Special Examination tests for Lumbar Spine dysfunction
Special tests play a crucial role in the assessment and diagnosis of lumbar spine dysfunction. The lumbar spine, located in the lower back, is prone to various conditions and injuries that can cause pain, restricted movement, and impaired function. Special tests are specific physical examinations performed by healthcare professionals to evaluate the integrity and functionality of the lumbar spine.
- These tests are used in the clinic to evaluate the joint dysfunction of the lumbar spine.
- These clinical tests are applied by the therapists when the patient is complaining about lower back pain.
- These tests are used after the patient has already completed the diagnosis with the x -rays.
- These tests are applied to the examination part of the assessment of back pain.
Table of Contents
Name of the special tests of joint dysfunction of the lumbar spine:
- Milgram’s test
- One–leg standing lumbar extension test
- Quadrant test
- Schober test
- Yeoman’s test
- Bragard’s Sign
- Femoral Nerve Tension Test
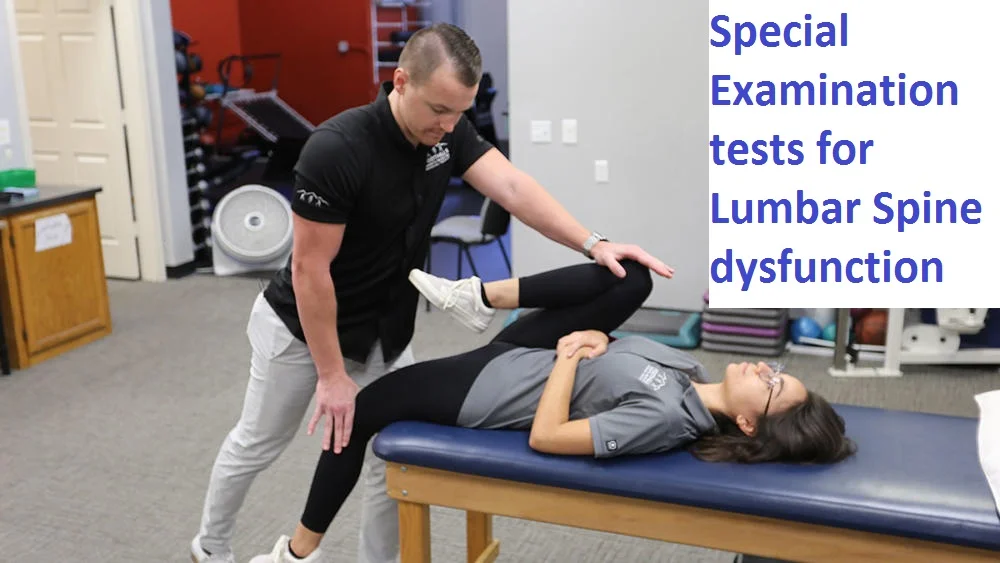
- Leg Lowering Test
- McKenzie Side Glide Test
- Crossed Straight Leg Raise Test
Milgram’s test
- Purpose =The Milgram test is performed to examine any neurological problems in the leg.
- The technique refers to the patient’s initial supine position.
- The patient is next instructed to actively lift both legs off the examination table at the same time, lifting them 5 to 10 cm (2 to 4 inches) off the ground, and keeping them there for 30 seconds.
- Result=If the limbs or affected limb cannot be held for 30 seconds or if symptoms are replicated in the affected limb, the test is considered as a positive test.
- Due to the substantial stress load exerted on the lumbar spine during this test, care should always be taken when doing it.
One-leg standing lumbar extension test

- The purpose of this one-leg standing lumbar extension test is to evaluate the pathophysiology of the facet joints.
- Technique: The patient extends their spine while standing on one leg and balancing.
- The patient is asked to stand on the other leg as the test is repeated.
- Back discomfort and a pars interarticularis stress fracture (spondylolisthesis) are indicators of a positive test, according to the outcome.
- Standing on the ipsilateral limb hurts more if the stress fracture is unilateral.
- Rotation may suggest facet joint disease on the side to which it occurs if it is accompanied by extension and discomfort.
Quadrant test:

- The goal of this quadrant test is to determine the intervertebral forearm’s maximum narrowing.
- Technique: The examiner stands behind the patient while they both stand upright.
The patient then stretched their spine while the examiner (therapist) held their shoulder to regulate the motion.
The examiner can support the weight of the head by using his or her shoulders to grip the occiput.
While the patient’s side flexes and rotates to the painful side, excessive pressure is given in the extension.
Until the range’s upper limit is reached or until symptoms appear, the movement is continued.
As a result, there was a force on the facet joints on the side where rotation occurred and maximal constriction of the intervertebral forearm.
If there are symptoms, the test is positive.
Cipriano described a quadrant test that is comparable to Kemp’s test.
Schober test:-
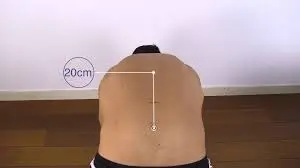
- The purpose of the Schober test is to measure the degree of lumbar spine flexion.
- Technique = The Schober test can be performed to gauge the degree of lumbar spine flexion.
- Between the two PSIS, a point is indicated. Describes the pelvic dimples, which are at the S2 level.
- Points are then drawn at 5 cm (2 inches) below and 10 cm (4 inches) above the level.
- The patient is requested to flex forward while the distance between the three spots is measured, then the distance is measured again.
- The amount of flexion happening in the lumbar spine is shown by the difference between the two measurements.
- Little is known about a Schober test modification that can also assess extension.
- The patient stretched their spine once the flexion action was finished, and the distance between the markings was observed.
- Little also recommended placing four marking points 10 cm (4 inches) between them.
Yeoman’s test:

- The purpose of this yeoman’s exam is to assess lumbar spine discomfort.
- Technique: For the test, the patient is in the prone position.
- The examiner (therapist) extends the patient’s knee while stabilizing the pelvis and extending each patient’s hip in turn.
- Then, with the knee flexed, the examiner (therapist) stretched each of the patient’s legs individually.
- The patient is passive in each scenario.
- Pain in the lumbar spine during any section of the test indicates a positive.
Bragard’s Sign
Purpose
- To figure out if lumbar or ischaemic pain is caused by lumbosacral radiculopathy (such as disc herniation causing nerve root compression), the Bragard’s sign (also known as the Braggard’s test) is utilized.
Technique

- The patient is lying on his back. Straight Leg Raise Test/Lasegue’s Sign: The straight leg is passively raised into hip flexion until the recognizable discomfort appears. The foot is then brought into dorsiflexion as the leg is lowered just below the discomfort threshold. A repeat of the familiar agony is a good indication for Bragard. This would point to a neurological system involvement in the cause of the patient’s suffering.
Evidence
- Homayouni et al. examined the sensitivity and specificity of Bragard’s sign for the differentiation of lumbosacral radiculopathy in research involving 506 individuals. Since the Straight Leg Raise test’s sensitivity and specificity declined as Bragard’s test sensitivity and specificity increased, they observed adequate test performance, particularly in individuals with symptoms lasting less than three weeks.
- The bragard’s Sign sensitivity is 69.3.
The bragard’s Sign has a 76.42 specificity.
Femoral Nerve Tension Test
Definition/Description
- The femoral nerve tension test, sometimes referred to as the femoral nerve stretch test (FNST), is a screening procedure for soft tissue sensitivity to stretching in the dorsal side of the leg, which may be connected to nerve root impingements. Wasserman gave the first description of it in 1919. According to the literature, this test is less frequently utilized than the Straight Leg Raise (SLR) test because upper lumbar radiculopathies are less prevalent than lower lumbar radiculopathies. It evaluates the mobility of the upper lumbar nerve segments and is regarded as an anterior consequence of SLR.
Purpose
- The mid-lumbar (L2-L4) nerve roots and the femoral nerve are both stressed during the prone knee bending test, a neural tension test. The femoral nerve tension test is performed to examine soft tissue at the dorsal side of the leg for sensitivity to stretching that may be related to root impingements.
Clinically Relevant Anatomy
- The inguinal ligament (superiorly), the medial border of the Sartorius’s muscle, and the lateral border of the Adductor Longus muscle form the femoral triangle, which also includes the muscles Pectineus, Iliacus, and Psoas. The lumbar plexus corresponds to where the femoral nerve begins. The femoral nerve is situated (most laterally) in close proximity to the femoral artery and femoral vein.
Technique

- The therapist stands on the side of the patient while they are in a prone position, stabilizing the pelvis with one hand to stop anterior rotation.
- Then, on the other hand, the therapist extends the knee’s maximum range of motion. The therapist then extends the hip while keeping the knee flexed if there are no encouraging indicators in this posture.
- To pinpoint the affected nerve, the therapist might make a few adjustments to the test posture. The lateral femoral cutaneous nerve bias test incorporates an active hip extension, abduction, and external rotation as opposed to the Saphenous Nerve Bias Test, which calls for prone reclining, passive hip extension, abduction, and external rotation along with knee flexion, ankle dorsiflexion, and eversion.
- Normal response: Knee flexion with the heel touching the buttocks is the typical reaction. One might feel a pull or strain in the quadriceps.
- The test is considered positive if there is unilateral discomfort in the lumbar area, buttocks, posterior thigh, or any combination of these sites between 80 and 100 degrees of knee flexion.
- Positive findings in this range might point to a disk herniation impacting the L2, L3, or L4 nerve root when the dura is tensioned between 80 and 100 degrees.
- Based on the range in which pain is recreated, positive findings owing to a disc herniation can be different from quadriceps issues.
When knee flexion is less than 80 degrees, tight quadriceps or an injury may be to blame. In addition, if there is stiffness, the hip flexes in reaction to passive knee flexion, raising the pelvis on that side. Perform the exam on both sides and compare the symptoms since a tight rectus femoris can also cause discomfort in the anterior thigh.
Key Research
- The femoral nerve tension test may occasionally cause ipsilateral sciatica in patients who have a lateral L4/5 disc protrusion.
- The femoral nerve tension test involves lowering and stretching the L4 nerve root. All of the patients (n = 40) who performed this test were confirmed in Christodoulides’ study using myelography, which involves injecting contrast material near the spinal cord and nerve roots while utilizing fluoroscopy, a real-time x-ray technique. Patients were only chosen if it was thought that they had a lateral L4/5 disc protrusion.
- The femoral nerve tension test may also be used to check for high lumbar radiculopathy, a condition characterized by a number of symptoms caused by a problem that starts close to the spine’s root nerves and prevents the nerves from functioning properly.
- This approach, still might not always be reliable. Because the diagnosis is considered positive when it causes pain in the groin, anterior or posterior thigh, buttocks, or lumbar region, for instance, when a person who has tight or injured muscles on the anterior side of his or her thigh undergoes this test, it may turn out to be falsely positive.
- According to studies by Pradeep Suri and colleagues, the femoral nerve stretch test has an accuracy rate of between 88 and 100% for detecting mid-lumbar (L2, L3, or L4) nerve root impingement.
- As the population ages, the probability that this test will be positive increases. Pain is often only induced in the groin and anterior thigh, although it can also occur in the calf, ankle, or foot. Contrary to earlier studies, the crossing femoral nerve stretch test, which is carried out similarly but with the opposite knee flexed, did not increase specificity. A level-specific impingement, low lumbar impingement, or mid-lumbar impingement may be present depending on the results of various physical examination tests, such as the femoral nerve stretch test, which might offer clinical information that significantly changes the likelihood of these conditions. Combining tests increases the accuracy of the mid-lumbar impingement diagnosis.
- The prone knee bend test and the thomas test have a positive correlation, according to a study evaluating hip flexor guarding or tightness using these two tests to assess femoral nerve tension.
- This shows the connection between the length of the iliopsoas muscle and the negative neural stress along the femoral nerve. The results show that patients’ or adaptive hip flexor shortening may result in detrimental neural tension, which may impact hip tightness in normal persons.
- According to another study, incorrectly positive results might occur from the anterior thigh muscles being tight or damaged as well as from hip joint or osseous disease.
- According to a case study, crossed FNST is a useful assessment technique for determining the cause of upper lumbar radiculopathy.
- Two patients’ clinical tests indicated significant lumbar radiculopathy, which the FNST and crossed FNST both corroborated. To determine its prevalence in the evaluation of high lumbar radiculopathy, more research is required.
Evidence
The test’s specificity and sensitivity are unclear.
Leg Lowering Test
Introduction of leg lowering test
- A typical exam to evaluate the core muscles is the double leg lowering test (DLLT). This examination is crucial since weak abdominal muscles can result in bad posture and lower back discomfort.
- The curl-up test is used to measure the strength of the lower abdominal muscles’ muscular fibers. The DLLT is substantially harder than the curl-up test because it examines the muscles as they contract eccentrically while lowering the limbs.
Purpose
- Torso-rectus-abdominis-transverse-abdominis.
The test’s goal is to evaluate your abdominal muscles and your ability to keep your lower limbs from being vertical while tilting your pelvis posteriorly against a load. Together, the abdominal and hip flexor muscles contract eccentrically to regulate the lowering of the leg. The resistance to maintain the pelvis’ posture increases as the legs descend. - The rectus abdominis muscle, as well as the external, internal, and transversus abdominis muscles, all contribute significantly to the effort to keep the low back and pelvis in place while the leg is lowered.
Procedure

- The patient is in a supine position, with the head resting on the floor and the arms crossed over the chest.
The test subject’s lower back is probed with the tester’s fingertips. An alternative is to utilize a pressure biofeedback device or blood pressure cuff that has been inflated to 40 mmHg. - The upper body remains level on the floor, while both legs are elevated vertically to a 90-degree angle.
Before straightening the knee joint, the individual may first bend their knees to get to the starting position.
By tightening their abdominals while their legs are lowered, the subject attempts to maintain the pressure on the tester’s fingers or cuff beneath their lower back.
If the pressure on your hand or the cuff is reduced while the test is running, halt the test, and the angle is measured.
The score is the angle of the legs from the floor, expressed in degrees. A guide to this test’s score is provided below.
Angle Rating
90 = very poor, starting position
75 = poor
60 = below average
45 = average
30 = above average
15 = good
0 =excellent, legs horizontal
Evidence
- Between the DLL test and the core strength test, Spearman’s correlation value was determined to be 0.24.
- The pressure decrease on the pressure biofeedback equipment was 9 mmHg, and the median for the DLL test was 4. The core strength test and the DLL test have a somewhat favorable association, according to the study.
A prospective descriptive study was conducted on a sample of 17 young fit adults to examine the kinematic movement of the pelvis during DLLT. - The sample was divided into two groups, with the first group being told to perform the test while attempting to control the pelvis and the second group descending without doing so.
- According to the study’s findings, there was a natural tendency for anterior pelvic tilting to grow across the range, with anterior pelvic tilt increasing by 1 degree for every 3.6 degrees of lower limb lowering starting with early DLLT.
McKenzie Side Glide Test
Introduction
- Patients have been divided into homogenous subgroups using the McKenzie Method of Mechanical Diagnosis and Therapy (MDT), a classification-based technique, to guide therapy.
- Long, Donelson, and Fung demonstrated that a McKenzie assessment could recognize a sizable subgroup of acute, subacute, and chronic low back patients with a directional preference (an instantaneous, long-lasting reduction in pain after repeatedly performing lumbar flexion, extension, or side glides/rotations tests). A provocative test for people with back pain, specifically low back pain, is the McKenzie side glide test.
Purpose
- The aim of this test is to determine if the patient experiences pain while undergoing the pain provocation test and, if so, during which movements of the test.
- The patient can be categorized into one of the three main McKenzie categories by doing this movement as well as others, such as flexion and extension or side glide.
Technique

- To examine the test, stand behind them while they move. tell the patient to stand with their feet about shoulder-width apart.
- In order to do this action, the patient is told to shift their pelvis and trunk in the opposite direction while keeping their shoulders level and in a horizontal plane. In place of side bending, McKenzie would tell the patient to stand and glide to the side.
- As an example, suppose we are using left-side gliding.
- A shoulder movement over a hip position change from right to left is known as left-side gliding. According to logic, the hip movement must be the antithesis of the shoulder movement. Talk to the patient beforehand to verbally prepare him or her for the glide’s application.
- Although acknowledged, suffering must be honored. Since the test involves active movement, the therapist should not apply additional pressure. The therapist can assist the patient if they are having problems doing this exercise.
- Repeating it both right and left will allow you to compare the quantity and quality of movement.
- Asking the patient whether moving to the left is simpler than moving to the right, and vice versa, can help you determine this. By raising their lower extremity off the ground and hiking their hip, patients may attempt to enhance the motion.
- By supporting the pelvis with your arm as the patient completes the mobility tests, you can reduce this risk. Keep an eye out for any discontinuities in the curve; also, the angle of the curve may point to a region of hyper- or hypomobility.
- Keep in mind how smoothly each intervertebral level contributes to the motion as a whole. Note if the patient’s fear of pain or actually feeling discomfort limits the range.
- A disc protrusion lateral to the nerve root or intra-articular dysfunction may be the cause if the patient’s symptoms worsen when they bend towards the painful side.
- A muscular or ligamentous lesion may be the source of the issue if the patient’s symptoms worsen when they bend away from the painful side and create tightness of the muscle or ligament.
- A disc protrusion medial to the nerve root may also be seen in the patient. A thorough neurological examination will aid in separating the diagnosis.
Evidence
- McKenzie says that the shift occurs when a frontal-plane ROM test of the trunk known as the side glide test changes the patient’s reported pain’s location or severity.
- Therefore, McKenzie suggested using a two-step process to identify the presence of clinically meaningful lateral shifts. The therapist must first assess the patient’s posture when they are standing to see whether there is a lateral shift.
- In order to assess if the location or degree of the patient’s reported pain may be changed, the second phase calls for the therapist to evaluate the clinical applicability of a lateral shift utilizing side-glide tests.
Crossed Straight Leg Raise Test
Background
In 1901, Fajersztajn made the first notice of the crossed straight leg raise test, often known as the “well-leg raising test” or “Fajersztajn sign”. It means that the patient feels discomfort on the ipsilateral, or afflicted side when the contralateral, or unaffected, leg is flexed at the hip.
Purpose
In patients with significant nerve root irritation or compression, positive test results imply central disc herniation, which is connected to lumbar disc herniation in 97% of instances.
The XSLR is more accurate than the straight leg raise test and is often only positive in patients with significant nerve root impingement.
Technique

- Examiner bends their unaffected leg at the hip while keeping their knee extended while the patient is supine.
- When the patient has discomfort in the afflicted leg at a hip flexion angle of 40 degrees, the test is considered positive.
Evidence
- The crossed straight leg raise test is shown to have poor sensitivity but excellent specificity in a systematic review.
- These findings, however, are not generalizable to groups with lower prevalences since they were drawn from populations with a very high prevalence of disc herniation and a severe spectrum of illness.
- The clinical value of the XSLR in identifying disc herniation in primary care populations and other patient populations not (yet) referred for surgery is not supported by sufficient data. While inter-rater reliability for a positive XSLR in two “mixed” samples of individuals was basically none to moderate, intra-rater reliability for a positive XSLR was moderate to considerable.
Clinical considerations
Test findings for diagnosis should be treated with caution due to the lack of inter-rater reliability.
FAQ
Milgrams Test – The patient is lying on the examination table on their back. The patient is instructed to lift both legs a few inches off the table and keep them there. If the patient is unable to maintain this posture owing to back discomfort, the test is positive.
To confirm the diagnosis, the Michelis’ test or unilateral extension test might be conducted. While standing on one leg, the patient performs lumbar spine hyperextension. Pain is replicated in a positive test. When standing on the ipsilateral leg, unilateral lesions frequently cause discomfort.
The Kemp test (also known as the quadrant test and the extension-rotation test) is a provocative examination used to assess pain caused by facet joint dysfunction, such as osteoarthritis. The patient simultaneously stretches and rotates the spine (either the cervical or lumbar spine).
A positive result for both forms of the test is an increase of less than 5cm, which may suggest ankylosing spondylitis (AS). (Image depicts the area of the spine most commonly affected in AS.) Schober’s Test is positive: Forward flexion causes a 5cm increase in length: Ankylosing spondylitis, decreased lumbar spine range of motion.
For the evaluation of sacroiliac joint involvement, the Yeoman test is used. If the discomfort is in the sacroiliac area, it might be caused by anterior sacroiliac ligament disease.
Braggard’s sign is used to assess lumbar disc herniation. Perform a straight leg lift, then drop the leg below the region of discomfort and dorsiflex the ankle passively. If this reproduces the patient’s suffering, the test is positive.
The Bragard test is another complementing physical manoeuvre. When the SLR test is positive at a particular position, the leg is lowered below the angle of radicular discomfort, and foot dorsiflexion is produced. The test is considered positive if there is an increase in radicular discomfort.
Symptoms. Any of the following symptoms might be present: Changes in feeling in the thigh, knee, or leg, such as numbness, tingling, burning, or pain. Weakness of the knee or leg, including difficulties climbing and descending steps, particularly down, with a sensation of the knee giving way or buckling.
The femoral nerve can be checked using the following method. The patient is in the prone position. The examiner elevates the leg while the leg is flexed at the knee (Reverse Lasegue test). Hyperextension of the hip with the leg flexed at the knee produces femoral nerve straining and discomfort.
By tightening the abdominals while the legs are lowered, the person being assessed attempts to maintain pressure on the tester’s fingers or cuff beneath the lower back. If the pressure on your hand or the cuff is reduced during the test, the test is stopped and the angle is measured.
In the evaluation and treatment of spinal pain, the McKenzie technique emphasises the centralization phenomenon, in which pain refers distally and migrates back towards the spine with concentrated repeating motions.
The McKenzie idea is a back pain treatment strategy. Your physiotherapist will teach you to do repeated motions to determine which movements cause your pain. The physiotherapist treating you can then determine which structure is causing discomfort in your spine and treat it effectively.
Position of the patient in a supine laying position to perform the exam. Then, flex the patient’s uninvolved leg at the hip until it is 60-70 degrees. If your patient has shooting pain in the extended leg along the axonal component of the leg, this test is considered as a positive test.
If symptoms appear on the other leg as your doctor elevates the opposite leg, this is considered to a positive result. When no sensations are felt in the contralateral leg, the test is negative.


![Test for tight retinacular [ collateral ] ligaments](https://samarpanphysioclinic.com/wp-content/uploads/2023/06/Test-for-tight-retinacular-_-collateral-_-ligaments.webp)