in one foot or in both feet?
When does the pain occur? Is it continuous, or does it come and go?
Is the pain worse in the morning or at night? Does it get worse when walking or running?
Your doctor will also ask if you have had an injury to your foot or ankle in the past. If so, he or she will discuss your injury, including when it occurred and how it was treated.
Your doctor will also examine your shoes to determine if there is any abnormal or uneven wear and to ensure that they are providing sufficient support for your foot and ankle.
Gait analysis. During the physical examination, your doctor will closely observe your gait (the way you walk). Pain and joint stiffness will change the way you walk. For example, if you are limping, the way you limp can tell your doctor a lot about the severity and location of your arthritis.
During the gait analysis, your doctor will assess how the bones in your leg and foot line up when you walk, measure your stride, and test the strength of your ankles and feet.
Tests
X-rays. These imaging tests provide detailed pictures of dense structures such as bone. An x-ray of an arthritic foot may show narrowing of the joint space between bones (an indication of cartilage loss), changes in the bone (such as fractures), or the formation of bone spurs.

Weight-bearing x-rays are taken while you stand. They are the most valuable additional test in diagnosing the severity of arthritis and noting any joint deformity associated with it. In arthritic conditions, if x-rays are taken without standing, it is difficult to assess how much arthritis is present, where it is located in the joint, and how much deformity is present. So, it is very important that, when possible, x-rays are taken standing.
Other imaging tests. In some cases, a bone scan, computed tomography (CT) scan, or magnetic resonance imaging (MRI) scan may be needed to determine the condition of the bone and soft tissues.
Laboratory tests. Your doctor may also recommend blood tests to determine which type of arthritis you have. With some types of arthritis, including rheumatoid arthritis, blood tests are important for an accurate diagnosis.
Your doctor may refer you to a rheumatologist if he or she suspects rheumatoid arthritis. Although your symptoms and the results from a physical examination and tests may be consistent with rheumatoid arthritis, a rheumatologist will be able to determine the specific diagnosis. There are other less common types of inflammatory arthritis that will be considered.
Physiotherapy treatment
Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your foot and ankle. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
Although physical therapy often helps relieve stress on the arthritic joints, in some cases it may intensify joint pain. This occurs when movement creates increasing friction between the arthritic joints. If your joint pain is aggravated by physical therapy, your doctor will stop this form of treatment.
Assistive devices. Using a cane or wearing a brace—such as an ankle-foot orthosis (AFO)-may help improve mobility. In addition, wearing shoe inserts (orthotics) or custom-made shoes with stiff soles and rocker bottoms can help minimize pressure on the foot and decrease pain. In addition, if deformity is present, a shoe insert may tilt the foot of ankle back straight, creating less pain in the joint.