Adolescent Hip Dysplasia [AHD]
Table of Contents
What is Adolescent Hip Dysplasia?
Adolescent Hip Dysplasia (AHD) is a condition where the hip joint is not properly formed or is unstable during the developmental years of adolescence. AHD typically affects girls more than boys and is a common cause of hip pain in young adults.
The exact cause of AHD is not clear, but it is believed to be related to a combination of genetic and environmental factors. Children who are born with a family history of hip dysplasia or who are born breech (feet first) are at an increased risk of developing AHD.
Symptoms of AHD may include pain or stiffness in the hip joint, limping, and difficulty walking or running. In severe cases, AHD can lead to osteoarthritis and hip replacement surgery may be necessary.
Treatment for AHD typically involves the use of braces or other devices to help stabilize the hip joint during development. In some cases, surgery may be required to reposition the hip joint and improve stability. Physical therapy and regular exercise can also be beneficial in managing symptoms and improving hip function.
It is important for parents and caregivers to monitor their child’s hip development during the early years of life and to seek medical attention if they notice any signs of hip dysplasia. Early diagnosis and treatment can help prevent long-term complications and improve outcomes for children with AHD.
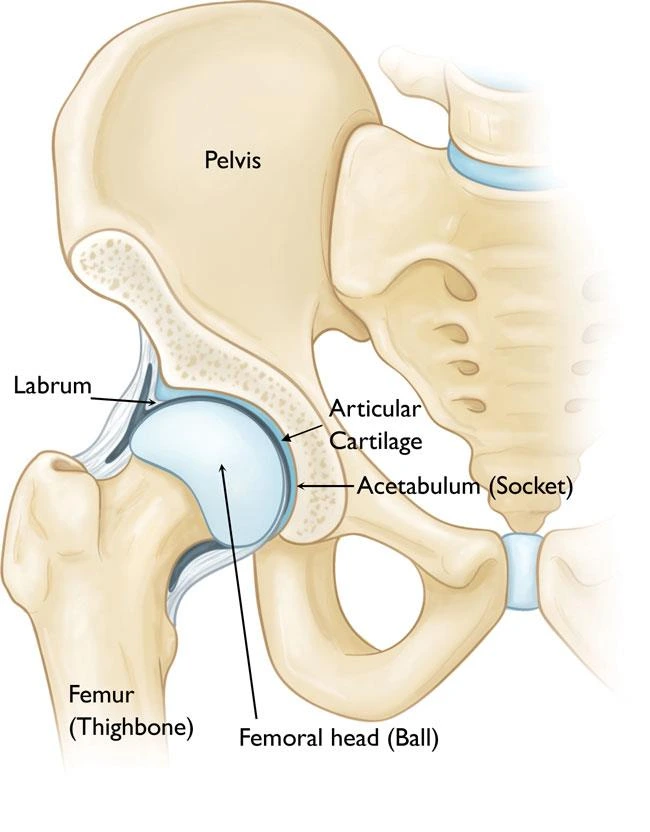
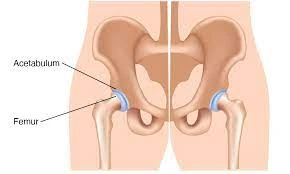
The hip is a “ball-and-socket” type of joint. In a usual hip, the ball is at the upper end of the femur which means the thighbone. It fits firmly into the socket, which is a curved part of the pelvis named the acetabulum. This anomaly can lead to pain in the hip & the early development of osteoarthritis, a disorder in which the articular cartilage in the joint wears away & bone rubs against bone.
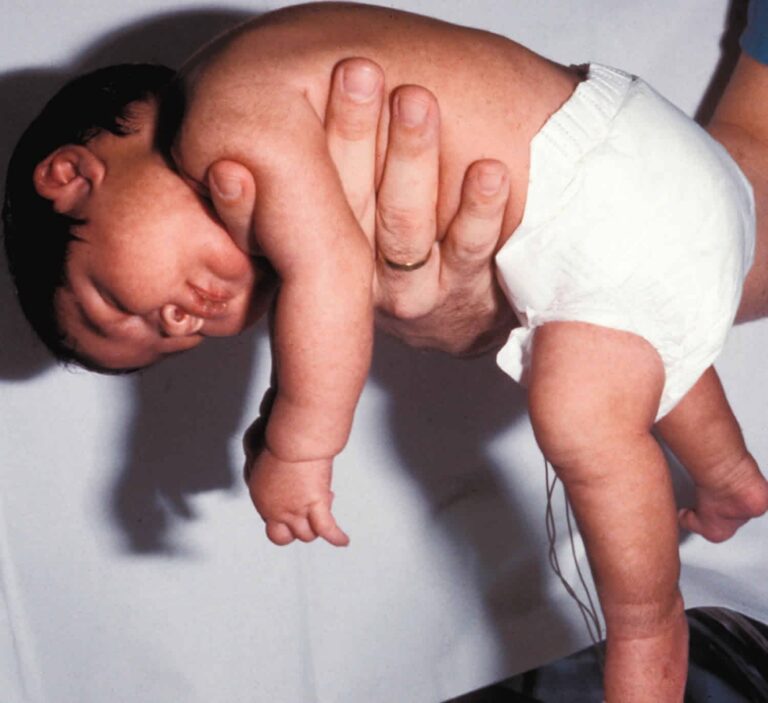
This disease is generally the result of developmental dysplasia of the hip [DDH] & a situation that arises at birth or in the starting stage of preadolescence. Although babies have routinely experimented with DDH, some cases remain hidden or are mild adequately that they are left untreated. These patients may not show signs of hip dysplasia until reaching juvenility.
Treatment for AHD reduces relieving pain while keeping the patient’s natural hip joint for as long as possible. In many patients, this is achieved via surgery to repair the normal anatomy of the joint & delay or control the onset of painful osteoarthritis.
Description
The acetabulum is shallow, suggesting that the ball, femoral head, cannot firmly fit into the socket in hip dysplasia.
As a consequence of this abnormality, the way that force is normally transferred between the bone surfaces is altered. The labrum can take the forces that generally be spread evenly throughout the hip joint. In addition, more force is established on a smaller surface of the hip cartilage & labrum. The smooth articular cartilage evolves frayed & wears out & the labrum evolves torn or damaged. These degenerative differences can progress to premature osteoarthritis.
The severity of hip dysplasia can differ from patient to patient. In mild cases, the head of the femur may only be loose in the socket. In more severe cases, there may be absolute instability in the joint, and the femoral head may be fully dislocated out of the socket.
Causes of Adolescent Hip Dysplasia [AHD]
The exact causes of irregular hip joint development are not invariably known, hip dysplasia is a disorder that most likely stems from an undiagnosed or untreated case of developmental dysplasia of the hip [ DDH ] in childhood. DDH can go unseen during infancy & childhood and may not provoke any symptoms even when severe. Some children have hip dysplasia. When the situation shows up in teens, it was probably present earlier in childhood.
Adolescent hip dysplasia [AHD] generally occurs as a child grows & becomes more active in the early teen years. This can be a result of an instantaneous difference spurt, the requirement for the hip to take more limitation as the child gets bigger, or increased movement.
DDH can happen in families, passed on from one generation to another one. It can be present in either hip or any person. It generally affects the left hip & occurs more often in:
- Girls
- First-born children
- Infants born in the breech position
Symptoms of Adolescent Hip Dysplasia [AHD]
Hip dysplasia in more youthful children is not a painful disorder. Pain affects when the altered forces in the hip lead to degenerative distinctions appearing in the articular cartilage & the labrum.
In most patients, this pain is:
- Discovered in the groin region, although it may occasionally be more toward the externals of the hip.
- Infrequent & mild initially, but may rise in frequency & intensity over time.
- More harmful with movement or near the end of the day.
Some patients may also encounter the feeling of locking, catching, or popping within the groin region. Symptoms differ from mild to severe. They are generally developed & worsen over time.
Diagnosis of hip dysplasia
Physical Examination
During the physical analysis, the doctor will examine the child’s medical history & symptoms. The doctor will move the child’s hip in various directions to evaluate the range of motion [ ROM ] & replicate the pain or pain he or she is feeling
Imaging Studies
In most patients, adolescent hip dysplasia [AHD] can be analyzed with just a physical exam. The doctor may order imaging examinations, however, to lead out other reasons for the child’s pain & to help establish the diagnosis.
X-rays: X-rays deliver images of bone, & will help the doctor evaluate the alignment of the acetabulum & femoral head. An X-ray can also show symptoms of arthritis.
Computerized tomography (CT) scans: More complicated than a plain X-ray, CT scans can help the doctor differentiate the harshness of dysplasia.
Magnetic resonance imaging (MRI) scans: These analyses can create better images of the body’s soft tissues. An MRI can help the doctor find damage to the labrum & articular cartilage.
Treatment of Adolescent Hip Dysplasia [AHD]
Treatment for adolescent hip dysplasia [AHD] concentrates on delaying or controlling the beginning of osteoarthritis while keeping the biological hip joint as considerable as possible.
Treatment counters rely on how serious hip dysplasia is. The care team at Cincinnati Children’s tailor’s treatment to each patient.
Treatment can include:
Nonsurgical Treatment
If the child has mild hip dysplasia and no damage to the labrum & articular cartilage, the doctor recommends nonsurgical therapy. Nonsurgical treatment may also be tested initially for patients who have such comprehensive joint injury that the only surgical option would be a total hip replacement [THR].
Common nonsurgical treatments for adolescent hip dysplasia [AHD] contain:
Observation: If the child has minimal symptoms & mild dysplasia, the doctor may suggest simply observing the condition to make sure it does not get worse. The child will have follow-up visits every 6 – 12 months so that the doctor can check for any progression that may be treated.
Lifestyle modification: The doctor may also suggest that your child avoid movements that lead to pain & discomfort. For a child who is overweight, losing weight will also help to relieve pressure on the hip joint.
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen & naproxen, can help reduce pain & decrease swelling in an arthritic joint. In accumulation, cortisone is an anti-inflammatory agent that can be infiltrated directly into a joint. Although an injection of cortisone can provide pain relief & reduce inflammation, the consequences are temporary.
Physiotherapy Treatment for AHD
Patients require skilled therapy once the hip joint has been fixed through surgery. The initial stage is known as gait training where patients are taught how to use a walker and crutches. After around 6 to 8 weeks the muscles will have reattached & the bone will be recovered. The situation will then require to be treated by a physiotherapist with techniques such as heat, ice, massage therapy, ultrasound, and possibly traction. Light strengthening exercises will be defined to help mobilize the hip & regain its range of motion[ROM]. At this stage, the therapist needs to identify any weak muscles & work on them. A therapist can define exercises that should make the surgery & rehabilitation process more tolerable. Repetitive movements such as cycling & swimming will benefit the hip joint & make things easier afterward. The stronger the joint & surrounding region before the surgery the more comfortable the rehab should be. This is also an ideal time for patients to get accustomed to using a walker or crutches & for the therapist to let them know what precisely they’ll be facing in the weeks after the operation.
The treatment of the condition relies on the age of the patient, but the goal is to make sure the hip joint is in the right position. Some especially young patients may have their hip placed in a cast or harness to hold the hip in its proper place. They will generally undergo surgery when older to keep it there & once again be placed in a cast. After going through the rehab course, a physiotherapist will help strengthen the muscles since they act as a shock absorber for the hip joint. Also, you may be placed on an exercise program to lose weight since there will be less stress put on the hip, which will also result in less pain. Physiotherapy may increase flexibility & strength around the hip joint & can assist lead the body in how to better align itself to decrease stress.
Exercises Adolescent Hip Dysplasia [AHD]
To get the most out of physiotherapy for hip dysplasia, might consider involving the following exercises in the routine:
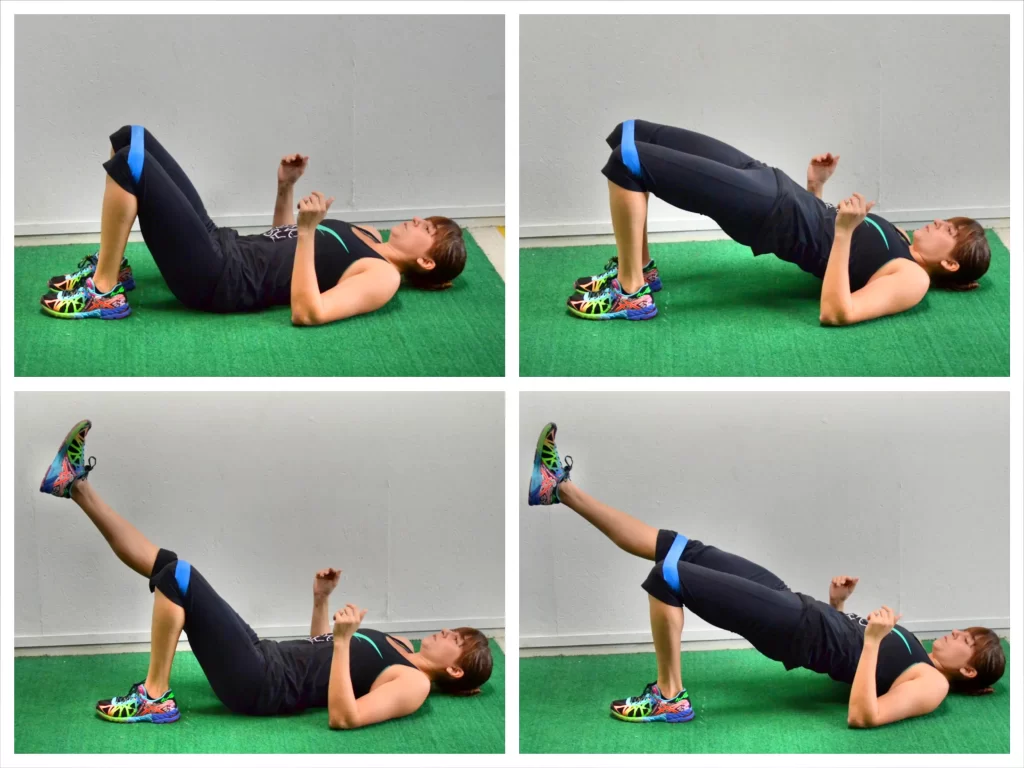
Glute activations
Understanding to isolate & start the gluteus medius permits correcting the over-dominance of the tensor fascia lata muscle that generally becomes hypertrophied over the hip. Experience muscle spasms or psoas disturbance as a result.
To perform this exercise the patient’s position is laying on the back with knees bent and shoulder width apart, and place a band around the upper thighs.
After then put the thumbs on the front of the hips & fingers behind the hip bone [ think back pocket of the pants ], and gently push the knees outwards into the band.
If executed correctly, you should feel the place where your fingers are triggering & not feel motion under the thumbs.
You can also count a bridge to the glute activation by pushing via the heels & raising the pelvis off the floor & towards the roof before slowly lowering back down.
Sliders
To assist in stabilizing the pelvis while walking, sliders work to prepare the gluteus medius to hold the pelvis.
To execute the slides exercise, think about working the static leg, not the sliding leg. The patient’s position is to stand in a mini squat position & bend the elbows onto a surface about chest height [counter, railing, and dresser].
Confirm that wearing socks or place something to slide under the foot [ plastic bag, paper plate, slider ].
Gently slide the foot out to the side & slightly backward without shifting the pelvis or letting the knee rise or fall.
Maintain this exercise for 30 seconds. If done correctly, feel the burn around the back pocket area of the static leg.
Hip abduction
The patient’s position is laying on the side with the bottom leg bent & the top leg straight.
Then, lift the top leg toward the roof & slowly lower it back down.
Repeat this exercise 10-15 times every day.
To be sure you’re accomplishing this correctly, concentrate on keeping the pelvis from rolling backward during the lift.

Banded lateral walk
The patient’s position is a slight squat, and maintain tension in the band & slowly step sideways. Put a mini-band around the ankles.
Do this exercise in 10 steps every day.

Surgical Treatment
It may suggest surgery if the child is in pain & has determined the damage to the articular cartilage in the hip. The surgical technique most generally used to treat hip dysplasia is an osteotomy or “cutting of the bone.” In an osteotomy, the doctor reshapes & reorients the acetabulum and femur so that the 2 joint surfaces are in a more normal situation.
Different types of osteotomies can be performed to treat hip dysplasia. The exact procedure the doctor suggests will rely on several factors, including:
- The child’s age
- The severity of the dysplasia
- The area of damage to the labrum
- Whether osteoarthritis is present
- The number of remaining growing years
Periacetabular osteotomy [ PAO ]: Nowadays, the osteotomy technique most commonly used to treat adolescent hip dysplasia is a periacetabular osteotomy (PAO). “Periacetabular” means “around the acetabulum.”
In most circumstances, PAO accepts from 2-3 hours to perform. During the surgery, it creates 4 cuts in the pelvic bone around the hip joint to facilitate the acetabulum. He or she then turns the acetabulum, transferring it into a more normal position over the femoral head. The doctor will utilize X-rays to direct the bony cuts & to ensure that the acetabulum is repositioned perfectly. Once the bone is transferred, the doctor inserts many small screws to maintain it in place until it heals.
Arthroscopy: In concurrence with PAO, the doctor may use hip arthroscopy to repair a torn labrum. During arthroscopy, the doctor inserts a small camera, named an arthroscope, into the joint. The camera depicts pictures on a television screen, & the physician utilizes these images to show small surgical instruments. Arthroscopic techniques may include:
Labral refixation: In this procedure, the doctor cuts the torn. The frayed tissue around the acetabular rim & reattaches the torn labrum to the bone of the rim.
Debridement: In some circumstances, simply extracting the torn and weakened labral tissue can give pain relief.
Postsurgical Rehabilitation for Hip Dysplasia in Adults
Physiotherapy starts as soon as possible after the technique, usually the very next day.
In circumstances where more intensive rehabilitation is required, or where there is no one at home to help during healing, patients continually go to inpatient rehabilitation centers. The goal of rehabilitation is to strengthen the involved muscles & 3w3 to control excessive scarring & contracture.
Physiotherapy exercises begin with the patient seated & improvement to walking and climbing stairs, first with, & then without, supportive machines. Rehabilitation contains occupational therapy & at-home activities to help patients learn new methods to function effectively in everyday movements. Therapists recommend to patients how to perform ordinary tasks without aggravating their situation by bending to the floor, crossing their legs, or sitting on soft surfaces.
The length of short-term healing, when a patient can walk independently & perform most household tasks, & long-term healing when a patient is fully independent, may differ quite greatly from 6 weeks to 6 months.
Complications
As with any surgical process, there are risks concerned with PAO. The doctor will discuss each of the risks with you & will take precise measures to help avoid potential difficulties.
Although the risks are low, the most common difficulties include:
- Infection
- Blood clots
- Damages to blood vessels & nerves
- Persistent hip pain
- Failure of the osteotomy to recover
Recovery
The child will remain in the hospital for 2 – 4 days after surgery. During this period, he or she will be monitored & given pain medication.
In most cases, full weight-bearing will not be permitted on the operated leg for 6 – 12 weeks while the bones recover in their new position. During this time, your child will require to use crutches.
X-rays will be handled so that the doctor can see how well the PAO has recovered. During your visit, the doctor will decide when it is safe to put weight on the leg & when physiotherapy can begin. The physiotherapist will show your child detailed exercises to help preserve a range of motion [ROM] & restore strength & flexibility in the hip joint.
Long-Term Outlook
For patients experiencing surgery, the long-term consequences of PAO & associated methods are very good. The most common advantage is the relief of pain so people can maintain or increase their hip function. Results can differ depending on age & how severe the disease is, but in general, outcomes are as follows:
10 years after surgery, more than 90% of patients continue to enjoy a successful outcome with the relief of pain.
20 years after surgery, 75% will have continued relief of pain & their situation will not have progressed to arthritis.
Some patients may produce arthritis later in life. Many people may require a hip replacement in the future relying on how developed the dysplasia was at the time of surgery. Hip replacement has enhanced the quality of life, function, & pain.
We watch the general health of the joint with ongoing follow-up appointments. There is no age limitation for continued follow-up, but consideration may be transitioned to an adult facility when applicable for select patients.
FAQ
Hip discomfort in youngsters is most repeatedly generated by a condition named irritable hip, which naturally gets better on its own. But it should always be restricted because it could be a symptom of something serious.
Hip dysplasia can impact anyone at any age. Although it is supposed to develop around birth, a child with mild dysplasia may not have signs for years or even decades.
Surgery for hip dysplasia usually corrects the situation. Many people who accept successful treatment go on to live beneficial lives without hip pain.
Hip dysplasia is usually corrected by surgery. If hip dysplasia goes untreated, arthritis is likely to ripen. Symptomatic hip dysplasia is likely to continue to lead to signs until the deformation is surgically repaired. Many patients profit from a technique called a periacetabular osteotomy or PAO.
If DDH is not treated, the child may create a painless limp when walking, they may walk on their toes rather than in a heel-and-toe action, or they may create a ‘waddling’ walk. In time, arthritis will expand in the untreated hip joint, which will become painful & may ultimately require a hip replacement.