Arthritis of Hand: Cause, Symptoms, Treatment & Exercise
Women are more likely to experience osteoarthritis than men, and the most common causes include age, repetitive joint movement, and trauma.
Genetics can also play a factor in the development of osteoarthritis. Arthritis in the hands may also be caused by rheumatoid arthritis or post-traumatic arthritis.
The hand and wrist have multiple small joints that work together to produce motion, including the fine motion needed to thread a needle or tie a shoelace. When the joints are affected by arthritis, activities of daily living can be difficult. Arthritis can occur in many areas of the hand and wrist and can have more than one cause.
Many bones in the body, including those of the wrists and hands, are protected by cartilage. Cartilage can wear down over time. As a result, a person can experience a condition known as osteoarthritis. Another name for this type of arthritis is “wear and tear” arthritis. Women are more likely to experience osteoarthritis than men, and the most common causes include age, repetitive joint movement, and trauma.
Genetics can also play a factor in the development of osteoarthritis. Arthritis in the hands may also be caused by rheumatoid arthritis or post-traumatic arthritis.

Table of Contents
Fast facts on arthritis in hand
Women are more likely than men to experience osteoarthritis.
There is no cure for any type of arthritis in hands.
Treatment focuses on relieving the pain and managing the underlying condition.
In rare instances, a doctor may recommend surgery to repair a severely damaged finger joint.
Types of arthritis affect on Hand:
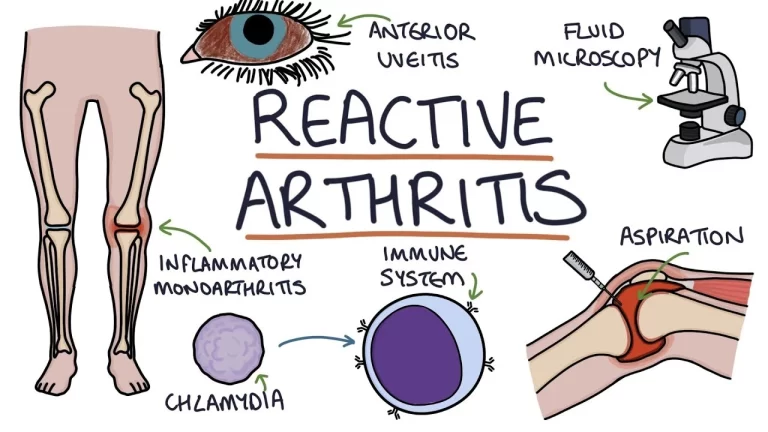
Both osteoarthritis and rheumatoid arthritis (RA) can affect the hands. While osteoarthritis is due to degenerative changes in cartilage, RA is the result of an autoimmune condition.
RA occurs when the body’s immune system attacks healthy tissue that protects the joints. The resulting symptoms can be similar to those of osteoarthritis, including pain, inflammation, and redness.
RA can occur with no risk factors. However, women are more likely to experience the condition than men. Those with a family history of RA, who are obese, or who smoke are also at a greater risk of developing it.
While a person can experience RA at any age, the most common age of onset is between 40 and 60.
A person can also experience post-traumatic arthritis in the hands. This occurs after a person has damaged their hands, such as in a sport-related injury or accident.
Broken or sprained fingers or wrists can also cause post-traumatic arthritis. Injuries can accelerate the breakdown of protective cartilage as well as cause inflammation.
Causes
Though this disease is often related to aging, it may have other causes too. Researchers suggest that arthritis is a combination of heredity and lifestyle factors. It runs in families and can be passed from one generation to another. If your parents or siblings have arthritis, you’re at risk too. Physio, regular exercise, and healthy lifestyle habits can help prevent its onset.
Hand arthritis also tends to occur in obese people. The joints are fragile, so excess weight can wear them down. Trauma, injuries, and joint misalignment only make things worse. Certain health conditions, such as psoriasis, gout, lupus, and infections, may contribute to hand arthritis too.
This condition may result from inflammatory and autoimmune diseases, gene mutations, menopause, and old age. Studies indicate that nearly all women over the age of 70 experience hand arthritis symptoms. The goal of treatment is to slow its progression and reduce complication.
Most types of arthritis cause:
- pain with movement or when at rest
- joint swelling
- joint stiffness
- joint deformity
- weakness and loss of muscle mass
- loss of joint and muscle function
- Symptoms differ slightly depending on the type of arthritis. These differences can help a doctor determine the correct underlying cause of arthritis symptoms in the hands.
Symptoms
Osteoarthritis symptoms
- bony lumps (known as nodes or nodules) at the middle finger joint
- bony lumps or nodes at the finger joint closest to the fingernail
- pain that occurs deep under the base of the thumb
- stiffness, especially in the morning
- difficulty pinching and gripping items
Rheumatoid arthritis symptoms
- pain at the wrist and finger knuckles
- deformities of the wrist and fingers where they will not straighten
- tendon ruptures, which affect the ability of the fingers to straighten
- unexplained fatigue
- flu-like achiness throughout the body
- Post-traumatic arthritis symptoms
- pain, primarily where the former injury occurred
- worsening deformity following an injury
- Many of the post-traumatic arthritis symptoms are similar to those of RA and osteoarthritis. However, with post-traumatic arthritis, a person can usually attribute their symptoms to a previous injury.
How to Diagnosis Arthritis of Hands?

It happens every day, all over the country. People with joint problems make appointments with their doctors, wanting a quick answer. They want to know what’s wrong and how it can be fixed. The signs and symptoms that lead people to the exam room are typically joint pain, swelling or stiffness. Sometimes unexplained fatigue and a lingering sense of illness are problems, too.
Primary care providers are usually the first stop for joint problems. Someone who’s been searching for answers for a while may see to a rheumatologist, a doctor who specializes in diagnosing and treating arthritis and rheumatic conditions, or an orthopaedic specialist, or joint surgeon. All of them are going to approach joint problems in a similar fashion, but with differences in depth and breadth of examination and testing.
A generalist will likely do a top-level exam and some basic tests looking for some of the more common types of arthritis. A rheumatologist will do a comprehensive and thorough assessment; an orthopedics will evaluate the physical, or mechanical, cause of joint pain and determine the potential for a surgical solution.
Here is an overview of the ways in which health care providers, on their own or as part of a team, evaluate joint problems and diagnose or eliminate arthritis.
Medical & Family History
The evaluation should start with questions and answers.
Symptoms. When did they start?; what’s the level of pain?; when does the stiffness occur, is it after activity or rest?; and how long does it last?; do symptoms come and go, or have they stayed the same over time?; and what, if anything, relieves the pain?
Current, Recent and Past Health. Have you been sick recently?; have you traveled out of the country, to the Rocky Mountains, New Mexico or spent time in wooded areas, particularly in the Northeast?; do you have an autoimmune condition?; have you injured the joint or joints recently or long ago?; do you play contact sports or ones that require quick turns and pivots (like soccer or basketball)?; do you work in a job that requires long hours of standing or sitting, frequent kneeling or repetitive motion?; do you have other chronic diseases, such as high blood pressure or diabetes?; and what medications – both over-the-counter and prescription – and supplements, herbs and vitamins are you taking?
Health Habits. Do you smoke?; are you at a healthy weight?; do you exercise regularly?; what do you do and how often?; do you eat healthful foods or too much processed, fatty or sugary foods?; do you get enough sleep?; do you have lots of stress?; and do you have any mental health issues, like depression or anxiety?
Family History. Does anyone in the family – parents, siblings, grandparents or even aunts or uncles have any type of arthritis or rheumatic disease; and how about an autoimmune condition?
Physical Exam
A joint evaluation is hands-on work. Doctors look to see which joints have visible signs of joint swelling, stiffness or redness. The exam is detailed. Knowing the fingers are affected is a little helpful, but seeing which finger joints — the knuckles, middle joints or tip joints – is very helpful. If more than one joint is involved, there will be a joint count, and check for whether the pattern is symmetrical, that is, whether the same joint is affected on both sides of the body (for example, both wrists). The doctor will feel the joint for warmth, swelling and fluid. The doctor will move the joints back and forth to see range of motion, and will and gently prod to see if there are tender areas near or far from the joint. Then there are the usual exam steps — a temperature reading, a check for swollen glands, a look into the eyes and down the throat, as well as a reflex check, too.
Imaging Tests
Depending on the findings so far, your doctor may order lab and/or imaging tests.
Lab Tests. Blood may be drawn to check for levels of inflammation, presence of antibodies, and status of general systems (complete blood count, liver and kidney function, etc.). The doctor may use a needle to draw fluid from the joint for analysis. In some cases, a genetic test may be ordered.
Imaging Tests. X-rays are the most frequently used means of visualizing the joint, but sometimes ultrasound and MRI are used. The image will be read for structural changes in the joint, signs of joint erosions, cartilage loss, soft tissue tears, inflammation, location and amount of fluid, and presence of loose tissue fragments.
Making an arthritis diagnosis can sometimes be relatively straightforward — but not always. The diagnostic process includes eliminating problems other than arthritis. But if the problem seems to be arthritis, then which type of arthritis is it? There are more than 100 types of arthritis and related conditions. Osteoarthritis is by far the most common type, and is often the first consideration, but many other types are relatively rare. Symptoms may come and go over time. And some types of arthritis don’t reveal their full range of effects at once. Sometimes a key feature that would confirm a diagnosis doesn’t show up for years. Oddly enough, one type of arthritis can be mistaken for another, and people may have more than one type.
Even if the specific diagnosis isn’t clear, but signs point to an inflammatory type of arthritis, doctors may go ahead and start treatment to bring down high levels of inflammation. Taking corticosteroids or disease-modifying anti-rheumatic drugs can help avoid the permanent joint damage that can occur in active, uncontrolled disease. Waiting to treat inflammatory arthritis is highly risky. That’s why rheumatologists say early diagnosis and aggressive treatment are the keys to preventing visible joint changes, chronic pain, loss of mobility and decreased function.
Whether or not treatment has begun, your doctor will likely advise at-home measures, such as heat and cold to soothe pain, resting the joint regularly and protecting it from strain and overuse.
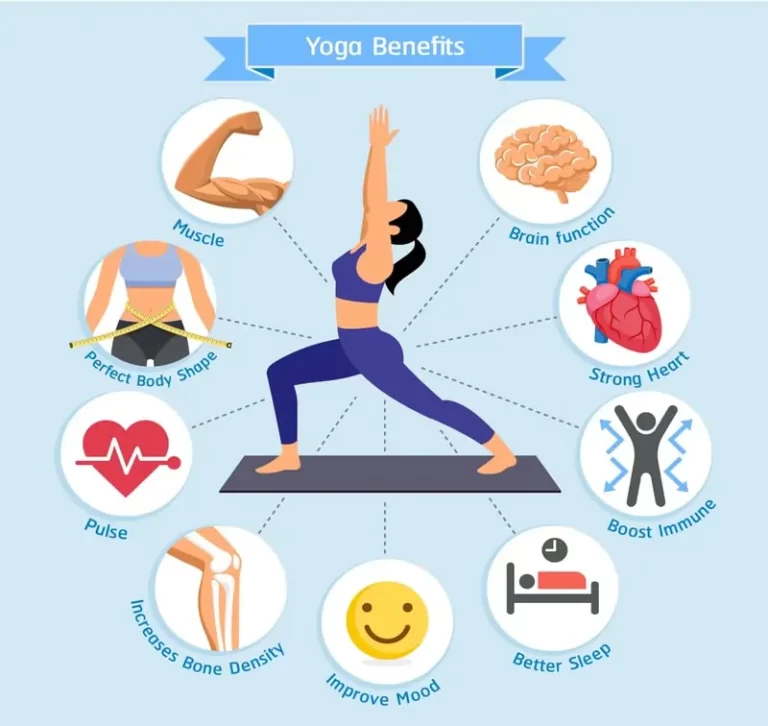
Physiotherapy treatment
Physiotherapy has emerged as one of the safest, most efficient ways to treat rheumatoid arthritis. Rehabilitation techniques include massage, hydrotherapy, electrical stimulation, cold and heat therapy, and preventive measures.
Cold and heat applications, for instance, provide temporary pain relief. Electro-stimulation helps reduce swelling and improves range of motion. Hydrotherapy activates the parasympathetic nervous system and alleviates pain. The physiotherapist may also recommend assistive devices, manual massage, and hand exercises that strengthen the muscles and joints.
Physiotherapy treatment & exercise can help improve your strength, flexibility, and dexterity. After a few sessions, you’ll find it easier to work and use your hands. Your joints will become less stiff and the pain will diminish. This treatment method can also reduce fatigue and depression, which are common side effects of arthritis.
Talk with your physiotherapist about compression gloves, splinting, and adaptive equipment. He can prescribe the most suitable products and help you prevent complications. A good physiotherapist will also recommend coordination and balance exercises that improve daily functioning.
Discuss your options in order to make an informed decision. Physiotherapy can make a world of difference, so ask for advice and stick to your treatment.
Hand exercises
Exercises can help to keep the supportive ligaments and tendons in the hands flexible and may also help reduce pain in the hands.
To help alleviate arthritic pain in the hands, a person can try:
Making a loose fist and opening the fingers to fully straighten them, repeating this several times on each hand.
Bending a finger slowly and carefully, then slowly straightening it out again, and repeating with all fingers.
Placing the hand on a flat surface with fingers extended and slowly lifting each finger off the surface.
Hold the finger at the highest point it can reach for 3 to 5 seconds. Repeat with each finger.
It is best to do these exercises using gentle motions.
Physiotherapists who specialize in hands may be able to recommend exercises as well.
Resting the hands from activities that cause pain and overuse can also help to reduce pain.
Hot and cold therapy
Applying ice to swollen joints for 10 minutes at a time can help reduce swelling. The ice should always have a protective covering, such as a cloth, to prevent skin damage.
Heat therapy can sometimes help to ease stiff joints. Placing the hands in a tub of warm water can help.
Some products for hot and cold therapy are available for purchase online, including cool packs and heat pads.
Paraffin wax treatments have also been proven to be soothing and help ease stiffness and pain. Wax treatments should only be done under the supervision of a physical therapist.
Splinting
Splinting can involve wearing a protective brace on the hand, which may resemble a fingerless glove.
There are also “sleeve” brace options that will fit a single finger or multiple fingers, depending on the source of arthritis pain.
By holding the joint still, these braces ideally reduce the incidence of pain.