Periarthritis
Table of Contents
What is Periarthritis?
Calcific periarthritis (perry-arth-ritus) is a condition that The crystals can rub against the tendons & muscles and can cause painful swelling around your joints. ‘Peri’ means that the swelling is around the joint, and not inside the joint itself.
Calcium crystals happen naturally in the body & help make our bones & teeth strong. Nevertheless, some persons have too many calcium crystals in other parts of the body – for example:
A tendon (one of the strong cords) that attaches your muscles towards bones – this is referred to as calcific tendonitis in a bursa, a fluid-filled sac that acts like a cushion that allows muscles, tendons, & ligaments to glide smoothly over our bones as you move.
It’s possible to have crystals in a tendon & not know that they’re there, because they might not cause any pain or other problems.
when calcium crystals build around the joints or in the soft tissues surrounding the joint.
But sometimes the crystals can leave the tendon, or ‘shed’, into the soft tissue around the joint. When this happens the hard, sharp crystals can cause pain & swelling as they rub against the soft tissues. This is known as calcific periarthritis.
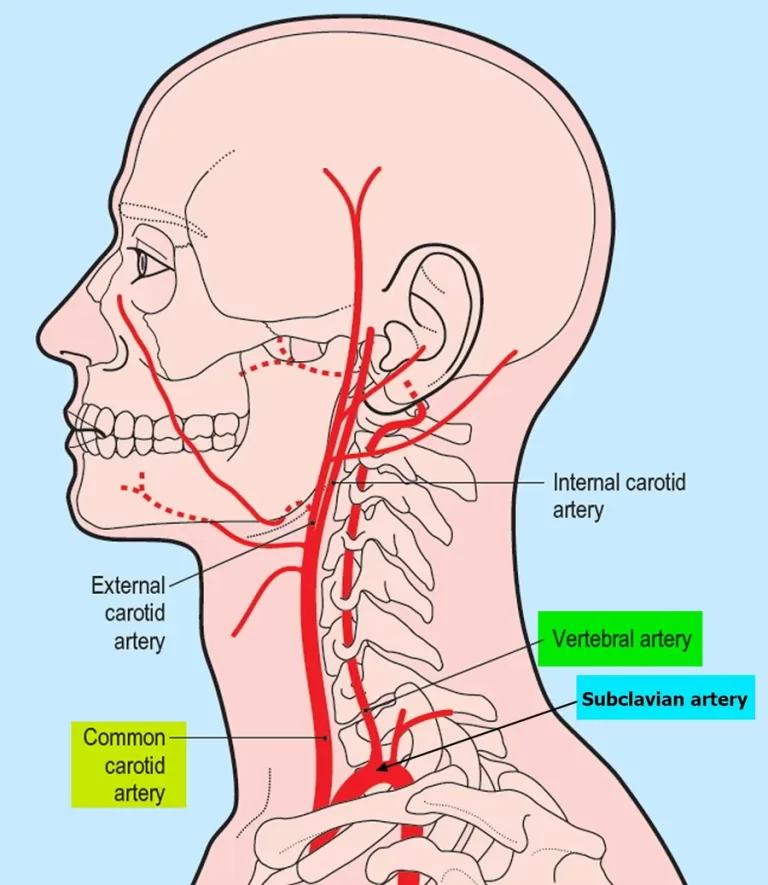
This condition most commonly affects tendons that help the shoulders move, but it can also affect the hips, hands, & other parts of the body.
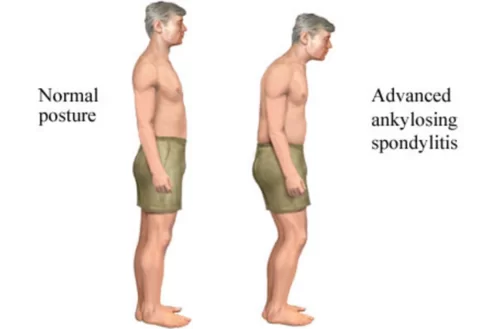
Periarthritis most commonly affects the shoulder. Periarthritis of the shoulder is also called Painful shoulder syndrome, Frozen Shoulder, Periarthritis humeroscapularis, or PHS syndrome
What are the symptoms of periarthritis?
Calcific periarthritis causes pain & swelling around a joint, and the joint might be tender to the touch. These symptoms usually come on quite quickly, which is referred to as ‘acute’ & can be severe.
In most cases, the pain and swelling only occur when the crystals leave the tendon & go into the soft tissues in the surrounding area.
However, if a patient has crystals in a tendon around the shoulder, this can cause problems even if they haven’t shed into the soft tissues. A large crystal, in particular, can be painful & make it difficult to move the arm properly.
Typical attacks of acute calcific periarthritis slowly settle on their own, without causing any damage to the tendon or surrounding tissues.
Even without treatment, the pain & swelling usually start to ease after the first few days & most people find they’re getting back to normal within about four weeks.
Once shedding starts, the crystals generally continue to shed until they’ve all gone. The crystals don’t usually re-form in the same place, so it’s frequently a one-off problem in that particular part of the body.
Nevertheless, if a patient has an attack of calcific periarthritis in one shoulder then you might be more likely to get it in the other shoulder. And some patients go on to have attacks in other parts of the body too.
What are the causes of Periarthritis?
As people get older, natural chemical changes in the body can make it more likely that calcium crystals will form in the blood, urine, or soft tissues.
The following diseases can also cause you to have too much calcium in your body:
an overactive parathyroid gland (hyperparathyroidism)
kidneys that aren’t functioning properly
diabetes – a condition that leads to high levels of glucose, a type of sugar, in the body.
It’s not always clear why crystals start to shed, but it quite frequently happens a day or two after an injury or overuse.
In addition to the less frequent severe traumas when trying to protect while falling, the humerus head can tear, and the tendons are damaged., these are more common overload traumas
Repetitive arms lifting or lifting of excessive heavyweights
Some people present a physical defect in their shoulder for which the area where the cuff is too tight and it damages the tendons.
What are the risk factors of Periarthritis?
Periarthritis is a common condition. It’s the result of too much calcium in the body, & it can happen to anyone, especially as your body ages.
Nevertheless, there are some factors that increase the patient’s risk of periarthritis. These include:
- having diabetes
- having had a stroke
- being between the age of 40 & 65
- being a woman
- having an overactive parathyroid gland or any other thyroid disease
- having had an acute injury to a joint or overusing a joint
- having had a rotator cuff injury
- having a health condition that affects kidney function
- having any heart health condition
- having Parkinson’s disease
- having postsurgical scarring, especially on your shoulders
- having taken certain medications
- leading a sedentary lifestyle
What is the diagnostic procedure for periarthritis?
The doctor will run several tests if they suspect that your pain & stiffness are caused by periarthritis. After a physical exam and discussion of your symptoms and medical history, The affected joint will have very limited mobility. Patient will likely have a series of tests, including:
imaging tests: Imaging tests such as X-rays & ultrasounds can help doctors look for calcium crystals around joints and tendons. During the procedure, a contrast dye is injected into the affected joint, & X-rays are taken. If the patient has periarthritis, the joint will appear shrunken & scarred.
Blood tests can check for:
- inflammation in the body
- calcium levels
- possible other causes of the condition, such as an infection problems with the kidneys, which is a rare case can be a cause of calcific periarthritis.
What is the treatment plan for Periarthritis?
Periarthritis will resolve on its own without any kind of treatment. The calcium crystal buildup generally lasts about 3 years before breaking up. Nevertheless, during this time, periarthritis can be very painful.
Are there any treatments to prevent the crystals from forming?
There are no drug treatments that can prevent the collection of calcium crystals in tendons.
If you have a condition that might increase the likelihood of calcific periarthritis, such as kidney disease or an overactive parathyroid gland, then these should be treated.
Are there any treatments to remove the crystals?
If needed, there are procedures to remove crystals, especially if they are large deposits.
Medical treatment:
Treatments can help the patient manage the pain until the condition resolves. The right treatment for the patient will depend on the severity of the patient’s symptoms. Common treatments for periarthritis are:
Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs can help reduce the pain & inflammation in your affected joint. For mild pain, the doctor might recommend over-the-counter NSAIDs. If your pain is moderate or severe, the doctor might write you a prescription for stronger NSAIDs.
needle aspiration: Periarthritis Sometimes there might be swelling in a bursa, a fluid-filled sac that gives cushioning to your joints. In this case, the doctor might use a needle & syringe to remove extra fluid from the bursa. This is called the aspiration procedure and it can quickly reduce pain.
steroid injections: the doctor will numb the area first, so it isn’t too painful. Usually, once the fluid has been drawn out, the doctor will inject a small amount of a long-acting steroid treatment into the bursa through the same needle. This helps to decrease swelling in the lining of the bursa and prevents the build-up of more fluid.
Surgical treatment for Periarthritis:
Key-hole (or endoscopic) surgery might be utilized to remove a large deposit that is restricting movement and causing discomfort.
As with any surgery, there is some risk of complications, such as infection. If a patient considering surgery, it’s important to discuss this with the doctor.
Shock-wave treatment
A process called shock-wave treatment might be a choice to remove large calcium deposits from a tendon if they’re causing problems. This is most usually done for calcium deposits in a tendon in the shoulder.
High-frequency shock waves are sent to the affected part. The vibrations can help to break up large deposits of crystals & allow the smaller particles to be gradually dissolved away.
The patient usually has a number of sessions of shock-wave treatment spaced about a week apart. Each session only takes about five minutes. Patients might experience some discomfort during the treatment session. You’ll be given an NSAID tablet to reduce swelling & an anesthetic patch to help numb the area. But let your healthcare professional know if you want them to reduce the intensity of the treatment.
This process causes the calcium deposits to shed from the tendon, which is sometimes necessary but itself can cause pain & swelling. Therefore, you might have some tenderness and bruises afterward.
People usually have several sessions spaced about a week apart.
There are a few possible complications from shock-wave treatment, such as the risk of harm to the tendon. Therefore, if the patient is considering this procedure it’s important to discuss it fully with your doctor.
How does Homeopathy help to cure Periarthritis?
Homeopathy is the best treatment for Periarthritis or frozen shoulder, as it is not just profitable but also safe & has no side effects. It enjoys an edge over other systems of medicine as it tackles the main cause & not only the visible symptoms. Being sourced from natural products, it also assures less toxicity.
The symptoms listed against each medicine might not be directly related to this disease because in homeopathy general symptoms & constitutional indications are also taken into account for selecting a remedy.
Commonly indicated Homeopathic remedies
Ferrum. met: Shooting & tearing in the shoulder joint and in the arm, especially right side, pulling or paralytic weakness & heaviness in the arm. Crackling sound in the shoulder joint. Tearing and stinging pain in the arms, especially at night. Uneasiness in the arms. Swelling & desquamation of the skin of the hands. Cramps & numbness in the fingers.
Rhus.Tox: Swelling, stiffness, & paralyzed sensations in joints because of sprains, over-lifting, or over-stretching. Lameness, stiffness, & pain on first moving after rest, or on getting up in the morning, relieved by constant motion. Trembling sensation in limbs. Rheumatic, drawing, & tearing pain in limbs, during rest. Extremely cold hands & feet all day.
Sanguinaria: Rheumatic pain in right arm & shoulder, cannot raise the arm, worse at night in bed (turning in bed), & slightest motion much worse. Pain on the top of the shoulder. Pain in right deltoid. Coldness in body and right arm. Burning of palms. Stiffness of finger joints.
Other indicated remedies: Cal.Phos, Ferrum. Phos, Ruta, Bryonia, Led. pal, Colchicum, Cimicifuga, Causticum, etc.
Physiotherapy treatment for Periarthritis:
The basic aim of exercises are:
- To reduce Joint pain.
- To increase the extensibility of the thickened and contracted capsule of the joint at the anteroinferior border and at the attachment of the capsule to the anatomical neck of the humerus.
- To improve mobility of the shoulder.
- To improve the strength of the muscle. However, it may be remembered that the strengthening of muscles is secondary to mobilization.
Approach to managing pain and mobility:
- Relaxation
- Passive mobilization technique
- Specific shoulder exercises to offer graduated stretching.
Early intervention involves patient education, pain management passive motion exercise, and gentle stretching exercises. These exercises consist of specific joint mobilization exercises to maintain a range of motion within a pain-free window.
Applying an ice pack around the painful area is a quick and safe way of taking the edge off the pain. Patients can buy ice packs, or they could use a pack of frozen peas or ice cubes wrapped up in a damp towel, to protect their skin.
Pain management techniques can include
- heat pack or cold pack
- Ultrasound therapy
- shockwave therapy
- manual therapy
- acupuncture
In later stages physiotherapy intervention can consist of further stretching exercises, postural exercises, strengthening and pain management techniques.
A home exercise program is also prescribed to maintain joint mobility and strength throughout the various phases. Hydrotherapy can also be useful in maintaining shoulder mobility in a pain-free environment.
How can you manage Periarthritis at home?
The patient can also take steps at home to help relieve the pain of periarthritis. Lifestyle steps are a great way to manage the condition between appointments & decrease your symptoms.
the doctor might recommend lifestyle steps that are specific to the joint your periarthritis effects & the severity of symptoms. Common lifestyle management steps include:
- Try to stop smoking. Smoking can increase inflammation in the body. When a patient quits, he can reduce inflammation & pain.
- Apply ice. Ice packs are a simple way to reduce swelling & relieve pain. The patient can use ice throughout the day to help manage her periarthritis.
- Rest. It’s important to get a good night’s sleep as your body heals & recovers.
- Exercise. Keeping your affected joint moving can help promote healing & prevent stiffness. the doctor might order a few physical therapy sessions to help you learn exercises tailored to your periarthritis that you can do at home.
- Manage your weight. Obesity is hard on your joints. Achieving & maintaining a healthy weight can help you decrease pain.
- Consider your diet. The amount of calcium someone eats or doesn’t eat, won’t impact periarthritis. Nevertheless, there are foods that have been shown to reduce inflammation. Following an anti-inflammatory diet could help you decrease pain.
FAQ (frequently asked questions)
What’s the difference between periarthritis and regular arthritis?
There are notable differences between periarthritis & regular arthritis. One of the primary differences is that periarthritis affects the site around a joint, while arthritis affects the joint itself.
Can periarthritis be cured?
Periarthritis is not a chronic condition. It will go away in about 2 to 3 years, even without any treatment. Nevertheless, treatment can help manage painful symptoms. & if symptoms are severe, certain medical treatments can help resolve periarthritis sooner.
What is the difference between periarthritis and a frozen shoulder?
‘Periarthritis’ shows a painful shoulder syndrome that is distinct from arthritis with general radiographic preservation of the joint. Earnest Codman later coined the term ‘frozen shoulder’ in 1934 to emphasize the debilitating loss of shoulder motion in patients affected by this condition.