Shoulder Dystocia
Table of Contents
What is Shoulder Dystocia?
Shoulder dystocia happens when the mother’s pubic bone blocks the baby’s anterior shoulder following vaginal delivery of the head. It is usually identified when the shoulders of the infant do not deliver when the baby’s head is gently pulled downward, necessitating the need for specialized delivery procedures. A “turtle sign”—the baby’s head retracting back into the vagina—is indicative of shoulder dystocia. This kind of work is blocked.
The most frequent side effects of shoulder dystocia may be clavicle fractures or brachial plexus injuries, even though the majority of cases are resolved without harming the unborn child. The mother may experience complications such as uterine rupture, postpartum hemorrhage, or an elevated risk of vaginal or perineal tears. Gestational diabetes, a history of the disorder, vaginal delivery, maternal obesity, a considerable infant, and epidural anesthesia are risk factors.
An obstetric emergency is shoulder dystocia. A lady on her back stretching her legs forward and outward, and pushing on her abdomen above the pubic bone are common ways to release a shoulder. If they fail, the lady may be placed on her hands and knees, or the baby’s shoulders may be manually rotated. About 0.2% to 3% of vaginal births result in shoulder dystocia. It is extremely rare for shoulder dystocia to cause death.
Pathophysiology
During typical labor, the fetal head is delivered by extension from the pelvic outlet. After this, the fetal head is restored to its neutral position concerning its spine. As a result, the fetal shoulders are now positioned anteriorly and posteriorly.
Shoulder dystocia is caused by either the posterior shoulder impaction on the sacral promontory or the anterior fetal shoulder impaction behind the mother’s pubic symphysis. The fetus experiences hypoxia in proportion to the time it takes for the fetal shoulders to be delivered.
In obstetrics, applying torque to the fetal head is a common cause of litigation and can cause harm to the fetal brachial plexus.
What are the signs of Shoulder dystocia?
Shoulder dystocia can affect anyone, even though there are risk factors. Shoulder dystocia has no symptoms, and its occurrence is unpredictable. Your obstetrician might not know the problem until you give birth. It is noticeable when your baby’s head comes out and then pulls back in against the perineum, which is the area between your rectum and vagina. This is known as the “turtle sign.”
What causes Shoulder dystocia?
When your baby’s shoulder or shoulders become lodged behind your pubic bones during delivery, it’s known as shoulder dystocia. Shoulder dystocia may result from the following factors:
- If your baby weighs more than eight pounds and thirteen ounces, you have fetal macrosomia.
- Your infant is positioned incorrectly.
- You have an inadequate pelvic opening.
- Your posture restricts the amount of space in your pelvis.
Risk factors
Shoulder dystocia can occur in anyone and cannot be accurately prevented or predicted, despite several established risk factors. Physicians should be prepared to tackle this issue in every birth and know the risk variables to look for in high-risk deliveries.
Risk factors before labor:
- Shoulder dystocia history
- Obesity in Mothers
- Fetal macrosomia, or high estimated fetal weight > 4.5 kg
- Diabetes in mothers (2–4 times higher risk) (Gestational diabetes)
- Being small in stature or having an irregular pelvis
Risk factors during labor:
- Oxytocin/Pitocin need (augmentation of labor)
- prolonged labor in the first or second stage
- Labor Arrest
- Delivery of instruments
Physicians do not advise C-sections for all women with a history of shoulder dystocia because the chance of recurrence is at least 10%. Instead, they advise creating a thorough delivery plan based on the patient’s preferences, future pregnancy objectives, and medical information.
Management
Because shoulder dystocia is an uncommon but critical condition, practicing with obstetric simulations can help healthcare professionals get ready for it. According to research, simulations enhance communication, maneuver usage, and event documentation.
The number of brachial plexus palsy cases decreased significantly from 10.1% before training to 4.0% during training and then to 2.6% after training, thanks to a training program that included lessons on a particular response plan for shoulder dystocia and repeated practice simulations and discussions afterward.
To reduce the risk of brachial plexus palsy caused by shoulder dystocia, the American College of Obstetricians and Gynecologists advises using simulations and adhering to shoulder dystocia protocols to enhance team communication and maneuver utilization.
Procedures
The acronym HELPERR can be used to summarize the processes involved in treating shoulder dystocia:
- Help: Request further assistance from pediatrics, anesthesia, nursing, and obstetrics. Additionally, the patient should be told not to press and to breathe.
- Evaluate for episiotomy: Though usually not required, it should be considered if more movement space is required.
- Legs: The McRoberts technique
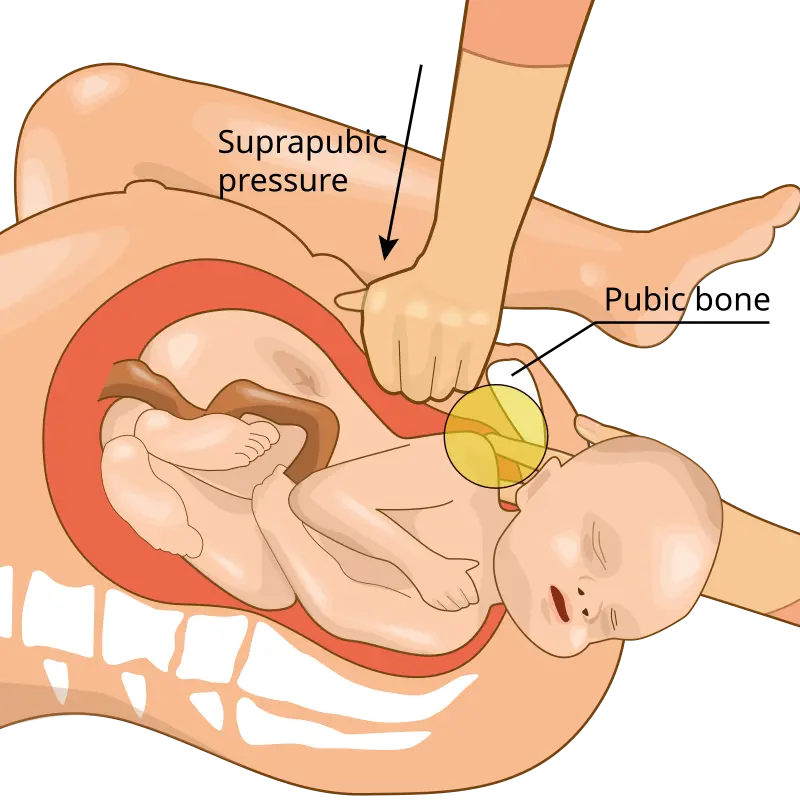
- Pressure: Supra pubic pressure is the pressure.
- Enter the maneuvers. Execute rotational actions
- Remove the back arm.
- Roll over on all fours.
It is not advised to push on the fundus as this may cause the shoulder to become more trapped and may cause the uterus to tear.
To try to make delivery easier, a variety of labor positions and techniques are carried out one after the other. These consist of:
First-line Maneuvers McRoberts maneuver;

- It is frequently the first maneuver done as it is simple, noninvasive, and effective. It includes hyper-flexing the mother’s legs close against her tummy. This flattens the lower back (lumbar spine) and expands the pelvis. This technique is typically used in conjunction with supra-pubic pressure, also known as Rubin I, in which a helper applies pressure with the palm or fist above the pubic bone, directing the pressure on the anterior shoulder laterally (toward the fetus’s face or sternum) and downward (toward the pubic bone). About 58% of shoulder dystocias are relieved when the McRoberts technique and supra pubic pressure are combined.
Second-line Maneuvers
- By applying pressure to the rear of the front shoulder, the Rubin II rotational technique rotates the back shoulder counterclockwise until the front shoulder is delivered.
- Wood’s screw move, which is essentially the reverse of the Rubin II technique, is another kind of rotating maneuver in which pressure is given to the front of the rear shoulder to spin it clockwise until the front shoulder is delivered.
- The posterior shoulder first delivery, also known as Jacquemier’s or Barnum’s procedure, involves identifying the forearm and hand in the birth canal and gently pulling them.
- By placing the mother on all fours with her back arched, the Gaskin technique widens the pelvic exit.
Extraordinary Measures
- The Zavanelli procedure entails a cesarean section after the baby’s head is pushed back in (internal cephalic replacement).
- Cleidotomy, which reduces the shoulder’s diameter to fit through the birth canal by purposefully breaking the clavicle.
- Maternal symphysiotomy breaks the connective tissue between the two pubic bones to make the birth canal opening laxer.
- O’Shaughnessy described abdominal rescue, in which the affected shoulder is delivered vaginally with the help of a hysterotomy.
Complications
Among the potential issues are:
Complications in newborns
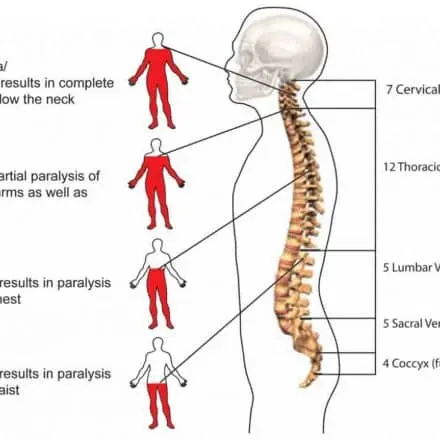
- damage to the brachial plexus (2.3% to 16%)
- Damage to the nerves of the upper brachial plexus is one consequence of shoulder dystocia. These provide the hands, arms, and shoulders with sensory and motor components. Shoulder dystocia is not usually the result of a brachial plexus injury. According to studies, shoulder dystocia is not the only cause of brachial plexus injury; there are other possible reasons as well. The sort of harm a baby has determines how effectively it heals. According to studies, just 14% of newborns with C5–T1 injuries healed completely by 6 months, compared to 64% of babies with C5–C6 or C5–C6–C7 injuries. Certain lesions to the brachial plexus may result in diaphragmatic paralysis, facial nerve damage, and Horner syndrome, or they may cause:
- Klumpke paralysis
- Erb’s palsy
- Fractures of the humerus or clavicle
- Hypoxia, which can occasionally result in:
- Cerebral Palsy
- Death
- Encephalitic in neonates
Complications for mothers:
- postpartum hemorrhage (11%).
- Fourth-degree lacerations of the perineum that penetrate the anal sphincter (3.8%)
- separation of the pubic symphysis
- Lateral femoral cutaneous nerve neuropathy
- rupture of the uterus
Prevention
Researchers have looked at whether bringing on labor before the baby reaches a weight that might raise health issues can help reduce the chance of shoulder dystocia, which is more likely in instances of bigger newborns (fetal macrosomia) or moms with diabetes. Studies examining the impact of induction on shoulder dystocia in full-term pregnancies with suspected larger babies, however, have produced conflicting findings.
Some have found that induction increases the rate of cesarean deliveries without lowering the risk of birth injuries, while other studies have found no effect on cesarean delivery rates and a decrease in shoulder dystocia rates. Regardless of how far along the pregnancy is, the American College of Obstetricians and Gynecologists advises against starting labor simply because macrosomia is suspected and advises against giving birth before 39 weeks unless medically needed.
In situations where fetal macrosomia is suspected, the advantages of selective cesarean delivery have also been investigated. Women without diabetes should think about elective C-sections if their unborn child weighs at least 5,000 g, and women with diabetes should think about them if their unborn child weighs at least 4,500 g, according to the American College of Obstetricians and Gynecologists.
FAQ
What to do during shoulder dystocia?
When shoulder dystocia arises, make it clear that it is present. When shoulder dystocia occurs, the first treatment technique is to raise both legs to the chest (McRoberts maneuver). If supra pubic pressure and the McRoberts maneuver don’t work, think about posterior arm delivery.
How do you treat a baby with shoulder dystocia?
Calling for assistance, halting the mother’s pushing, performing the first-line McRoberts technique with or without supra pubic pressure, and then performing second-line internal movements are all part of management. Before using heroic moves, the sequence should be repeated if first- and second-line tactics don’t work.
Does shoulder dystocia go away?
Most of the time, this is only transitory, and movement will resume in a matter of hours or days. One baby out of every 100 with shoulder dystocia will suffer irreversible harm. Fractures of the infant’s arm or shoulder are among the other problems that can result from shoulder dystocia. These typically heal without any issues.
What causes shoulder dystocia?
The following are the most prevalent risk factors for shoulder dystocia: Infants weighing 8 pounds, 13 ounces or more are considered to have fetal macrosomia. having a brachial plexus damage or shoulder dystocia from a prior birth. obesity in mothers.
What is the best position to avoid shoulder dystocia?
The rate of infant injury is decreased when shoulder dystocia is treated with the hands-and-knee posture as the initial treatment. No issues had been noticed throughout the procedure. For a safer birth, it ought to be implemented into clinical practice.
References
- Wikipedia contributors. (2025b, February 9). Shoulder dystocia. Wikipedia. https://en.wikipedia.org/wiki/Shoulder_dystocia
- Shoulder dystocia. (2025, March 19). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22311-shoulder-dystocia