Total Hip Replacement
Table of Contents
Introduction:
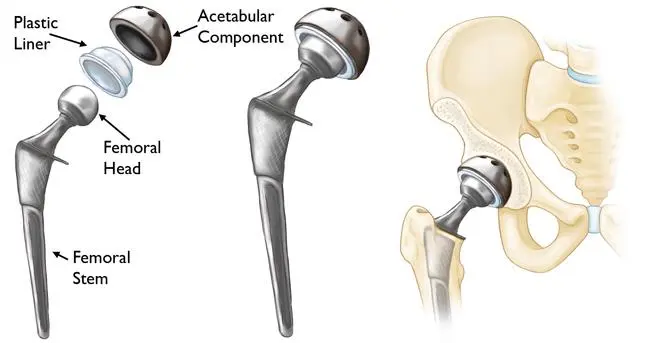
Total hip joint replacement is a surgical procedure in which a damaged or diseased hip joint is replaced with an artificial joint, also known as a prosthesis. The procedure involves removing the damaged parts of the hip joint and replacing them with components made of metal, plastic, or ceramic materials.
Total hip joint replacement is typically recommended for individuals who have severe hip pain and limited mobility due to conditions such as osteoarthritis, rheumatoid arthritis, avascular necrosis, or a hip fracture. It can also be performed in cases of congenital hip deformities or developmental dysplasia of the hip.
Indications of Total Hip replacement:
Total hip joint replacement is typically recommended for individuals who have severe hip pain and limited mobility due to conditions such as:
- Hip Osteoarthritis: This is the most common indication for total hip joint replacement. Osteoarthritis is a degenerative joint disease that causes the cartilage in the hip joint to wear away, resulting in bone-on-bone contact and pain.
- Rheumatoid arthritis: This is a chronic autoimmune disease that causes inflammation of the synovial lining of the joint. In severe cases, it can lead to erosion of the cartilage and bones, resulting in significant pain and disability.
- Avascular necrosis: This is a condition in which the blood supply to the hip joint is disrupted, leading to bone death and collapse of the joint.
- Hip fractures: Fractures of the hip joint can occur due to trauma, such as a fall or a car accident. In some cases, surgery may be required to replace the damaged joint.
- Developmental dysplasia of the hip: This is a condition in which the hip joint doesn’t develop properly, leading to instability and wear and tear of the joint.
- Congenital hip deformities: Certain congenital conditions can cause abnormalities in the hip joint that may require surgical intervention.
It’s important to note that not all cases of hip pain require total hip joint replacement. Your doctor will evaluate your condition and determine if this surgery is the best option for you. Other treatment options, such as medication, physical therapy, or minimally invasive procedures, may be recommended before considering total hip joint replacement.
Contraindications:
Here are some of the common contraindications to total hip joint replacement:
- Infection: An active infection anywhere in the body, including the hip joint, can increase the risk of complications during and after surgery. THJR is typically postponed until the infection is treated and resolved.
- Bone disease: Individuals with severe bone diseases, such as osteoporosis, may not be good candidates for THJR. The implant may not be able to properly anchor into the weakened bone, increasing the risk of implant failure.
- Neurological disorders: Individuals with certain neurological disorders, such as Parkinson’s disease or multiple sclerosis, may have difficulty with postoperative rehabilitation and may not be able to achieve the full benefit of the surgery.
- Cardiovascular disease: Patients with severe cardiovascular disease may be at increased risk for complications during surgery and may not be good candidates for THJR.
- Obesity: Obesity can increase the risk of complications during and after surgery, including infection and implant failure.
- Psychological issues: Individuals with severe mental health disorders, such as schizophrenia, may not be good candidates for THJR due to difficulty with compliance and rehabilitation.
- Allergy: Patients with a known allergy to any of the materials used in the implant may not be good candidates for THJR.
- Poor general health: Individuals with poor general health may not be able to tolerate the stress of surgery and may not be good candidates for THJR.
It’s important to note that the decision to undergo THJR should be made in consultation with an experienced orthopedic surgeon, who can evaluate each patient’s unique medical history and circumstances to determine the most appropriate treatment plan.
Types of Total Hip replacement:
There are several types of total hip joint replacement, including:
- Cemented hip replacement: This type of hip replacement involves using special bone cement to secure the artificial joint components to the remaining bone. A cemented hip replacement is commonly used in older patients or those with weaker bones.
- Uncemented hip replacement: In an uncemented hip replacement, the artificial joint components are designed to attach directly to the bone without the use of cement. This type of hip replacement is often used in younger patients or those with strong bones.
- Hybrid hip replacement: A hybrid hip replacement involves using both cemented and uncemented components in the same surgery. For example, the femoral stem may be uncemented while the acetabular cup is cemented.
- Metal-on-polyethylene: In this type of hip replacement, the ball component of the artificial joint is made of metal, and the socket component is made of polyethylene, a type of plastic. This hip joint replacement is the most commonly used.
- Ceramic-on-polyethylene: Similar to metal-on-polyethylene, the ball component of the artificial joint is made of ceramic, and the socket component is made of polyethylene. Ceramic-on-polyethylene hip replacements may have lower wear rates compared to metal-on-polyethylene hip replacements, but they may also be more brittle and prone to fracture.
- Metal-on-metal: In a metal-on-metal hip replacement, both the ball and socket components are made of metal. This type of hip replacement is less common now due to concerns about metal ions being released into the body and causing adverse reactions.
The choice of which type of hip replacement to use will depend on several factors, including the patient’s age, bone quality, activity level, and any underlying medical conditions. Your orthopedic surgeon will discuss the best type of hip replacement for your individual situation.
Surgical approaches:
There are several surgical approaches that can be used for total hip joint replacement, including:
- Anterior Approach: In this approach, the surgeon makes a small incision at the front of the hip and moves muscles aside to access the hip joint. This approach is becoming increasingly popular due to the potential for less muscle damage, faster recovery, and reduced pain.
- Posterior Approach: This approach involves making an incision at the back of the hip joint and moving muscles aside to access the joint. This is the traditional approach for hip replacement surgery and is still commonly used today.
- Lateral Approach: In this approach, the surgeon makes an incision on the side of the hip and moves muscles aside to access the hip joint. The lateral approach is less commonly used than the anterior or posterior approach.
- Direct Lateral Approach: In this approach, the surgeon makes an incision on the side of the hip and cuts through the muscles to access the hip joint. This approach has fallen out of favour in recent years due to the potential for muscle damage and a longer recovery time.
The choice of surgical approach may depend on a variety of factors, including the surgeon’s preference and experience, the patient’s anatomy, and any pre-existing medical conditions. It’s important to discuss the potential risks and benefits of each approach with your surgeon before undergoing hip replacement surgery.
Medical management:
Medical management for total hip joint replacement involves a variety of strategies to prepare the patient for surgery and manage their recovery afterward. Some of the common medical management strategies include:
- Pain management: pain management is a key aspect of medical management for total hip joint replacement. Pain medications may be prescribed before and after surgery to manage pain and reduce inflammation.
- Blood thinners: Blood thinners may be prescribed to reduce the risk of blood clots after surgery.
- Antibiotics: Antibiotics may be prescribed before and after surgery to reduce the risk of infection.
- Nutritional support: Nutritional support, including supplements or a special diet, may be recommended to optimize the patient’s overall health and support healing after surgery.
- Physical therapy: Physical therapy may be recommended before and after surgery to improve strength and flexibility and to help the patient regain mobility and function after surgery.
- Smoking cessation: Smoking can delay healing and increase the risk of complications after surgery, so smoking cessation may be recommended before surgery.
- Medical clearance: Depending on the patient’s overall health, medical clearance may be required before surgery to ensure that the patient is in the best possible condition for surgery. This may involve consultations with other medical specialists, such as a cardiologist or pulmonologist.
It’s important for patients to work closely with their healthcare team to ensure that they are following all recommended medical management strategies to optimize their outcomes after total hip joint replacement surgery.
Pre-operative Physiotherapy management:
Pre-operative physiotherapy management for total hip joint replacement typically involves a combination of exercise, education, and functional training. The goals of pre-operative physiotherapy are to improve joint range of motion, strength, and endurance, as well as optimise the patient’s overall physical condition to ensure a successful surgical outcome and promote a speedy recovery.
Here are some common pre-operative physiotherapy interventions for total hip joint replacement:
- Strengthening exercises: The patient may be instructed to perform exercises to strengthen the muscles around the hip joint, such as the glutes, quadriceps, and hamstrings. Strengthening exercises may include resistance training, bodyweight exercises, and low-impact aerobic exercises.
- Education: The physiotherapist will educate the patient on the proper use of assistive devices, such as crutches or a walker, and instruct the patient on how to properly transfer and move around in the days leading up to surgery.
- Pain management: The physiotherapist may use modalities such as heat, cold, or electrical stimulation to help manage pain and inflammation.
- Cardiovascular exercise: The physiotherapist may prescribe cardiovascular exercises such as walking, swimming, or cycling to help improve the patient’s overall fitness level and promote circulation.
- Respiratory exercises: The patient may be instructed on deep breathing and coughing exercises to improve lung function and prevent post-operative complications such as pneumonia.
- Pre-operative assessments: The physiotherapist may conduct a pre-operative assessment to evaluate the patient’s physical abilities and identify any potential areas of concern that may impact post-operative recovery.
Overall, pre-operative physiotherapy can help prepare patients for total hip joint replacement surgery, optimize their physical condition, and promote a faster recovery. It is important to follow the physiotherapist’s instructions and complete the prescribed exercises to maximize the benefits of pre-operative physiotherapy.
Post-operative physiotherapy Treatment:
The post-operative physiotherapy management for total hip joint replacement can be divided into different phases based on the patient’s recovery and progress. Here is a breakdown of the phase-wise post-operative physiotherapy management for total hip joint replacement:
Phase 1: Acute phase (day 1 to day 4)
The focus of this phase is pain management and early mobilization.
The physiotherapist will teach the patient breathing exercises, ankle pumps, and gentle range of motion exercises to improve blood flow and prevent blood clots.
The patient will be taught how to get in and out of bed, sit and stand, and walk with the help of an assistive device such as crutch or a walker.
Phase 2: Subacute phase (day 5 to week 2).
The focus of this phase is on increasing the range of motion and strengthening exercises.
The physiotherapist will progress the patient’s exercises to include more challenging ranges of motion and strengthening exercises, such as hip flexion, abduction, adduction, and extension.
The patient will continue to work on walking, balance, and gait training and gradually reduce the use of the assistive device.
Phase 3: Intermediate phase (weeks 3–6)
The focus of this phase is on further strengthening exercises and improving function.
The physiotherapist will introduce more advanced exercises such as squats, lunges, and step-ups to improve hip strength and stability.
The patient will continue to work on walking, balance, and gait training and will progress to walking without an assistive device.
Phase 4: Advanced phase (week 6 onwards)
The focus of this phase is on improving function and returning to normal activities of daily living.
The physiotherapist will work with the patient to achieve goals such as climbing stairs, getting in and out of a car, and returning to work or sports.
The patient will continue to work on strengthening and conditioning exercises to maintain hip joint health and function.
It is important to note that these phases are not set in stone and may vary depending on the patient’s progress and individual needs. The physiotherapist will tailor the treatment plan accordingly to ensure the best possible outcome for the patient.
Total Hip replacement Precautions:
After total hip joint replacement surgery, there are several precautions that patients should take to prevent complications and ensure a successful recovery. Here are some of the common precautions:
- Avoid crossing your legs: Crossing your legs can increase the risk of dislocating the hip joint. It is important to avoid crossing your legs for at least six weeks after surgery.
- Use assistive devices: Assistive devices such as crutches or a walker may be initially required to assist with walking and prevent falls. Patients should use these devices as directed by the physiotherapist.
- Avoid bending your hip beyond 90 degrees; bending the hip too far increases the risk of the joint dislocating. Patients should avoid bending their hip past 90 degrees (e.g., picking something up from the floor) for at least six weeks after surgery.
- Use a raised toilet seat: Patients should use a raised toilet seat to avoid bending the hip past 90 degrees when using the toilet.
- Avoid twisting the hip: twisting the hip can also increase the risk of dislocating the joint. Patients should avoid twisting their hips and instead pivot their entire bodies when turning.
- Avoid high-impact activities: High-impact activities such as running or jumping should be avoided for at least six months after surgery. These activities can put stress on the hip joint and increase the risk of complications.
- Maintain a healthy weight: Excess weight can put stress on the hip joint and increase the risk of complications. Patients should maintain a healthy weight to reduce the stress on the hip joint.
It is important to follow the precautions recommended by your healthcare team to ensure a successful recovery and prevent complications. Your healthcare team will provide specific instructions based on your individual needs and progress.
Conclusion:
Total hip joint replacement is a surgical procedure that can improve the quality of life for individuals with significant hip joint pain and disability. The surgery involves replacing the damaged or diseased hip joint with a prosthetic implant and is typically followed by a period of rehabilitation to help regain strength and mobility. While the procedure is generally safe and effective, it is important to carefully consider the risks and benefits and to work closely with your healthcare provider to determine if a total hip joint replacement is the right option for you.
FAQs:
Which are the 2 types of hip replacement surgery?
Total hip replacement (THR): This procedure involves removing the damaged hip joint and replacing it with an artificial joint made of metal, plastic, or ceramic components. The ball-shaped head of the femur bone is replaced with a metal or ceramic ball, and the socket of the hip joint is replaced with a plastic or metal cup.
Partial hip replacement (PHR): This procedure involves replacing only the damaged portion of the hip joint, rather than the entire joint. It may be performed when only the ball-shaped head of the femur bone is damaged, but the socket of the hip joint is still in good condition. The damaged portion of the femur bone is removed and replaced with a metal or ceramic prosthesis, which is attached to the remaining healthy bone in the hip joint.Which Hip replacement is best?
It’s important to note that there is no one “best” type of hip replacement that is suitable for everyone. The decision to undergo a particular type of hip replacement should be made in consultation with a healthcare provider who can assess the individual’s unique circumstances and recommend the best course of treatment.
What are the advantages of hip replacement?
Hip replacement surgery is a common and effective treatment option for people who have severe hip pain or other conditions that affect the hip joint. Some of the advantages of hip replacement surgery include:
Pain relief: Hip replacement surgery can provide significant relief from chronic hip pain, allowing patients to perform daily activities and improve their overall quality of life.
Improved mobility: The surgery can improve mobility and range of motion in the hip joint, allowing patients to perform activities that were previously difficult or impossible.
Increased strength: By improving mobility and reducing pain, hip replacement surgery can also help patients regain strength in the affected hip and surrounding muscles.
Long-lasting results: With proper care and maintenance, hip replacement implants can last for many years, providing long-lasting relief from hip pain and other symptoms.
Improved overall health: By reducing pain and improving mobility, hip replacement surgery can help patients maintain an active and healthy lifestyle, reducing the risk of other health problems associated with a sedentary lifestyle.
Overall, hip replacement surgery can provide significant benefits for patients who are experiencing chronic hip pain or other conditions that affect the hip joint. It is important to discuss the potential benefits and risks of the surgery with a healthcare provider before making a decision about treatment.What is the best age for hip replacement?
The best age for hip replacement depends on a number of factors, including the severity of the hip condition, the patient’s overall health, and their level of physical activity. In general, there is no one “best” age for hip replacement surgery, as the decision to undergo surgery is based on an individual’s unique circumstances.
Hip replacement surgery is most commonly performed on people between the ages of 50 and 80, but it can be done on younger or older patients as well. Younger patients who have severe hip conditions that impact their daily activities and quality of life may benefit from hip replacement surgery, but they should be aware that the implants used in the procedure have a limited lifespan and may need to be replaced in the future.
Older patients who are in good health and have relatively low levels of physical activity may also be good candidates for hip replacement surgery. However, patients who are frail or have other medical conditions that may increase the risks of surgery may not be good candidates.
Ultimately, the decision to undergo hip replacement surgery should be made in consultation with a healthcare provider who can assess the individual’s unique circumstances and recommend the best course of treatment.Is hip replacement a high-risk surgery?
Hip replacement surgery is generally considered a safe and effective procedure, but as with any surgery, there are risks involved. The overall risk of complications associated with hip replacement surgery is relatively low, but it can vary depending on factors such as the patient’s age, overall health, and the complexity of the procedure.
Some of the potential risks associated with hip replacement surgery include infection, blood clots, nerve or blood vessel damage, dislocation of the new joint, and allergic reactions to anesthesia or implant materials.
However, it’s important to note that the vast majority of people who undergo hip replacement surgery experience significant pain relief and improved mobility, making it a worthwhile option for those with hip pain or other conditions that affect the hip joint. As with any surgery, it’s important to discuss the risks and benefits with your healthcare provider before making a decision about treatment.



2 Comments