SI JOINT Dysfunction : Physiotherapy Treatment
Table of Contents
What is SI Joint dysfunction
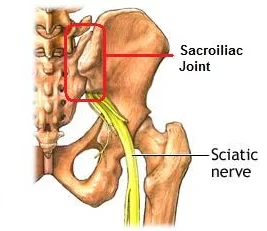
The SI Joint, also known as the sacroiliac joint, is a joint in the pelvis that connects the sacrum (the triangular bone at the base of the spine) to the pelvis. SI Joint Dysfunction is when there is abnormal wear and tear in this joint, causing inflammation and pain in various parts of the body. This can be caused by a number of factors, including injury to surrounding muscles or ligaments, poor posture, or simply being born with a misaligned SI Joint.
The SI joint is located at the front of the pelvis, between the sacrum and the ilium bones. This joint can become dysfunctional due to trauma or injury, but it can also be caused by overuse of the muscles in this area. Symptoms of SI joint dysfunction include pain in this area, difficulty sitting down for extended periods of time, lower back pain, and stiffness.
- Sacroiliac joint syndrome is a significant source of pain in 15% to 30% of mechanical low back pain sufferers.
- The posterior sacral ramus of the spinal nerve is the main nerve that innervates the sacroiliac joint.
- Mechanical dysfunction of the sacroiliac joint results in more pain and decreased mobility.
- The symptoms are often described as pain over the posterior aspect of the joint.
- The pain varies in its degree of severity; it can be referred to the groin, over the greater trochanter, down the back of the thigh to the knee, and sometimes down the lateral or posterior calf to the ankle, foot and toes.
- Sacroiliac joint syndrome occurs when the sacroiliac ligaments are damaged or torn by age causing too much play in the joints.
- This causes an inflammation of the joint making it possible to disrupt.
- Degenerative changes need to be considered as well.
- Traumatic incidents such as motor vehicle accidents, falls landing on the buttocks, and cumulative injuries, such as
- lifting and running, are the most common causes.
- It occurs more frequently in older people, but there is too little research done to substantiate this conclusion.
Description :
The sacroiliac joint is the joint connection between the spine and the pelvis.
- It is a large diarthrodial joint made up of the sacrum and the two innominates of the pelvis.
- Each innominate is formed by the fusion of the three bones of the pelvis: the ilium, ischium, and pubic bone.
- The sacroiliac joints are essential for effective load transfer between the spine and the lower extremities.
- The sacrum, pelvis and spine-, are functionally interrelated through muscles, fascia and ligamentous interconnections.
Clinically Relevant Anatomy:
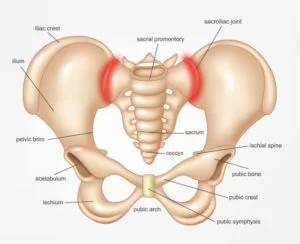
- The sacroiliac joints are located on each side of the spine between the two pelvic bones, which attach to the sacrum.
- Multiple structures are involved in the support and movement of the sacroiliac joints.
- The ligaments which contribute to this synovial joint are the anterior and posterior sacroiliac ligament, interosseus ligament, sacrotuberous ligament, sacrospinous ligament and iliolumbar ligament.
- The joints are surrounded by some of the most powerful muscles of the body, but none of these have direct influence on joint motion.
- The main function within the pelvic girdle is to provide shock absorption for the spine and to transmit forces between the upper body and the lower limbs.
What causes si joint pain?
- It is often hard to determine exactly what caused the wear and tear to the joints. One of the most common causes of problems at the Sacroiliac joint is a trauma.
- The force from these kind of injuries can strain the ligaments around the joint. Tearing of these ligaments leads to too much motion in the joint and over time it will lead to degenerative arthritis.
- Pain can also be caused by an abnormality of the sacrum bone, which can be seen on X-rays.
- Pregnant women have a greater chance to develop sacroiliac joint syndrome. Female hormones are released during pregnancy, relaxing the sacroiliac ligaments. This stretching in ligaments results in changes to the sacroiliac joints, making them hypermobile.
SI joint dysfunction symptoms :
Symptoms of sacroiliac joint syndrome are often difficult to distinguish from other types of low back pain. This is why making a diagnosis of sacroiliac joint syndrome is very difficult. The most common symptoms include :
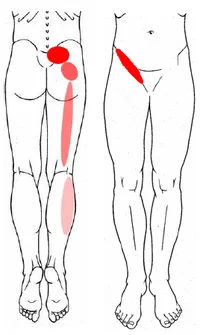
- Low back pain
- Buttock pain
- Thigh pain
- Difficulty sitting in one place for too long due to pain
- Local tenderness of the posterior aspect of the sacroiliac joint (near the PSIS)
- Pain occurs when the joint is mechanically stressed
- Forward bending causes also pain
- Absence of neurological deficit
- Absence of nerve root tension signs
- Aberrant sacroiliac movement pattern
Differential Diagnosis :
Sacroiliac joint syndrome is a controversial diagnosis that includes
- radicular pain
- piriformis syndrome
- ankylosing spondylitis
- lumbosacral facet syndrome
- spondyloarthropathy
- trochanteric bursitis
- hip fracture
- hip overuse syndrome …
Important to notice: the sacroiliac joint syndrome is not a synonym of sacroiliitis!
How is SI joint dysfunction diagnosed?
The Diagnostic of SI Joint pain with a medical history, with type of pain and related symptoms. Physical examination with Extra information, a medical history with information on diet, sleep, and exercise/activity habits, as well as any recent or past injuries that may helpful to the diagnosis of SI joint pain.
Following Provocative test of SI Joint are also helpful in Diagnosis of SI Joint Dysfunction.
Test for SI joint dysfunction :
Your Physiotherapists use a variety of orthopedic provocation tests. The diagnosis can be conclusive if at least one of these tests is positive. Besides the known provocation tests:
- Gaenslen Test
- Sacral Thrust Test
- Thigh Thrust test
- Compression test and Distraction Test
- Yeoman’s test
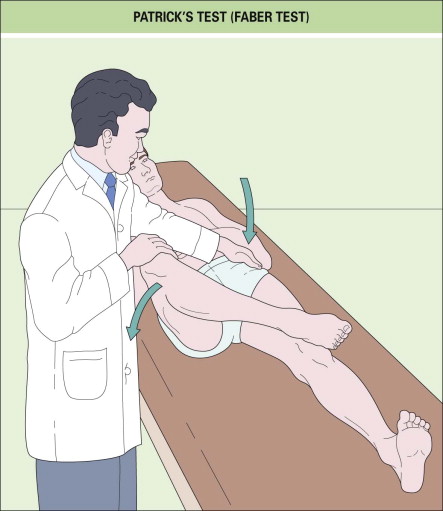
- Faber test (Patrick Sign)
- Gillet test
- Laguerre test
- Sacroiliac Stress Test



Yeoman’s test:

- The patient is prone with the knee flexed 90°.
- The examiner raises the flexed leg off the examining table, hyperextending the hip.
- This test places stress on the posterior structures and anterior sacroiliac ligaments.
- Pain suggests a positive test.
Gillet test:

- The examiner’s thumbs are placed under the posterior superior iliac spine and S2.
- The patient is asked to stand on one leg while moving the opposite leg towards the chest.
- If the joint side that is flexed moves up, this is considered a positive test.
Laguerre test:
- The patient lies supine and the examiner flexes, abducts and rotates the patients affected joint.
- The pelvis must be stabilized and pain signifies a positive test.
- This test differentiates hip pain from sacroiliac pain.
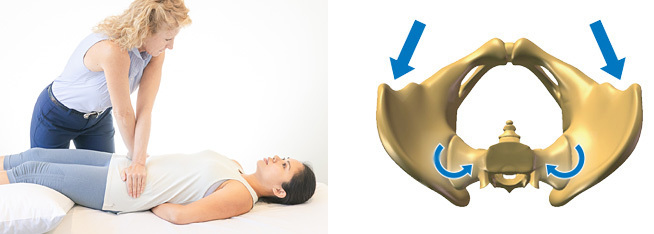
Sacroiliac Stress Test:

- The patient lies supine. The examiner exerts anterior pressure on the iliac wings with both hands.
- By crossing his or her hands, the examiner adds a lateral force to the compression
- Pain is a sign of strained anterior sacroiliac ligaments.
CT and MRI are often used to confirm the diagnosis.
Physiotherapy Treatment :

Primary goal of treatment is
- To reduce the pain,inflammation with IFT (Interferential Therapy), TENS, ice packs, Hot Packs and anti-inflammatory medication medicine.
- To improve mobility using mobilizations, manipulation or exercise therapy.
- If there are complaints of instability, it can be useful to make use of a sacroiliac belt to temporarily support the pelvis, together with progressive stabilization training to increase motor control and stability.
- If the sacroiliac joint is severely inflamed, a sacroiliac belt can also be used.
- postural and ergonomic advice will help the patient to decrease the risk of reinjury.
Exercises for SI joint dysfunction
Core stability–Stabilization exercises:
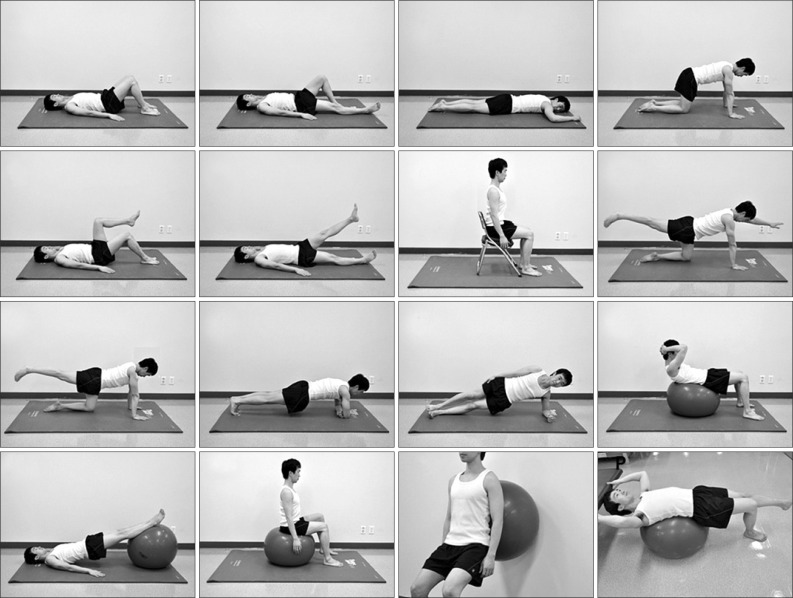
- For lumbar exercises, awareness is necessary in order to isolate the co-contraction of the local muscle system, which happens without global muscle substitution.
- It’s necessary to train the specific isometric co-contraction of two important core stabilizers:
– musculus transversus abdominis
– lumbar multifidi.
- These muscles have to be trained at low levels of maximal voluntary contraction; it’s important to maintain controlled respiration and neutral lordosis in weight bearing exercises.
- It’s really important to take into account the following principles:
-breathe in and out
– tighten the lower abdomen below the umbilicus carefully and slowly without moving the upper stomach, back or pelvis such as a hollowing.
- Furthermore, a bulging of the multifidus muscle may be felt by the physiotherapist.
- There is a need of precise palpation of the muscles to ensure effective muscle activation.
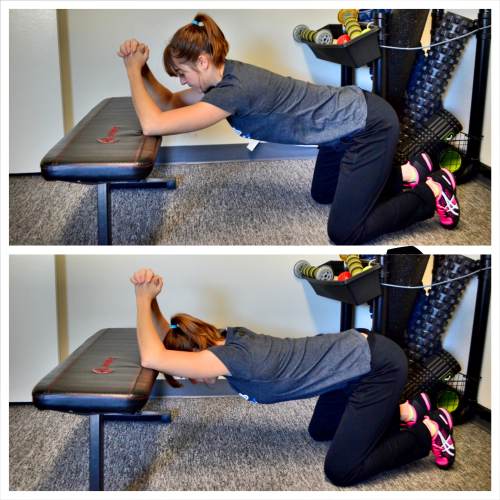
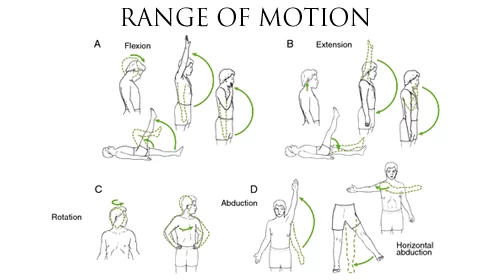
Isolated lumbar stabilizing muscle training:
- Specifically for stabilization exercises, it’s recommended to begin in a quadruped position.
- The physiotherapist can manually guide the spine through the full arc of flexion and extension.
- It’s essential to tuck in the chin and hollow the abdomen by tilting the pelvis posteriorly.
- Lift one arm slowly while continuing to maintain the neutral position of the spine, without changing the natural curves;
- return the arm and then continue with the other.
- The lumbar multifidi can be palpated medial to the lumbar facet joints bilaterally; this allows the physiotherapist to avoid changes in muscle activity of the long spinal extensor muscles, ensuring that the patient is performing the exercise correctly.
- Activation of the musculus transversus abdominis and multifidus together in sitting and standing positions, or while performing stepping and balance activities are essential.
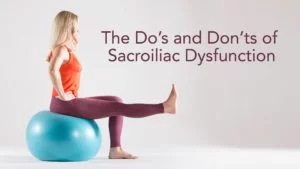
Integration of lumbar stabilization into light dynamic functional tasks:

Sit on an unstable base of support and co-contract the transverse abdominis and multifidus muscles while performing the following stabilizing exercises individually to improve lumbopelvic control-
- hip extension
- lumbar spine extension
- thoracic spine extension with co-contractions.
- These co-contractions can also be performed while walking and performing other activities of daily living.
Integration of lumbar stabilization into heavy-load dynamic functional tasks:


The next exercises are isometric co-contractions to be performed with the addition of heavier external loads to the lumbar spine-
bridging
single-leg extension in quadruped.
- Single-leg extension from quadruped can provide further challenge with alternating arm/leg extensions.
- To increase the complexity and the load of these exercises, single-leg bridging and the bilateral bridging exercises can
- be performed with the lower extremities on an unstable base of support such as a Swiss ball
- Finally an example of an exercise to improve coordination is single-leg bridging with alternating lower extremities on an
- unstable base of support.
- Alternating the stabilizing lower extremity on the Swiss ball further challenges coordination and balance while improving
- the stabilization capabilities of the core musculature.
- During all these exercises the co-contraction of the musculus transversus abdominus and multifidi are imperative.
Manipulation :
- Treatment approached from a multidisciplinary standpoint.
- Conservative treatment consists of exercise therapy and manual therapy. It’s important to determine and address the underlying causes of dysfunction during the treatment.
SI Joint manipulation:
- The patient lies on his back with the therapist standing opposite the side to be manipulated.
- The patient places his hands behind his head and the therapist then moves the patient passively into side bending to end range toward the target side.
- The therapist then delivers a quick thrust to the Anterior Superior Iliac Spine (ASIS) in a posterior and inferior direction.
Lumbar rotational manipulation:

- The patient lies on the unaffected side and the therapist stands opposite the patient, flexing the patient’s hip until the lumbar spine is in flexion.
- The therapist grasps the patient’s lower shoulder and arm to stabilize him, and moves him into left trunk side bending and right rotation, until motion is felt at the desired segment of the lumbar spine.
- The arms of the patient are placed above the therapist’s arm.
- This position is maintained while the patient is rolled toward the therapist. The therapist’s other arm is used to apply a high-velocity low-amplitude thrust to the pelvis in an anterior direction.
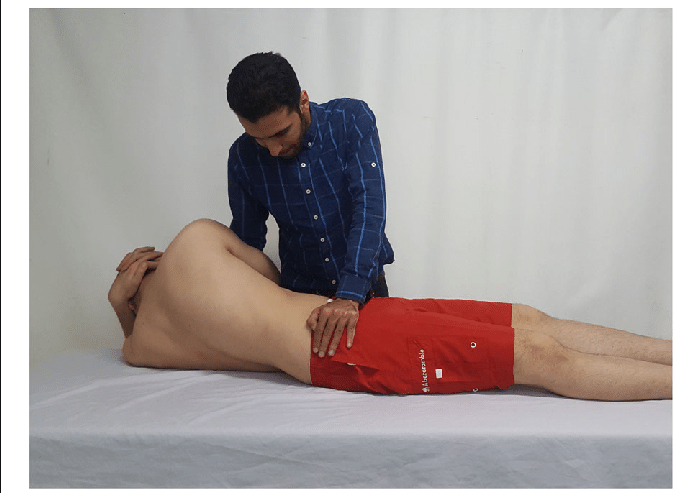
Posterior iliac rotation sacroiliac joint manipulation:
- The purpose of this technique is to manipulate an iliac anterior rotation displacement sacroiliac joint dysfunction and to restore posterior rotation of the ilium.
- The patient lies on his side and toward the therapist.
- The therapist places his hand on the ASIS and the other is on the ischial tuberosity.
- The top hip is flexed to 90° and the other leg is relatively extended. Rotate the spine to the level of the L5-S1 segment pull the patient’s bottom arm in an anterior and superior rotation.
- The hand on the ASIS pushes posteriorly and the other pushes anteriorly.
- This must be maintained for 10 to 30 seconds.
Anterior iliac rotation sacroiliac joint manipulation:

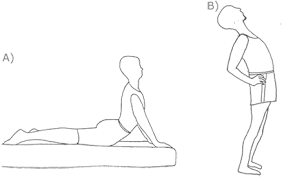
- The aim is to manipulate a posterior iliac rotation displacement to restore anterior rotation of the ilium.
- The patient lies prone with a pillow under his pelvis.
- The therapist supports the thigh just above the knee.
- To stabilize the ilium, the other hand is on the ipsilateral PSIS (Posterior Superior Iliac Spine) pushing in an anterolateral direction.
- The therapist’s fingers should point toward the patient’s feet.
- After positioning, the therapist brings the leg above the table into hip extension just enough to take up the slack in the hip flexors.
- It is recommended to hold this position for 10 seconds with the knee either extended or flexed.
Stabilisation :
Pelvic belt :

- The tension of a pelvic belt is comparable to the muscle activity of the transversus abdominis (and the obliquus internus abdominis) muscle.
- Transversus abominis has an anterior attachment on the iliac crest, an ideal place to act on the ilium producing compression of the SI Joint in combination with stiff dorsal sacroiliac ligaments.
- A minimum contraction of 30-40% of the maximum voluntary force of the transversus abdominis is sufficient to achieve stability of the pelvis according to Richardson et al.
- No greater contraction is needed to achieve joint stabilization because the lever arm of the transversus abdominis is almost equal to the lever arm of the pelvic belt.
- There is also no significant change of stability by increasing belt tension from 50 to 100 N, but if the belt is placed in too low of a position, it may lead to a small decrease of laxity.
- Greater belt tension isn’t recommended secondary to the potential of skin pressure and discomfort.
- When the pelvic belt is worn there is a decrease of the sacroiliac joint laxity.
- This difference in laxity is due to the position of the belt.
- Positioning the pelvic belt just below the anterior superior iliac spines (the high position) is more effective than the low position (at the top of the pubic symphysis).
- However, the tension of the belt has no significant influence on the stability of the SI-joint.
Sacroiliac binder :

- When the use of the sacroiliac belt for a hypermobile SI-joint is appropriate, it should be worn for 24 hours per day up to 6 to 12 weeks.
- This belt should be used in combination with physical exercises and manual therapy in the case of joint dysfunction and muscle imbalance.
- The belt may be removed once the patient has improved control of the lumbopelvic musculature.
- The location of the sacroiliac belt should be at the superior aspect of the PSIS to assist in stabilizing and supporting the pelvis.
ERGONOMICS FOR SI JOINT DYSFUNCTION:
1. Rolling Over in Bed:
To roll over from your back to your side, bend one knee, placing your foot on the bed. Push the heel down, slightly lifting your buttocks and turn towards the side on which the leg is still extended straight. The top arm helps the turning motion.
2. Sitting:
- When sitting (whether you are driving a car, riding a bicycle or sitting on a chair), press your chest upward and let your shoulder blades relax and drop.
- Sitting in a tailor’s position is good (crossed legged with your feet crossed underneath your legs) on the floor or on a very firm bed; use your hands to pull your knees gently back towards your hips and lift your chest, and keep your shoulders low.
- If you have been sitting in this position for a while, stretch forward as far as you can and touch the floor in front of you while keeping your spine straight. At the same time, look up. Practice this stretch as often as it feels necessary and good.
Static Sitting Positions:

- Sit on a chair with your knees apart and slightly turned out
- Sit in positions that relax your lower back while it remains supported, using a cushion or a rolled towel behind your back; sit upright when the back is not supported
- You can also stretch your hips by sitting high enough so that your knees are lower than your hips or by crossing your feet under your chair.
- Use a ball cushion while you are sitting, or sit on a therapy ball; sitting on a ball cushion allows your tailbone to be free. When you use a ball cushion or ball, you develop active stomach and back muscles over time as a result of trying to maintain your balance
- A good posture for resting is lying on your back on the floor, putting your feet up on the couch or bed, with a small pillow to support your back and/or head
- If you have tailbone pain, this may be caused by your pelvic floor being too tight. Favor positions that open your hips, push your legs downward away from your torso (sitting on the edge of the chair or on a ball) or crossing your feet under your chair; let your vaginal muscles relax as much as possible
3. Standing:
- Bend your knees slightly
- Distribute your weight evenly on both legs
- Point your toes slightly outward
- This posture may feel unnatural in the beginning, but if you look in the mirror, you’ll see that it looks quite normal.




Thank you for this wealth of information.