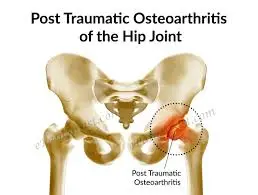
Post-traumatic arthritis
Table of Contents
What is Post-traumatic arthritis?
Osteoarthritis is a degenerative joint condition that affects approximately 32.5 million adults Trusted Source in the United States. It is frequently the outcome of long-duration wear & tear as the cartilage within the joint damages, & the underlying bony changes. Osteoarthritis can take several years to develop. That’s why it is more usually seen in adults over the age of 50. But when an injury occurs, the patient can develop post-traumatic osteoarthritis or Post-traumatic arthritis. This occurs aside from age or the wear & tear on the joint.
Post-traumatic arthritis is inflammation in joints that forms after you’ve experienced trauma. This condition is secondary osteoarthritis It occurs instantly later in an injury contrary to years of wear & tear like other forms of arthritis.
It’s usually a temporary issue, & many patients recover in a few months. Sometimes, post-traumatic arthritis carries on for a longer duration & becomes a chronic disease. It’s rare, but you may need surgery if your symptoms are severe & limit your quality of life. Most patients can handle post-traumatic arthritis with changes in lifestyle & exercise, frequently as the role of their recovery plan from their primary injury.
when trauma leads the smooth surfaces of joints to become irregular, they rub against each other, which causes accelerated wear of the cartilage. On average, 20–50% of patients with joint trauma might develop post-traumatic arthritis. Post-traumatic arthritis is a kind of arthritis & that can pick up any of two forms, osteoarthritis or inflammatory arthritis.
Joint injuries, with or without associated disruption of the articular surface, frequently lead to a progressive process of a severe debilitating condition known as acute post-traumatic arthritis (PTA). post-traumatic arthritis can occur at any age, in any joint, & may occur from any form of acute physical injuries, such as sports, vehicle accident, fall, or military injury. Although one trauma might sometimes be enough to generate arthropathy, repeated injuries, & excess body weight is known to elevate the risk for post-traumatic arthritis.
The acute symptoms following joint trauma involve swelling, synovial effusion, severe pain, & occasionally internal bleeding. Usually, post-traumatic arthritis recovers spontaneously in 2–3 months. The persistence of symptoms following this period should deserve attention & after 6 months, in clinical practice, it might be considered pathological & so-called chronic post-traumatic arthritis. Chronic post-traumatic arthritis can therefore represent an inflammatory disease that persists over time after a joint trauma. The most frequent chronic post-traumatic arthritis is post-traumatic osteoarthritis (PTOA). Nevertheless, a non-negligible number of post-traumatic arthritis might lead to chronic inflammatory arthritis (PTIA), in particular psoriatic arthritis.
What are the symptoms of Post-traumatic arthritis?
Post-traumatic arthritis gives rise to pain & stiffness in the concerned joints. Depending on which joints are impacted, it’ll be hard to walk, run, play sports, or move like patients were used to. The most usual joints affected by post-traumatic arthritis include:
- Ankles
- Knees
- Hips
- Elbows
There are some symptoms that can specify a case of post-traumatic arthritis. It includes the following:
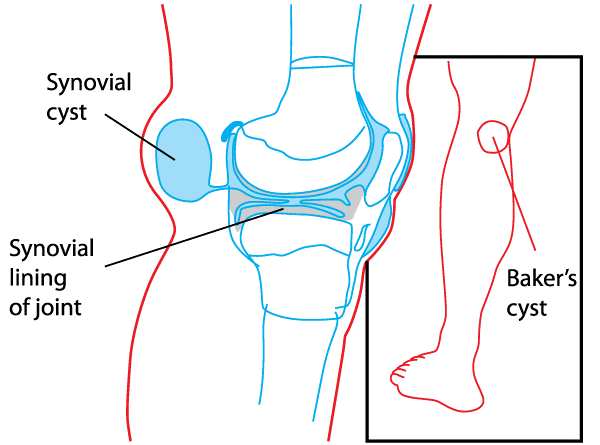
- Swelling of the joint
- Synovial effusion
- Pain in the joint
- Intolerance to weight-bearing activities
- Joint instability
A diagnosis of post-traumatic arthritis can be considered, even more, when this disease develops at an early age. Post-traumatic arthritis generally recovers spontaneously, but if the symptoms are still there after 6 months, it is seen as chronic.
Sometimes the pain comes & goes over a longer period of time. The pain might or might not be accompanied by inflammation of the joint or surrounding area. Frequently the symptoms would disappear without any major medical intervention, these symptoms might re-appear after a while.
What are the causes of Post-traumatic arthritis?
Any injury to any joint can cause traumatic arthritis. It is important to distinguish between regular arthritis and post-traumatic arthritis. Post-traumatic arthritis occurs as an outcome of trauma, while regular arthritis develops slowly without any apparent outside reason. Post-traumatic arthritis is about 12% of osteoarthritis cases. Symptom onset can be as long ago as 2 to 5 years after an injury to the joint was sustained. The cartilage can bruise when too much pressure is exerted on it. This can occur without any superficial appearance of damage. The injury to the joint does not see until months later. More serious injury to the cartilage can lead to loose fragments when the cartilage comes loose from the bone. These loose pieces are unable to restore, and move around in the joint, & can outcome in catching & later pain. These defects do not heal as with bone but are instead filled with scar tissue. Broken-off cartilage requires to be surgically removed from the joint.
Again, it depends on the starting injury. For example, a severe fracture might cause Post-traumatic arthritis to develop sooner than a ligament injury. Post-traumatic arthritis can last a lifetime. It starts as inflammation and turns into a chronic disease and then osteoarthritis.
This can outcome in a lifelong battle with osteoarthritis. While the damage to the joints can not be reversed, doctors can recommend treatment that helps manage the symptoms.
- vehicle accidents
- fall
- military injuries
There are several injuries that can cause Post-traumatic arthritis. Nevertheless, it is most frequently triggered by common sports injuries such as:
- acute ligament strain
- chronic ligamentous instability
- ACL rupture
- meniscus injury
- fracture
- cartilage damage
- or a combination of these
Additionally, some research shows that genetic impacts factor into the development of Post-traumatic arthritis, especially in knee injuries.
How can a patient prevent the risk for post-traumatic arthritis?
Follow these general safety tips to decrease your risk of an injury:
- Always wear a seatbelt.
- Wear good protective equipment for all the activity & sports.
- Make sure the patient’s home & work area are free from the clutter that could trip them or others.
- Always use the proper tools or equipment at home to reach out for things. Don’t stand on chairs, tables, or countertops.
Post-traumatic arthritis is the result of traumas & accidents, so you can’t prevent it.
What are the risk factors of Post-traumatic arthritis?
Since post-traumatic arthritis generally occurs after injuring a joint, the risk of having post-traumatic arthritis after such an injury is significantly higher.^ Risk factors which increase the danger of getting post-traumatic arthritis are being overweight & physical activity. The prevalence of this condition is much higher when doing heavy work & overusing the injured joints. Examinations also revealed that a body mass index (BMI) elevate of five units results in a 35% higher risk of post-traumatic arthritis.
It is reported that genetics do have an impact on the prevalence of post-traumatic arthritis. According to newer examinations, the sex of the patients might also have an influence on post-traumatic arthritis, since females are affected by post-traumatic arthritis more often than males.
What is the classification of Post-traumatic arthritis?
Post-traumatic arthritis is a type of osteoarthritis & the former can occur after the latter. Nevertheless, post-traumatic arthritis can also occur after the development of chronic inflammatory arthritis.
Generally, post-traumatic arthritis is classified into two groups: post-traumatic osteoarthritis & post-traumatic inflammatory arthritis.
- Post-traumatic osteoarthritis
Different studies show that joint injuries substantially increase the risk of osteoarthritis, which further increases with the patient’s age at the time of injury & with time from the onset of the injury. Other studies reported that ranges from 20% to more than 50% of patients who had had joint trauma develop Osteoarthritis & represent ∼12% of all Osteo arthritis cases.
Post-traumatic osteoarthritis mainly affects younger adults than other forms of Osteo arthritis. Indeed, it has been reported that patients with disabling osteoarthritis who had had an articular injury are more than 10 years younger than those who did not have joint trauma. In addition, 13.9% of patients with a history of joint injury during adolescence or young adults developed knee osteoarthritis, compared with just 6% of those without a history of joint trauma.
Common causes leading to Post-traumatic osteoarthritis include intra-articular fractures & meniscal, ligamentous, and chondral injuries. The ankle is the most affected joint, accounting for 54–78% of over 300 000 injuries occurring in the USA alone each year. Knee injuries remain the most prevalent worldwide, with 700 000 cases annually in the USA & 12.5% of Post-traumatic osteoarthritis. Nevertheless, even if less frequent, Post-traumatic osteoarthritis can occur also in other anatomical locations such as the shoulder & hip.
Generally, Post-traumatic osteoarthritis is not clinically diagnosed until the onset of the symptomatic phase, which is highly variable. PTOA might occur early, in less than a year, or remain asymptomatic for a long period of time, even 10–20 years after the trauma. Nevertheless, in both cases, it is increasingly believed that the Osteo arthritis development in the injured joints initiates during the initial traumatic event by intra-articular pathogenic processes, such as apoptosis of articular chondrocytes, subchondral bone remodeling, cellular infiltration, and the release of inflammatory mediators in synovial fluid (SF).
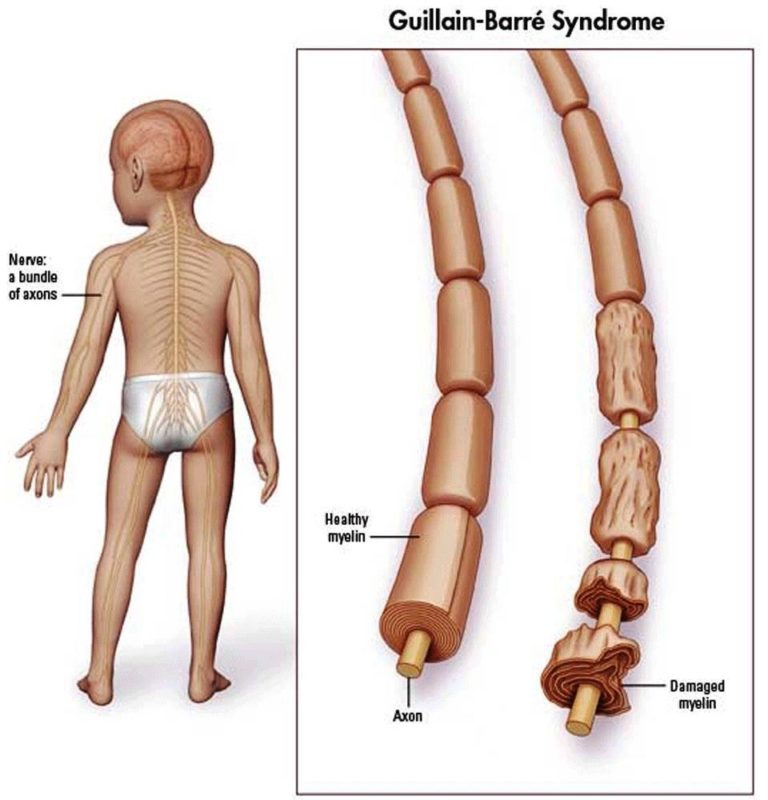
- Post-traumatic inflammatory arthritis
A history of physical trauma might also be found in patients with chronic inflammatory arthritis with the percentage varying from 2% to 25%.5 Trauma is one of the most frequent causes of recurrence of acute attack in gout & pseudogout as an aftermath of crystal shedding. Furthermore, it has been reported that patients who experienced significant joint injuries have an elevated risk of developing calcium pyrophosphate & basic calcium phosphate crystal deposits. Different studies support the idea that a previous physical trauma might also be considered pathogenically relevant in other categories of inflammatory chronic arthritis, including rheumatoid arthritis (RA), juvenile chronic arthritis, juvenile or adult-onset Still’sdisease, & spondyloarthritis, especially PsA. It has been reported that the prevalence of trauma preceding arthritis was higher in patients with PsA than in patients with Rheumatoid arthritis or ankylosing spondylitis. A preceding event was not found to be more usual in patients with Psoriatic arthritis who had positive human leucocyte antigen-B27 status. No difference was noticed between post-traumatic & non-post-traumatic arthritis with regard to their clinical evolution.
Several hypotheses have been suggested to explain the mechanisms behind the onset of Psoriatic arthritis following joint trauma, but the exact pathogenesis is still not clear. A genetic predisposition, a ‘deep Koebner’ phenomenon, & the release of self-antigens or neuropeptides, such as substance P & nerve growth factor, have been proposed. Alternatively, the concept of a synovium-entheses complex & an abnormal innate immunity pathway with an increased release of inflammatory cytokines has been supposed to play a key role in early post-traumatic Psoriatic arthritis (PT-PsA). In this setting, entheses damage after injury might be identified as the initiator of the disease process & leads to the release of different proinflammatory substances, including interleukins, whose access to the adjacent synovium could trigger & perpetuate inflammation. Although all these potential local mechanisms following joint injury have been hypothesized to trigger the development of chronic inflammatory arthritis, it is hard to define a link between the articular damage & causes of systemic events. No specific studies have been conducted to describe systemic consequences of joint trauma, even though an increase in the erythrocyte sedimentation rate (ESR) & in the serum C reactive protein (CRP) levels have been observed in post-traumatic spondyloarthropathy & PT-PsA.
What is the prevalence of Post-traumatic arthritis?
Post-traumatic arthritis is more common at a younger age, especially in healthier & more active individuals. Because Post-traumatic arthritis has an earlier onset, it is often more debilitating than traditional osteoarthritis, which typically develops later in life.
Osteoarthritis, also called wear & tear arthritis, happens from overuse, the natural degeneration of cartilage from aging, or a trauma. It is the very usual form of arthritis.
Post-traumatic arthritis affects more than 5 million population every year. It’s around 10% of all osteoarthritis cases.
You’re seven times more prone to develop arthritis in an injured joint than people who’ve never experienced trauma to their joint.
What is the Differential diagnosis of post-traumatic arthritis?
- Osteoarthritis
- Rheumatoid arthritis
- Juvenile rheumatoid arthritis
- Various pathologies related to specific joints
What is the diagnostic procedure for Post-traumatic arthritis?
The healthcare provider will evaluate post-traumatic arthritis with a physical exam & imaging tests. the healthcare provider will move the joint, ask the patient about the symptoms & compare the joint and its range of motion (how far you can move part of your body) to what it was prior to your injury, if possible.
What tests are done to diagnose post-traumatic arthritis?
After a physical exam, the patient might need at least one of a few imaging tests:
X-rays: An X-ray will confirm and show how damaged the bones in the joint are.
Magnetic Resonance Imaging (MRI): healthcare provider might use an MRI to get a complete picture of the damage to your joint & the area around it. This will show them the bones & the tissue around the joint.
- Outcome Measures
- Hip Disability & Osteoarthritis Outcome Score
- Knee Injury & Osteoarthritis Outcome Score
- Western Ontario & McMaster universities osteoarthritis index, (WOMAC) Osteoarthritis Index,
- Algofunctional index (AFI)
- Intermittent & constant osteoarthritis pain index (ICOAP)
- West-Haven-Yale Multidimensional Pain Inventory (Assesses chronic pain in individuals and is Recommended for use in conjunction with behavioral & psycho-physiological strategies)
- Oxford Hip Scale
- Oxford Knee Score
- McGill Pain Questionnaire Short-Form
CT scan: If a patient needs surgery, a healthcare provider or surgeon needs to know exactly how damaged the joint is. A CT scan will give them a more detailed picture of your bones & the surrounding tissue than an X-ray.
laboratory tests on bodily fluids to find the amount of inflammation around the joints
synovial fluid examinations to differentiate between different types of arthritis
Doctors must consider the outcomes of several such diagnostic tests before making a confident arthritis diagnosis. They will also ask about any previous traumatic injury to diagnose post-traumatic arthritis.
What is the treatment plan for Post-traumatic arthritis?
Post-traumatic arthritis treatment includes:
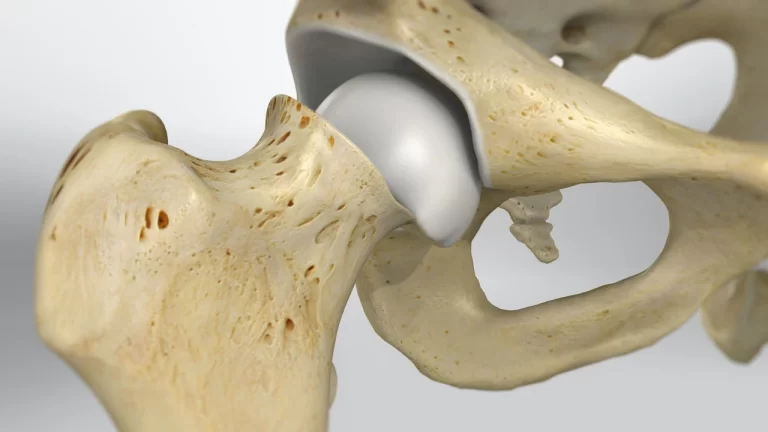
Conservative management is the treatment of the first choice, & surgery is only considered when this fails. Surgical management will determine the affected joint, as well as the extent of damage to the joint. For example, post-traumatic hip arthritis may be managed with a hip replacement when conservative management fails. Medical management can not stop the disease progression of post-traumatic arthritis, but it can be utilized to manage the symptoms. Supplemental glucosamine & anti-inflammatory pain medications are normally prescribed to patients. Management will be very same as that of osteoarthritis.
Weight loss: Being overweight can put extra stress on joints.
Low-impact exercise: Activities like swimming or biking can help patients move their joints & reduce pain while not putting your full weight onto their joints.
Wearing a brace: A brace around your joint can help decrease tension on it & hold it in place.
Medical treatment
Post-traumatic arthritis is cured symptomatically with nonsteroidal anti-inflammatory drugs (NSAIDs). For more moderate symptoms, paracetamol is also utilized. Another medical treatment program is the injection of cortisone or corticosteroid into the affected joint.
Over-the-counter (NSAIDs) like aspirin or ibuprofen can lead to bleeding & other complications after surgery. the surgeon will talk to you about the medications you can take to reduce pain after surgery.
Complications/side effects of the treatment
Side effects of NSAIDs include:
- Bleeding.
- Ulcers.
- Stomach pain.
- Bowel complications.
Treating arthritis is not a quick fix, & it might take a few months for symptoms to go away, but the patient should feel a little better as soon as you start new exercises or physical therapy.
surgical treatment
Surgery for post-traumatic arthritis is rare & is usually only an option when arthritis is so severe that it’s limiting your quality of life. If other treatments aren’t working or you’re still experiencing severe pain after several months, the healthcare provider might recommend surgery. Post-traumatic arthritis surgery includes:
Debridement: Debridement is how surgeons refer to cleaning up something in the body. This means removing damaged tissue or reshaping bones to fix arthritis.
Joint fusion (arthrodesis): the surgeon will insert a plate & screws to keep the bones of your joint together. the patient will have a more stable, pain-free joint, but will have limited flexibility & movement.
Joint replacement (arthroplasty): the surgeon will replace your damaged joint with an artificial joint (made of metal, ceramic or plastic).
Physiotherapy treatment
physiotherapists will create customized exercises & movements to increase your strength & flexibility around your affected joint.
- Activity modification
- Unloading the joint with mobility assistive equipment
- Exercise program’s goal toward regaining range of motion, strength, and coordination
- Weight management
There are various types of therapeutic interventions that might or might not be useful for patients with various degrees of evidence to support them:
Hydrotherapy – this might be particularly useful if the pain is very high & analgesia is not tolerated.
Manual therapy – effective to improve range of motion According to a systematic review, manual therapy mobilization with movement, passive joint mobilization, & patellar mobilization therapy & exercises effectively reduce knee pain & increase functionality. Nevertheless, further research is required to determine the long-term effects of manual therapy on knee arthritis.
Massage – might be useful to manage pain in some subjects, but this has low evidence to show its effectiveness.
Bracing -to support the joint.
Electrotherapy -such as muscle stimulation to improve quadriceps strength & (TENS) transcutaneous electrical nerve supply as it has some evidence to show it can help with pain reduction.
Physiotherapy also plays a major role in the post-surgical management of these patients. The type of surgery will regulate the physiotherapy approach.
What is the outlook for Post-traumatic arthritis?
Post-traumatic arthritis frequently develops following joint trauma. Inflammatory events in the starting phase after injury, such as the increased release of inflammatory cytokines, can predispose to the development of OA or inflammatory arthritis.
Post-traumatic arthritis treatment is a challenging affair to manage. Currently, biochemical markers that predict or correlate with the progression of the disease are lacking, and interventions are limited to restoration and stabilization of the joint. Anti-inflammatory therapy, in particular intra-articular cytokine inhibition, might provide an effective approach for decreasing or preventing chronic disability.
Thus, further studies are needed to identify specific markers for the early detection of the disease progression and to explore innovative opportunities for the prevention of future chronic diseases.
The symptoms that occur during the acute phase of post-traumatic arthritis might spontaneously resolve after a couple of months. Nevertheless, the condition might slowly progress through a long period of no symptoms referred to as a “clinically asymptomatic latency period.”
Even acute post-traumatic arthritis can be challenging to live with because of the pain & reduced mobility that it might cause.
Moreover, those individuals who develop chronic forms of the disease will have to consult a doctor to find the most suitable way to treat symptoms.
Post-traumatic arthritis is something a patient might only have for a few months. But, if you have chronic post-traumatic arthritis, you’ll have to treat it as a long-term condition. the healthcare provider will help you find the best ways to manage your specific symptoms while you heal.
FAQs (frequently asked questions)
Post-traumatic arthritis can disappear, but it depends on various factors. For example, some patient experience symptoms for a few months after an injury or trauma but recover quickly after the initial trauma. Nevertheless, if patient experience symptoms for over 6 months, you might be dealing with a chronic condition. This can cause osteoarthritis, a long-term disease that cannot be reversed.
When post-traumatic arthritis present for more than 6 months, it’s considered chronic arthritis. This is an inflammatory condition that is frequently diagnosed as post-traumatic osteoarthritis or post-traumatic arthritis.
Most people have post-traumatic arthritis short-term, generally around a few months. patient’s symptoms might go away as your body recovers from trauma. If you experience post-traumatic arthritis symptoms for more than six months you could have chronic post-traumatic arthritis, which can last for the rest of your life.
Post-traumatic arthritis can develop months to years following any physical injury to your joints. Most commonly, physicians see arthritic development in patients who have suffered from vehicle accidents, past sports injuries, military injuries, & falls.
It is generally a temporary issue, & many patients recover in a few months. Sometimes, post-traumatic arthritis lasts more & becomes a chronic (long-term) condition. It’s rare, but patients may need surgery if their symptoms are severe and limit their quality of life.



9 Comments