Thoracic spine mobilization technique
Table of Contents
What is Mobilization for the Thoracic spine?
- Thoracic spine mobilization is a passive, skilled, manual therapy maneuver applied to joints and related to the soft tissue at various speeds and amplitudes taking physiological or accessory movement for therapeutic purposes
- small volume oscillation applies at a fast velocity, and a large volume force applies at to slow velocity
- it is a hand-operated method that consists of applying the target forces on a painful, stiff, or otherwise neglected joint in addition to elevating its overall function. Which is inappropriate in all conditions, joint mobilizations/manipulation help improve the range of motion, reduce pain, and reduce stiffness.
- Thoracic spine mobilization is a manual therapist’s hand treatment that is repeatedly executed by physical therapists and healthcare professionals who master rehabilitation for locomotion huddles and chiropractors, health professionals treating huddles of the musculoskeletal system that subsists bones, muscles, soft tissue, and ligaments, etc.
Introduction to the Thoracic Spine
- A healthy spine has three natural curves that initiate an S-shape in which the thoracic spine middle creates a convex shape. This spinal curvature soaks up shocks to your body and protects your spine from injury. Many different parts create the spine:
- Vertebrae: The thoracic spine has 33 irregular vertebrae small bones that hammer the spinal canal. The spinal canal is a cave that houses the spinal cord and nerves, defending them from injury. Most of the vertebrae locomote to grant a range of motion.
- Facet joints: These spinal facet joints have cartilage a greasy connective tissue that permits the vertebrae to slide in opposition to each other. Facet joints permit you to twist and turn, giving flexibility and stability. facet joints may develop arthritis and cause back pain or neck pain.
- Intervertebral disc: These flat, round cushions lie in the middle of the vertebrae and act as the spine’s shock absorbers. Each intervertebral disk has a soft, gel-like center the nucleus pulposus confined by a flexible outer ring the annulus fibrosus. Intervertebral discs are under constant pressure. A herniated disk can crack, and tear, permitting some of the nucleus’s gel substance to expose. Herniated disks also called bulging, slipped, or/and ruptured disks can be terrible.
- Spinal cord and nerves: The spinal cord is a column of nerves that passes along with the spinal canal. The line of nerve extends from the skull to the lower back. 31 pairs of nerves branch out across the vertebral beginning in the neural foramen. These nerves take out messages in the middle part of the brain and muscles.
- Soft tissues: Ligaments affix to the vertebrae to hold the spine in an upright position. Muscles support the back and help you to move on the front side and/or backside. Tendons affix to the muscles to bones and aid movement.
What are the spine segments?
- The 33 vertebrae subsist of five specific spine segments. Starting at the neck and/or going down toward the buttock’s rear end, these segments subsist
- cervical spine
- thoracic spine
- lumbar spine
- sacrum
- coccyx
Thoracic Spine
- Thoracic spine (middle back): The chest or thoracic part of the spine has 12 vertebrae from T1 to T12. Your ribs attach to the thoracic spine. The thoracic spine turns out gently to make a backward C-shape called the kyphotic curve.
ligaments of the thoracic spine
costotransverse ligament
- The costotransverse ligament is a fibrous band in the middle part of the transverse process and the neck of the rib, it’s separated into two parts: the superior and the lateral costotransverse ligaments.
- there are three types of costotransverse ligaments in the human body: costotransverse ligament affixes the posterior surface of the neck of the rib with the transverse process of the analogous vertebrae. a lateral costotransverse ligament affixed with the non-articular part of the rib with the tip of the transverse process and a superior costotransverse ligament affixes the upper border of the rib of the neck of the inferior border of the transverse process of the vertebrae beyond. In inclusion, the inferior costotransverse ligament and the posterior costotransverse ligament are in the costotransverse grouping.
Functions
- Support and/or inhibit displaced ribs and restrict the costotransverse joint to perform a gliding movement.
- The costotransverse ligament posterior surfaces give attachment points for the extensor muscles of the deep group of the back.
Anterior atlanto axial ligament
- The anterior atlantoaxial ligament is a strong membrane, fixed, beyond, the lower border of the anterior arch of the atlas; beneath the front of the body of the axis.
- It is strengthened in the middle line via a rounded cord, which affixes the tubercle on the anterior arch of the atlas to the body of the axis, and is an extension of the upward of the Anterior longitudinal ligament.
- The ligament is in contact, in front, with the longus capitis.
Anterior longitudinal ligament
- A strong strap like a band of variable thickness and/or width glazes the anterior side of the vertebral bodies and intervertebral discs the whole length of the vertebral column. in distinction to superficial to deep its ligamentous fibers run differing lengths:
- the deepest fibers are little intersegmental fibers
- the intermediate fibers join 2 to 3 vertebrae
- the superficial fibers join 3 to a vertebrae
- It is thick, yet narrow, among the vertebral bodies where it is loosely joined to the periosteum. At the levels of the intervertebral disc, ligaments broaden and the fibers strongly affix to the fibrocartilage disc the hyaline cartilage in vertebral end plates, and the margin of the vertebra
- A primary spine stabilizer surrounds one inch broad, and the Anterior longitudinal ligament travels the all-over length of the spine in distinction to the base of the skull, via the cervical, thoracic, and lumbar all the 3 spines to the sacrum. It joins the front side anterior of the vertebral body with the front of the annulus fibrosis.
- posterior longitudinal ligament affixed to the upper and lower margins of the particular vertebral body.
- decelerate the extension of the vertebral column and point out the intervertebral disc.
- the edge on the anterior surface of the vertebral bodies is the vertebral column.
animation
- The anterior longitudinal ligament is animated by recurrent branches of rami communicantes.
posterior longitudinal ligament
- The posterior longitudinal ligament is one of the most important ligaments that distribute stability in the spine. It ravines along with the posterior aspect of the vertebral body inner side of the vertebral canal from the body of the axis to the sacrum. The posterior ligament is a sequence of longitudinal fibers that are opaquer than the anterior longitudinal ligament. However, like the anterior longitudinal ligament, the blurred fibers are deeper and affix to one vertebra while the superficial fibers attach to three to four vertebrae. The superficial layer is a continuation of the tectorial membrane at the axis of the posterior longitudinal ligament, and the deep layer is an origination of the cruciform ligament at the Atlas.
- The fibers are wide at the intervertebral spaces and are more adherent to the annulus fibrosus of the intervertebral discs rather than at the vertebral body where fibers are thinner. This peculiarity is more showable in the posterior ligament rather than in the anterior. Therefore, the posterior longitudinal ligament is much more dignified rather than the anterior longitudinal ligament, which is constraining for the disc herniation appearing posterolateral.
- The Posterior longitudinal ligament includes superficial and deep connective tissue layers, The superficial layer is the more dorsal side, with its continuation from the dura mater often being difficult to identify. the superficial layer consists of a central band of fibers 8 to 10 mm broad expanding beyond a lot of vertebral segments. Due to its major joining with the intervertebral disc, it has been termed as being ‘‘feeble’’, granting a craggy appearance over every vertebral body. This craggy appearance turns more probable in the lower thoracic and lumbar areas, where the superficial layer is of more decent width.
- connotation variation even within the lumbar area, where both the central fibers and the ‘‘fan-like’’ part favor deceleration in width in the center of L1 and L5 vertebrae. The deep layer, which is adherent to the superficial layer in the midline, is of more decent diameter whole its length, being 2 to 3 mm wide at its precarious point. It also has a craggy appearance.
- In the cervical area, the Posterior longitudinal ligament is a broad band-like structure of equal width beyond both the intervertebral disc and vertebral body, however more inferiorly, it made increasingly craggy, with its fastest part being beyond the intervertebral disc The division fibers of the superficial and deep layers were difficult to identify at the level of the intervertebral disc, but the intervertebral disc affixation to the edges of the vertebral bodies and intervening annulus fibrosus was clear.
- The fibers of each and every layer came to reinforce, hammering standard affixation. Both the superficial and deep layers are affixed to a midline of the bony septum on the posterior surface of the vertebral body in the middle of the superior and inferior boundary. The connection was only sometimes propagated because of insufficiency in the septum in the central 3rd of the vertebral body. The adaptation of fibers within the posterior longitudinal ligament was perpetual at all levels, with the fiber in the central portion of the superficial layer being more vertical than those of the ‘‘fan-like’’ part. even if the deep layer was examinable through the superficial layer
- The posterior longitudinal ligament has a more antagonistic than supportive role. The examination pattern of movement of antagonistic materials like masses and bony fragments following a vertebral fracture into the vertebral canal suggest that the Posterior longitudinal ligament acts as a defender for the spinal cord and from displaced disc material.
- Fibers of the superficial layer will restrict the forward flexion, while the oblique fibers of the deep layer will restrict the lateral flexion and rotation. fibers from both layers subsist in all movements, with the raising number of fibers enrolled with elevating pressure. The craggy appearance of the Posterior longitudinal ligament in the lower thoracic and lumbar area may be due to the raised rotational and lateral flexion forces bore out in the lower area correlated to the upper area of the vertebral column of the spine. The presence of elastin protein in the Posterior longitudinal ligament aid that it has a role in the many movements of the spine. examined patterns of disc fragment migration following vertebral burst fractures indicate that the Posterior longitudinal ligament also preserves the contents of the vertebral canal.
blood supply
- The major supply of blood to the spinal cord is in distinction to a single anterior spinal artery and the two posterior spinal arteries. Two posterior spinal arteries are the branches of the vertebral artery in the spine. Posterior arteries send the blood to the posterior part of the spinal cord, and the anterior segment obtains blood supply from the anterior spinal artery. contiguous to the spinal arteries, there are other arteries also available at each spinal segment termed radicular spinal arteries, which arrive from the body wall arteries. The small penetrating arteries radiate off via both anterior and posterior spinal arteries that hammers interrelate in the spinal cord.
- The radicular spinal arteries convey the blood to the ventral and dorsal parts of the spinal cord. The sewerage of blood from the spinal cord snatches the place with the aid of anterior and posterior spinal veins. The anterior and posterior spinal veins conduit into the internal and external venous plexus. Through the venous plexus, the blood conduit into the main venous system with the help of azygos veins, lumbar veins, and hemizygous veins
nerve supply
- The primary source of the nerve supply of the posterior longitudinal ligament is the meningeal branch hired from the spinal nerve. It consensus ascending and descending branches in the vertebral column of the spine. There are transverse roots hammered by the fusion of ascending and descending nerve roots. The amalgam of the transverse branches from the reverse side generates a connection of nerve fibers superficially, which animates the posterior longitudinal ligament in the vertebral segment of the spine. The posterior part of the annulus fibrosus is desperate by the nerve fibers hammering a network deeply in the intervertebral part of the posterior longitudinal ligament
- There is no nerve supply of the deep layer of the nucleus pulposus or/and annulus fibrosus due to the shortcoming nerve fibers and nerve boundary. some nerve boundaries are available in the middle part of the nucleus pulposus, but in the peripheral zone, there are bulky nerve fibers. The heavy nerve fibers in the peripheral segment perform an essential part in the regulation of movement and posture in the vertebral column of the spine.
muscle of the posterior longitudinal ligament
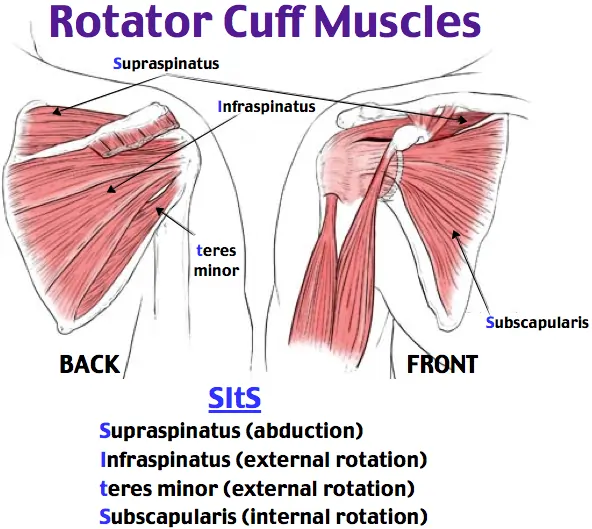
- There are 3 groups of muscle in the posterior of the spine; superficial, intermediate, and deep muscle layers. The superficial layer subsists of two muscles the splenius cervicis and splenius capitis. muscles perform the needed part in the extension of the neck and the movement of the shoulder.
- The intermediate muscle group subsists of the longissimus, iliocostalis, and/or spinalis muscles. longissimus, iliocostalis, and spinalis muscles of the intermediate group have parallel tendinous arises. The intermediate groups of muscles aid in the flexion of the head and the upper vertebral column and the movement of the thoracic cage. The deep layer subsists of the semispinalis, rotatores, and multifidus. The major function superficial intermediate and deep muscle group is the stabilize the vertebral column and manage an upright posture. The intermediate group of muscle also assist in balance and proprioception
variants of the posterior longitudinal ligament
- the posterior longitudinal ligament is smaller and sluggish. It has an egg shape that varies from 2 to 2.25 mm in thickness at the level of L5-S1. From the L5 vertebrae upwards, the ligament hammers a slim band, which widens parallelly at the level of each disc. The fibers of the annulus fibrosus and the boundary of the vertebral body are the sites of association of the ligament, but in some cases, not all, it is associated with the posterior aspect of the vertebra.
- The posterior longitudinal ligament bear to be most developed at the level of the L3 and L4 vertebrae, where its average thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker mid-segment almost about 2.5 to 4 mm thickness all over the whole length of the ligament. The posterior longitudinal ligament in the mid-segment of every vertebral body envelops the vascular foramina
interspinous ligament
- This ligament is settled of thin sheets affixing the spinous processes from roots to apexes from C1 to S1 vertebrae one segment at a time. Anteriorly, Its fibers affix with ligamentum flavum, in conjunction with posteriorly its fibers affix with the supraspinous ligament. The ligaments are small and/or lengthen in the thoracic area, broader, thicker, quadrilateral in hammers in the lumbar area, and only slightly clear in the neck. In the neck, the interspinous ligament is normally contemplated as part of the nuchal ligament.
- The interspinous ligaments are thin and short structures that affix adherent spinous processes. The Interspinous ligament is well vascularized and subsists of sensory nerves, especially on their posterior and lateral surfaces. These ligaments arise partially from the ligament Flava, partially from the reciprocal vertebral laminae, and partially from the caudal aspect of the spinous process. The lumbar Interspinous ligament is somewhat thicker and bears to be more sparkler and quadrilateral in nature and in general, happens in pairs. The lumbar Interspinous ligament is usually blocked out with a fiber direction passing obliquely or/and horizontally in an anterior-posterior direction from the superior margin of the caudal spinous process to the cranial spinous process.
- The Interspinous ligament is part of the posterior ligamental complex, and the ligament acts as a stabilizer of the thoracic spine and assists to limit spine flexion.
nerve supply
- The lumbar interspinous ligaments obtain a nerve supply from the medial branches of the lumbar dorsal rami and experimental stimulation of the interspinous ligament gives low back pain and referred pain in the lower limbs. nerve donates the interspinous ligament as an alluring source of low back aches.
blood supply
- The interspinous ligament is well supplied by small blood vessels and/or sensory nerves, then after, especially in its posterior part and/or on its lateral surfaces.
- movements The role of the interspinous ligament is to restrict flexion bending forwards by restricting the division of the spinous processes of the vertebral column.
intertrasverse ligament
- the intertransverse ligaments are ligaments that are confined in the middle of the transverse processes of the spine.
- In the cervical area, the intertransverse ligament subsists of a few irregular, scattered fibers that are often reachieved by muscles. In the thoracic area, the intertransverse ligament is rounded cords intimate affix to the deep muscles of the back. In the lumbar area, the intertransverse ligament is thin and bleary.
- The intertransverse ligaments in general blend with the intertransverse muscles.
- The function of the intertransverse ligaments is to prohibit lateral flexion of the spine.
- The posterior longitudinal ligament bear to be most developed at the level of the L3 and L4 vertebrae, where its average thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker mid-segment almost about 2.5 to 4 mm thickness all over the whole length of the ligament. The ligament in the central portion of every vertebral body shield the vascular foramina
Nuchal ligament
- the nuchal ligament is positioned on the back of the neck elongation with the Supraspinous ligament. It hammers a 2 layered fibroelastic septum that removed the dorsal muscles of the neck and runs from the spine of the C7 vertebra to the occiput bone.
attachments
- continuous from the external occipital protuberance on the skull and/or median nuchal line to the spinous process of C7 vertebrae. The deep fibers of the ligament affix to the external occipital crest, the posterior tubercle of the atlas, and the medial surface of the bifid processes of the other cervical vertebrae.
Function
- Limits flexion
- provides affixation in the middle of the Trapezius and Splenius capitis.
ligamentum flavum
- The ligamentum flavum is a short but thick ligament that affixes the laminae of adjoining vertebrae from C2 to S1 and/or is designated a medical word elongation of a facet joint. It involves 80% elastin fibers and 20% collagen fibers. The high percentage of elastin protein fibers gives to the ligament with its yellow color and flexible nature.
- in spite of the elastic and flexible essence of the ligament, at the neutral position, the ligament has a hypocrisy inhibiting it from buckling. At the lumbar vertebra, the neutral position is given by the traction and tension forces put by muscles on the Thoracolumbar fascia by the supraspinous, interspinous ligaments to ligamentum flavum create hypocrisy in the neutral position of the theinterspinous_supraspinous thoracolumbar ligamentous complex
- At any intersegmental level, the ligamentum flavum is a combined structure represented symmetrically on both sides.
- In the neck side part, the ligaments are thin but broad and long; ligaments are broader in the thoracic segment and broadest in the lumbar area.
Attachments
- The ligament flavum starts from the lower half of the anterior surface of the lamina apart from and affixed to the posterior surface and upper edge of the lamina beneath, hammering a cup-like shape clasp on the upper border of the lamina beneath.
- On either side the ligament is the division into two portions:
- The medial portion: ravine to the back of the next lower lamina and astride the gap between the neighboring vertebrae fusing with the interspinous ligament
- The lateral portion: ravine in front of the facet joint where it affixes to the anterior aspect of the inferior and superior articular processes and hammers the anterior capsule. Most lateral fibers extend apart from the superior articular process to the pedicle beneath.
Function
- The point-out elasticity gives conserves the upright posture and assists the vertebral column in reopening its shape after flexion. It inhibits excessive separation of the relative vertebral lamina and inhibits buckling of the ligament into the spinal canal during extension, inhibiting canal compression. The lateral part of the ligament inhibits the anterior capsule of the facet joint from being hideout within the joint cavity during movement.
supraspinous ligament
- The supraspinous ligament or/and the supraspinal ligament is a strong fibrous cord that affixes in conjunction with the apices of the spinous processes from the 7th cervical vertebra to the 3rd or 4th lumbar vertebrae. From the C7 vertebra to the skull ligament convert into structurally specific from more back parts of the ligament and is called the ligamentum nuchae
- Origin: It originates from the C7 vertebra.
- Insertion/Terminates: Sacrum
- The supraspinous ligament is fully grown up only in the upper lumbar segment and may terminate at L3 vertebrae, in spite of the most common termination site tending to be at L4 vertebrae. The supraspinous ligament is always not present at L5 and S1 vertebrae.
- It is thicker and broader in the lumbar segment rather than in the thoracic segment, it associates with the thoracolumbar fascia.
- The most superficial fibers of the supraspinous ligament enlarge beyond 3 or/and 4 vertebræ; those more deeply seated ligaments pass away in the mid part of 2 or /and 3 vertebræ while the deepest ligaments affix the spinous processes of relative vertebrae
- The deep layer of the supraspinous ligament is authorized by tendinous fibers of the multifidus muscle. in the middle of the spinous processes, it is elongated with the interspinal ligaments. The supraspinous ligament’s mid fibers affix with the thoracolumbar fascia’s dorsal layer.
Function
- restricts flexion onward with other ligaments of the vertebral column.
- The supraspinous ligament contributes as a part of the midline affix for some important muscles.
- The supraspinous ligament aids in conducting the upright position of the head.
- supraspinous ligament stretched in flexion, its fibers restrict the division of spinous processes during forward flexion, while hyperflexion, the interspinous ligament, and supraspinous ligament are the first to fall.
- At the lumbar area, through the affixation of the supraspinous ligament to the thoracolumbar fascia and interspinous ligament, the ligaments hammer in conjunction with the Interspinous_supraspinous thoracolumbar ligamentous complex which it`s function is to move tension that is positioned on Thoracolumbar fascia to ligamentum flavum causing conceit in the neutral position
Muscle of the thoracic spine
- Superficial muscles and back muscles are created just beneath the skin. consists of the latissimus dorsi, the trapezius, the levator scapulae, and the rhomboids. capability to move the upper limb as they awake at the vertebral column and insert onto either the clavicle, scapula or/and humerus.
- Intermediate back muscles – task to elevate and depress the rib cage of the spine. There are two major muscles that elevate and depress the spine. the serratus posterior superior and/or the serratus posterior inferior muscle.
- Back muscles – Include Erector Spinae and Transversospinalis Group intrinsic back muscles. These muscles in general work to benefit the movements of the vertebral column of the spine and to also control posture.
Major Muscles of the thoracic spine
Superficial Layer
- Trapezius large back muscle affixed to the vertebral column from the base of the skull to the ligamentum nuchae of the neck, again affixing to the spinous processes of the C7 vertebrae and the thoracic spine downwards to the T12 vertebrae. It affixed the shoulder blade to the vertebral column and acts to help the arm and assist in upper limb movement by controlling shoulder blade movements.
- Latissimus Dorsi is the broad back muscle that travels from the spinous processes of the lower thoracic vertebrae and the lumbar spine, the connective tissue fascia of the thoracolumbar area, along with the pelvis and lower ribs, to embed into the upper arm bone called the humerus. humerus’s first action is to expand, adduct, and internally rotate the upper arm bear the upper arm backward, to the side of the body, and rotate the upper arm towards the body performing a chin-up. humerus also consequences the movements of the shoulder blade and trunk.
- Rhomboids muscle rhombus-shaped muscles start from the spinous processes of cervical and thoracic vertebrae C7 to T5 vertebrae and affix to the shoulder blade. The rhomboid’s main action is to drag the shoulder blades back through scapular retraction
Intermediate Layer
- Serratus Posterior Superior is a thin, quadrilateral-shaped muscle, positioned at the upper and back part of the thoracic spine. It stays deep in the rhomboids and inspiration by elevating rib cages 2 to 5 where it affixes.
- Serratus Posterior Inferior is positioned at the junction of the thoracic and lumbar segments. It starts from vertebrae T12 downward to L3 vertebrae and embeds into the 9th through to the 12th ribs. It acts to snatch the lower ribs backward and downwards and assists in trunk rotation and extension. It also assists with forced exhalation.
back muscle
- Thoracic Erector Spinae groups are Iliocostalis; Longissimus; Spinalis the main extensor backward-twisting muscle of the thoracic spine, positioned on either side of the vertebral column.
- Transversospinalis Group muscles are shorter, deep muscles that assist stabilize the spinal segments.
- They are positioned deep to the erector spinae, travel obliquely, and make up the mass of musculature that fills the laminar groove of the spine in the middle of the transverse and spinous processes.
- The transversospinalis muscle group can be separated into three subgroups: from superficial to deep, the semispinalis, the rotators, and the multifidus:
- The Semispinalis affixes superiorly to vertebrae on five or more levels beyond the inferior connection
- The Rotatores affixes superiorly to the vertebrae on one to two levels beyond the inferior connection
- The Multifidus affixes superiorly to vertebrae three to four levels beyond the inferior connection.
The condition affects the thoracic spine
- kyphosis
- arthritis of the thoracic spine
- Radiculopathy
- myelopathy
- bulging disc
- herniated disc
- disc protrusion
- intervertebral disc prolapse
- spondylitis
- spondylolisthesis
- spondylitis
Goals for Thoracic spine mobilization
pain, muscle guarding, and spasm
- painful joint, reflex, muscle guarding, and/or muscle spasm can be checked with slight joint play methods to prompt neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and/or distraction movement is necessary to encourage mechano receptors that may inhibit the transmission of nociceptive stimuli at the spinal cord or/and brain stem level
Mechanical effect
- minor amplitude distraction or/and gliding for movement of the joint is necessary to generate synovial fluid movement, which is an agent for obtaining the nutrients to the avascular part of the articular cartilage
- musical joint play techniques help to maintain nutrient exchange and prohibit the painful and degenerating effects of statis when the joint is swollen or/and painful, and can not go over a range of motion
- when the glide/oscillation force is adjusted to treat pain, muscle spasms and muscle guarding small amplitude methods should not apply stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be checked with a progressively vigorous joint stretching method to elongate hyper mobile capsular and/or ligamentous connective tissue
- uninterrupted or/and distracted stretch forces necessary to amplify a shortened tissue mechanically
Positional faults/subluxations
- A faulty or/and not proper position of one bony companion in addition to its opposing surface may affect the conclusion in limited motion or/and pain
- postural faults can ensue with traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be conserved
- by maladapted neuromuscular control across a joint
- during checking an active range of motion, faulty tracking of the joint surface outcome in pain or/and lessened motions
Progressive limitations
- diseases that progressively prohibit movement can be inspected with joint play techniques to maintain available motion or/and leesen the progressive automated deduction
- the patient’s response is essential for the dosage of distraction or/and glide to treatment and the state of the disease
Functional immobility
- when the patient can’t functionally locomote the joint for a larger period of time
- the joint can be inspected with nonstretch gliding or/and distraction procedure to maintain available joint play and prohibit degenerating and reduce the effect of immobility
Grades for thoracic spine mobilization
- grade 1 small amplitude oscillations and/or glide are used for pain, modulation, commonly during the acute stage of injury
- grade 2 large amplitude oscillations and/or glide are necessary for pain modulation, dosage, and indication same for grade 1
- grade 3 large amplitude oscillation and/or glide that goes up to the preventive joint barrier,
- grade 3 is designed to enhance joint ROM and is used only during the subacute, chronic stage of healing
- grade 4 small amplitude oscillation and/or glide that goes up to the preventive joint barrier,
- grade 4 is intended to improve joint ROM and is used only while the chronic stage of healing
- grade 5 (HVT) high velocity and low amplitude thrust/glide put at the physiologic limit of joint motion
- grade5 grade is performed only one time and solely improves the range of motion
Thoracic spine mobilization
Thoracic spine extension

- patient position: prone with arm lying down comfortably on patient’s side
- put a pillow beneath the thoracic segment to accelerate patient comfort and promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on one side of the patient either right or left depending upon the affected area with your body showing toward the head of a patient
- place the distal phalanx of your 2nd and 3rd finger on the transverse process of the superior vertebral segment to be manipulated
- The thoracic spine extension technique is also known as the V spread technique
- put the hypothenar eminence of your other hand on top of the two-finger contact method
mobilizing force
- exploit an anterior glide, the contact points on the transverse process provide a point of reference
- the other hand exerts pressure through the hypothenar eminence pisiform in an anterior direction
Thoracic spine flexion

- patient position: prone with arm lying down comfortably on patient’s side
- put a pillow beneath the thoracic segment for accelerated patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on one side of the patient either right or left depending upon the affected area with your body showing toward the head of a patient
- place the distal phalanx of your 2nd and/or 3rd finger on the transverse process of the inferior vertebral segment to be manipulated
- The thoracic spine flexion technique also termed as V spread technique
- place the hypothenar eminence of your other hand on the top of the two-finger contact method
mobilizing force
- exploit an anterior glide, the contact points on the transverse process provide a point of reference
- the other hand exerts pressure through the hypothenar eminence pisiform in an anterior direction
- reorganize your pressure for pain modulation or to improve from
Thoracic spine rotation

- patient position: prone with arm lying down comfortably on patient’s side
- place a pillow beneath the thoracic segment for accelerated patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- use v spread contact
- place one finger on the superior transverse process and the second/other fingers on the opposite inferior transverse process to be manipulated
- the finger placement convoy the rule of the lower finger
Rule of the lower finger
- when applying v-spread contact on the opposite side transverse process for thoracic rotation manipulation, rotation of a segment happens in the direction of the finger on the inferior transverse process
mobilizing force
- apply an anteriorly directed force against the transverse process with the opposite hand pressing through the contact finger
pistol thrust

- patient position: supine with arm crossed
Therapist position and hand placement
- stand at the patient’s side showing toward his/her head
- turn the patient toward you and reach above the patient’s body
- contact the inferior vertebrae of the 3 joint complexes to be manipulated by ” using pistol grip “
- one contact is obtained passively to return the patient to the supine position
- to enhance the rotation, use the rule of the lower finger
mobilizing force
- positioned your trunk directly over the segment to be manipulated
- A cephalad distraction force is started with the patient’s body weight at the segment to be manipulated
- apply high-velocity posterior force opposite to the patient’s crossed arm toward the treatment table
Cross arm thrust

- patient position: prone with arm lying down comfortably on patient’s side
- put a pillow beneath the thoracic segment for accelerated patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand beside the patient
- cross your arm and position the pisiform bone hypothenar eminence of one hand on the left side and one hand on the right side of the transverse process of the segment to be manipulated
- change transverse process contact to flexion, extension, or rotation by placing the pisiform bone on the superior and inferior or using a rule of the lower finger
mobilizing force
- An anterior pressure is applied simultaneously by the hypothenar eminence
Fall thrust

- patient position: standing with arms crossed
Therapist position and hand placement
- stand behind the patient
- wrap your arms around the patient
- place a manipulation with put folded towel at the desired thoracic spinal level to direct the force to a specific thoracic segment
- grasp the patient’s elbow alternatively
- if unable to grasp the with the elbow, interlock your fingers in front of the patient
mobilizing force
- bend backward on your heels while applying an extension force on the patient’s thoracic spine then instantly drop down so your feet are flat on the floor
Precaution for spine mobilization
- if a mobilization task causes a change in sensation or an elevated pain to radiate downward an extremity or/and if a patient reports a feeling of dizziness or lightheadedness or does not perform additional manipulations
- use utmost precaution if the patient reports either a current history of corticosteroid use or excessive pain
Joint effusion
- the joint effusion occurs due to trauma or disease of the thoracic spine
- rapid swelling of the spine generally designate
- bleeding in the thoracic spine and may happen with diseases aspiration of the blood to lessen the necrotizing effect on an articular cartilage
- slow swelling for more than 4 hours generally designates serious thoracic spine effusion or edema on the spine due to mild trauma irritability or disease
- do not stretch the inflamed or injured thoracic spine with manipulation because the joint capsule is already stretched by being expanded to accommodate the extra fluid
- the reduction of motion is, in addition, to add extra fluid and/or muscle response to pain, not from shortened fibers
- gentle oscillating motion that does not stress the ligaments may help to block the transmission of a pain stimulus so it is not perceived and may help to begin fluid flow while maintaining available cooperative movement
- if a patient’s response to a slight method is elevating pain or/and joint irritability
- the task was exercised too strenuously or should not be done with the current state of pathology
Inflamation
- whenever inflamation is present, stretching elevating pain and muscle guarding conclusion in greater tissue damage
- gentle oscillatory movements may temporarily decrease the pain response
hypermobility
- the joint of the patient with probable necrosis of ligaments should not be manipulated with stretching tasks
FAQS
- How long do you do joint mobilization for the thoracic spine?
Typical treatment of the thoracic spine joint may add a series of 3 to 6 manipulation grasp on up to 30 seconds, with 1 to 3 oscillations or/and glide per second
- When do we use joint mobilization for the thoracic spine?
The major goal of thoracic spine mobilization is to re-achieve the normal joint play movement that might have been compromised by damage or/and injury. Normal movement of the affected thoracic spine will be re-achieved faster if it is compromised early in the treatment program. Also, mobilization is advantageous in cases when the range of motion is absent in the thoracic spine
- how much time mobilization is given for the thoracic spine?
soft tissue mobilization was applied three times a week and home program exercises were recommended which contain positioning of the thoracic spine
- Why is early mobilization necessary after an injury?
In patients with acute spine injuries, early mobilization prohibits pain and swelling and enhances functional outcomes correlated with cast immobilization
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation initiates rangeless, unachieved the limit of movement, apply the glide for 2 or 3 seconds for 1 to 2 minutes
that goes mid path into the joint range of movement, attending each part of the range and still not reaching the end range. This method can be given to treat stiffness by elevating the range of motion and pain