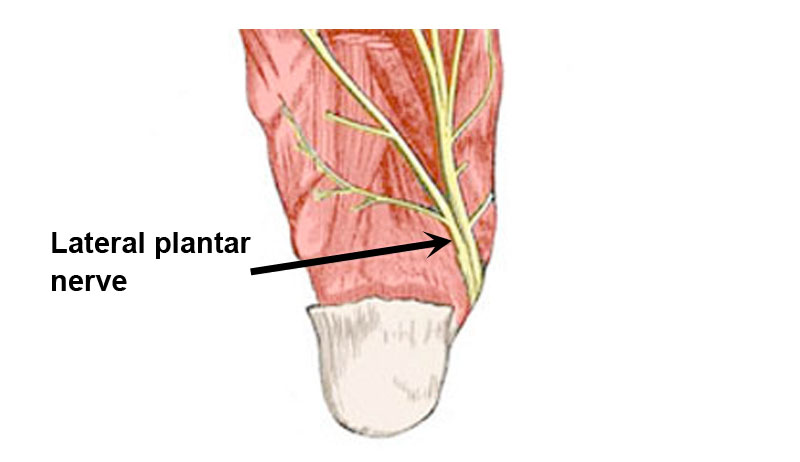
Lateral Plantar Nerve
Table of Contents
What is Lateral Plantar Nerve?
The distribution of the Lateral Plantar Nerve, also known as the External Plantar Nerve, is similar to that of the Ulnar Nerve in the Hand. It supplies the majority of the deep muscles as well as the skin of the fifth toe and the lateral portion of the fourth foot. Between the Flexor digitorum brevis and Quadratus plantae, it travels obliquely forward along with the lateral plantar artery to the lateral side of the foot. It separates into a superficial branch and a deep branch in the space between these two muscles. It provided Quadratus plantae and Abductor digiti quinti prior to division.
It travels deep to the proximal insertion of the abductor hallucis muscle before entering the sole of the foot. It continues between the flexor digitorum brevis and quadratus plantae muscles on the sole anteriorly and laterally, innervating both of these muscles. When that happens, it will split into deep and superficial branches just below the fifth metatarsal head.
Superficial branch: The lateral side of the little toe, the Flexor digiti quinti brevis, and the two interossei of the fourth intermetatarsal gap are supplied by the appropriate digital nerve, which is part of the superficial branch (ramus superficialis) as opposed to the common digital nerve. In order to feed the adjacent sides of the fourth and fifth toes, the common digital nerve splits into two proper digital nerves and interacts with the third common digital branch of the medial plantar nerve.
Deep branch: All of the Interossei, with the exception of those in the fourth metatarsal space, the second, third, and fourth Lumbricales, as well as the deep branch (ramus profundus; muscular branch), which runs next to the lateral plantar artery on the deep surface of the tendons of the Flexor muscles and the Adductor hallucis, supplies the Adductor hallucis muscle.
Anatomy of Lateral Plantar Nerve:
The sciatic nerve travels down the leg before splitting into the tibial nerve and common peroneal nerve close to the popliteal fossa. Even though it is not a distinct branch, the tibial nerve at the ankle is frequently referred to as the posterior tibial nerve.
The medial, lateral, and posterior plantar nerves all branch from the posterior tibial nerve as it descends the foot through the tarsal tunnel. The medial septum, which is located between the medial calcaneus and the deep fascia of the abductor hallucis, divides the independent medial and lateral plantar tunnels.
The clinically significant Baxter’s nerve or the inferior calcaneal nerve are two of the lateral plantar nerve’s divisions.
Origin: The tibial nerve’s a smaller terminal division
Course: The proximal connection of the abductor hallucis muscle is where the lateral plantar nerve enters the sole of the foot.
It then separates near the head of the fifth metatarsal into deep and superficial branches, continuing laterally and anteriorly over the sole between the flexor digitorum brevis and quadratus plantae muscles and supplying branches to both of these muscles.
Motor supply includes the adductor hallucis, flexor digiti minimi brevis, quadratus plantae, second, third, and fourth lumbricals, as well as the dorsal and plantar interossei.
Sensory supply: The lateral one-and-a-half digits’ of neighboring plantar surfaces and a strip of skin on the anterolateral anterior two-thirds of the sole serve as the sensory supply.
Clinical relevance:
Baxter’s nerve entrapment: Baxter’s nerve, also known as the inferior calcaneal nerve or the lateral plantar nerve first branch, is entrapped and causes pain on the inside of the ankle and heel that can resemble tarsal tunnel syndrome and plantar fasciitis. After a long period of rest or after getting out of bed in the morning, pain tends to get worse with weight-bearing. The discomfort may at first get better, but as the day goes on, it gets worse.
Assessment
Baxter’s neuropathy:
- Palpating the nerve may reveal radiating discomfort.
- The medial border of the heel, generally around the origin and deep to the abductor hallucis, is the most painful place where the entrapment occurs. This could result in pain that spreads laterally across the plantar foot and radiates or burns.
- The Phalen’s test is affirmative (passively invert and plantarflex the foot). As a result of the porta pedis being smaller, the nerve gets compressed.
- There could be a slight fifth-toe abduction.
- It’s possible that Tinel’s sign is favorable. By tapping on the nerve that runs underneath the abductor hallucis muscle, paresthesias can be induced.
- Patients may experience decreased sensation in the lateral plantar foot in chronic conditions.
Treatment
Conservative treatment contains:
- Overpronation can be controlled with taping or orthotics.
- Soleus and gastrocnemius muscle stretching.
- Soft tissue therapy for the foot intrinsics and plantar fascia.
- NSAIDs, or non-steroidal anti-inflammatory drugs.
- Foot intrinsic strengthening exercises.
- Unconservative therapy
Lateral Plantar Entrapment:
When you bear weight, you may experience lateral foot pain due to lateral plantar nerve entrapment, also referred to as lateral plantar neuropathy.
Pathophysiology: The lateral plantar nerve is entrapped
Clinical Features:
Clinical characteristics include:
- Lateral foot discomfort,
- Numbness,
- Paraesthesias when bearing weight.
- The medial calcaneal tubercle is tender.
Examinations:
- Plain films,
- Ultrasound,
- MRI,
- Diagnostic injection.
Causes:
- Ankle sprain, soft tissue damage, unsuccessful tarsal tunnel release, and tendon harvesting of the flexor hallucis longus are all injuries that can occur. However, medial plantar nerve injury is more likely.
- Neurilemmoma and pseudoganglion are lesions.
- Foot abnormalities include excessive pronation of the foot, laxity of the midtarsal joint, forefoot varus, posterior foot eversion, pes planus, cavovarus foot, and hypertrophy of the abductor hallucis during strenuous activity.[1] Epidemiology
- It is less frequent than Baxter’s nerve (inferior calcaneal nerve) entrapment.
Diagnosis
A: Test of plantar flexion and inversion.
B: Test of dorsiflexion and eversion.
The clinical picture can be difficult since LPN entrapment can happen in conjunction with the entrapment of other local nerves.
History:
The lateral side of the sole and the lateral toes are affected, causing patients to experience scorching pain, paraesthesias, and numbness. Usually, weight-bearing activities make symptoms worse, while rest cures them. However, symptoms may also seen at rest.
Examination:
The abductor hallucis may feel tender to the touch and cause paraesthesias.
The lateral aspect of the foot, which corresponds to the sensory area of the lateral plantar nerve, may have lessened pinprick sensation. Motor impairment is uncommon.
- Tinel’s sign: at the proximal and distal tarsal tunnels, it could be positive.
- The foot is plantar flexed and inverted as pressure is given under the abductor hallucis in the plantar flexion-inversion test.
- Pressure across the proximal tarsal tube during the dorsiflexion-eversion test. The medial plantar nerve, inferior calcaneal nerve, and lateral plantar nerve are all compressed as a result.
Differential Diagnosis:
Differential Diagnosis of Lateral Foot Pain are:
- Tarsal Tunnel Syndrome
- S1 radicular pain
- Plantar Fasciitis
- Fat Pad Atrophy
- Neuroma
- Investigations
- Obtain weight-bearing plain films to assess foot alignment and exclude fractures and osteoarthritis.
Denervation alterations, masses, and tendon anomalies can all be found with MRI.
Studies on the lateral plantar nerve’s nerve conduction may be irregular.
Treatment:
Determine the causes of greater foot pronation, such as obesity, laxity of the midtarsal joint, forefoot varus, back foot eversion, pes planus, cavovarus foot, etc., and address them. Orthotics might be beneficial. Stretching the Achilles tendon and plantar fascia may relieve pressure on the soft tissues. Losing weight and getting physical treatment to make the intrinsic muscles stronger will help to lessen hyperpronation.
Both diagnostic and therapeutic purposes can be served by lateral plantar nerve injection.
Physical therapy:
Physiotherapy treatment helps to increase muscle strength and also helps in relieving pain and pressure on the nerve.
Various treatment includes:
- Ankle movement to increase range of motion
- Exercise of foot
- Proper rest
- Stretching of achilles tendon to increase plantarflexion
- Pain modalities such as ultrasound and tens in nerve course where numbness and tingling sensation present.
- Thermotherapy to reduce swelling and pain in the foot and ankle.
- Isometric exercise of the foot to increase strength.
- Resistance training with various weights and theraband.
- Foot orthosis may support to prevent pronation of the foot
FAQs:
What are the branch’s lateral plantar nerves?
Branches. The lateral proper plantar digital nerve, which supplies the flexor digiti quinti brevis and interossei of the fourth web space, arises from the superficial branch of the lateral plantar nerve.
What are the symptoms of lateral plantar nerve damage?
When the medial and lateral plantar nerves are compressed, it hurts practically constantly, whether one is standing or sitting. It’s often hard to stand still. The discomfort is frequently chronic, challenging to manage, and made worse by high-impact exercises like jogging.
What is the function of the lateral plantar nerve?
The medial plantar nerve supplies the abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and first lumbrical muscles, leaving the lateral plantar nerve to innervate the remaining intrinsic muscles in the sole of the foot.
Can lateral plantar nerve cause foot numbness?
Baxter’s nerve entrapment: The lateral plantar nerve, which is entrapped, extends from the inner ankle side to the little toe down the bottom of your foot.
How do you treat lateral foot pain?
Typically, lateral foot discomfort can be relieved with ice, lots of rest, special foot orthotics, a brace, and certain exercises. Elevation and compression with an elastic bandage can both help reduce edema. Other treatment options, including as surgery, are required in more severe situations.



One Comment