Pain Neuroscience Education (PNE)
Table of Contents
Description
Pain neuroscience training is an approach used to manage and treat chronic pain. It is based on the understanding that chronic pain is not simply a direct result of tissue damage, but rather a complex interaction of various factors, including physical, psychological, and social factors.
The primary goal of pain neuroscience education is to help people with chronic pain better understand the mechanisms of pain generation and how it is processed in the nervous system. By providing education in the science of pain, this approach aims to empower patients to actively participate in pain management and improve their overall quality of life.
Pain neuroscience training concepts may include:
Neural sensitization:
An explanation of how the nervous system can become sensitized, leading to an increased pain response even in the absence of tissue damage.
Pain Modulation:
Information about mechanisms that can amplify or reduce pain signals, e.g. decrease pain inhibition and facilitation.
Central nervous system changes:
Understanding how chronic pain can cause structural and functional changes in the brain and spinal cord.
Biopsychosocial model:
Understands that pain is influenced not only by physical factors, but also by psychological and social factors such as stress, emotions, beliefs, and social support.
Pain Perception vs. Tissue Damage:
Explains the difference between pain perception and actual tissue damage and how the two can sometimes be distinguished.
Avoidance behaviors:
Addressing the possible consequences of fear avoidance and how they can contribute to the persistence of chronic pain.
Self-management strategies:
Educating patients on various pain management strategies, relaxation techniques, and exercises to improve physical function and reduce pain.
- Training in the neuroscience of pain is often provided by health professionals such as physical therapists, occupational therapists, psychologists, or pain specialists.
- It can be delivered individually or in groups, and the content can be tailored to the specific needs and understanding of the patient.
- Research has shown that pain neuroscience training can be an effective part of a comprehensive pain management program, especially for people with chronic pain.
- By promoting a more accurate understanding of pain and its complexities, patients can experience reduced pain intensity, improved physical functioning, and improved psychological well-being.
- However, as with any treatment, the effectiveness of pain neuroscience training can vary from person to person.
- Therefore, a multimodal and individualized approach to pain management is often recommended.
Application of PNE
Pain neuroscience training can be applied in a variety of clinical and therapeutic settings to help people with chronic pain. This program aims to improve patients’ understanding of pain and promote active self-care. Here are some specific applications of pain neuroscience training:
Chronic Pain Clinics:
- Pain neuroscience training is often used in specialty chronic pain clinics.
- Health professionals such as physical therapists, occupational therapists, or psychologists can provide group or individual sessions for patients with chronic pain.
Physical therapy:
- Physical therapists can incorporate pain neuroscience training into their treatment plans for patients with chronic musculoskeletal pain.
- By educating patients about pain mechanisms and neuroplasticity, physical therapists can help people understand the importance of gradual exposure to movement and functional activities.
Multidisciplinary pain programs:
- Training in the neuroscience of pain is often part of multidisciplinary pain management programs.
- These programs bring together a variety of healthcare providers to address different aspects of chronic pain, including physical, psychological, and social factors.
Pain self-management programs:
- Pain neuroscience training can be part of pain self-management programs where patients are taught to take an active role in pain management and overall well-being.
- These programs provide people with treatment strategies and information to make informed decisions about treatment.
Preoperative education:
- Preoperative pain neuroscience education can prepare patients for surgery and help manage postoperative pain expectations.
- Understanding the neurobiology of pain can reduce the fear and anxiety associated with surgery and recovery.
Occupational Health:
- Occupational health companies can implement pain neuroscience training to help workers with chronic pain manage their symptoms at work.
- This may include task modification strategies, ergonomic adjustments, and stress management techniques.
Primary care:
- Primary care providers can use pain neuroscience training to educate patients about chronic pain and its management.
- This can be especially helpful in cases where people may not have access to specialized pain clinics or programs.
Online Resources:
- Pain neuroscience training materials can also be made available through online platforms, making them accessible to a wider audience.
- This may include informational videos, interactive modules, and written resources.
Sports Rehabilitation:
- Athletes who experience chronic pain from overuse injuries or other musculoskeletal problems can benefit from training in the neuroscience of pain.
- Understanding pain mechanisms can help athletes develop realistic expectations and initiate appropriate rehabilitation strategies.
- Pain neuroscience training is important to adapt to the needs and level of understanding of the individual.
- Healthcare professionals must use clear and relatable language to effectively explain complex concepts to patients.
- In addition, pain neuroscience training works best when combined with other evidence-based pain management methods, such as cognitive-behavioral therapy, physical therapy, and medications, as part of a comprehensive treatment plan.
What is pain?
In pain neuroscience training, pain is understood as a complex and multifaceted experience rather than simply the direct result of tissue damage. Pain is considered a perception that originates in the brain and is influenced by a combination of physical, psychological, and social factors. This method is frequently referred to as the biopsychosocial model of pain.
Here are some key points about the concept of pain in pain neuroscience training:
Pain as a defense mechanism:
- Pain is considered a defense mechanism developed to alert us to potential bodily harm or danger.
- When tissues are damaged or at risk of damage, the body’s nociceptors (pain receptors) send signals to the brain, which interprets these signals as pain.
Nociception vs. pain:
- Nociception refers to the detection of tissue damage or potential damage by specialized nerve fibers called nociceptors.
- It is a physiological process that occurs in response to noxious stimuli.
- However, pain is a subjective experience or perception that arises based on information received by nociceptors in the brain.
Pain as an output from the brain:
- Pain is considered an output from the brain, not a direct input from the body.
- The brain processes multiple inputs from the body such as sensory information, emotional responses, beliefs, memories, and social context to create the experience of pain.
Brain plasticity and pain:
- Chronic pain is often related to changes in the nervous system called neuroplasticity.
- Prolonged pain experience can cause the nervous system to become more responsive to pain signals and increase the pain experience.
Pain perception and context:
- Pain perception can be influenced by various contextual factors, including emotional state, cognitive factors (such as beliefs and expectations), past experiences, social interactions, and cultural background.
Pain as an emergent property:
- Pain is considered an emergent property of the nervous system resulting from the integration of various sensory, emotional, and cognitive inputs.
- This complexity underscores the need to address multiple factors in chronic pain management.
Acute vs Chronic Pain:
- Acute pain is usually related to tissue damage or injury and is a warning signal to protect the body during the healing process.
- Chronic pain, on the other hand, can last longer than the expected healing time and may not be directly related to tissue damage.
- By understanding pain from this neuroscience perspective, people with chronic pain can gain insight into the factors that contribute to their pain experience.
- Pain neuroscience training empowers patients to take an active role in pain management through various coping strategies, lifestyle changes, and behavioral changes, improving their overall quality of life.
- This approach shifts the focus from treating only the source of the pain to the broader context in which the pain is experienced.
What does PNE contain?
PNE, which stands for Pain Neuroscience Education, involves the systematic delivery of information and education to people who suffer from chronic pain. The main goal of PNE is to help patients better understand the complexity of pain, the underlying mechanisms, and how it is processed in the nervous system. By providing this information, PNE aims to empower patients to take an active role in pain management and overall well-being. Here are the main components of pain neuroscience education:
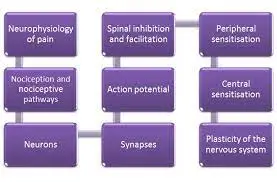
Pain Science Explained:
- PNE provides a comprehensive explanation of the science of pain, covering topics such as nociception, neuroplasticity, central sensitization, pain modulation, and the role of the nervous system in pain perception.
Biopsychosocial Model:
- PNE presents a biopsychosocial model of pain, emphasizing that pain is influenced not only by physical (biological) but also by psychological and social factors.
- This model helps patients understand that their pain is caused by multiple interrelated factors.
Pain perception versus tissue damage:
- PNE explains the difference between pain perception and actual tissue damage and helps patients understand that pain does not always reflect the severity of tissue damage.
Neurophysiology of Pain:
- PNE explains how pain signals are transmitted through the nervous system from the site of injury to the brain and how the brain processes and interprets these signals.
Brain plasticity and pain:
- PNE addresses the concept of neuroplasticity, which refers to the brain’s ability to reorganize and change in response to experience, and how chronic pain can cause neural changes.
Fear-avoidance and pain:
- PNE addresses the potential consequences of fear-avoidance behavior, where patients may avoid certain movements or activities due to fear of pain.
- This can lead to physical recovery and make the pain worse.
Treatment strategies:
- PNE educates patients on various pain management strategies, such as relaxation techniques, mindfulness, stimulating activities, and gradual exposure to movement.
Self-management:
- PNE empowers patients to take an active role in the self-management of their pain by providing tools and strategies for daily pain management.
Addressing misconceptions:
- PNE aims to correct any misconceptions or misconceptions about the pain that patients have developed over time.
Individual approach:
- PNE is often delivered individually or in a group setting, allowing healthcare professionals to tailor training to the specific needs and insights of each patient.
- Pain neuroscience training is usually provided by health professionals with experience in pain management, such as physical therapists, occupational therapists, psychologists, or pain specialists.
- Training can be delivered in person or through various multimedia formats such as videos, manuals, or online resources.
- In addition, PNE is often integrated into a comprehensive pain management program, which may include other treatments such as physical therapy, cognitive-behavioral therapy, and medications, depending on the individual’s specific pain condition.
Indication for PNE training
Pain neuroscience education (PNE) is often used as part of a holistic approach to chronic pain management. It can be useful for people who have persistent or chronic pain that exceeds the expected healing time and for whom traditional treatments may not provide adequate relief. Some of the indications for PNE include:
Chronic musculoskeletal pain:
PNE can be effective for people with chronic musculoskeletal pain, such as chronic low back pain, neck pain, osteoarthritis, fibromyalgia, and other persistent musculoskeletal pain that affects the muscles, bones, and joints.
Central sensitization:
PNE is particularly important in patients with central sensitization, in which the nervous system becomes hypersensitive, amplifying pain signals and causing generalized or stronger pain responses.
Failed conventional treatments:
When conventional treatments such as drugs, physical therapy, or surgery have not provided satisfactory relief, PNE can be considered as part of multimodal pain management.
Fear-avoidance behavior:
PNE is useful for people who have fear-avoidance behavior, where they avoid certain activities or movements for fear of making their pain worse. PNE can help them understand the importance of gradual exposure and pacing of activities.
Persistent pain without permanent tissue damage:
In cases where pain persists despite permanent tissue damage or detectable pathology, PNE can be useful in helping patients understand the mechanisms underlying the pain experience.
Preoperative Education:
Preoperative PNE can be beneficial for patients preparing for surgery, as it can help manage pain expectations, reduce procedural anxiety, and promote a positive recovery experience.
Psychological Factors:
PNE can be beneficial for patients with chronic pain conditions influenced by psychological factors such as anxiety, depression, or stress because it addresses the biopsychosocial aspects of pain.
Empowerment and self-management:
PNE can empower people to take an active role in managing their pain and overall well-being by providing them with information and tools for self-management.
Improve treatment outcomes:
Including PNE in a pain management program can improve treatment outcomes and improve the overall effectiveness of other interventions.
- It is important to note that pain is a complex and individual experience and the effectiveness of PNE can vary from person to person.
- Therefore, PNE is often used as part of a holistic, patient-centered approach that may include other evidence-based treatments such as physical therapy, cognitive-behavioral therapy, medications, and lifestyle changes.
- Healthcare professionals must assess the individual needs of each patient and adapt the treatment plan accordingly to optimize pain management outcomes.
Contraindication
Although pain neuroscience education (PNE) can be beneficial for many people with chronic pain, there are certain situations in which its use may not be appropriate or require careful consideration. Contraindications to the use of PNE are:
Acute pain or recent trauma:
PNE is not usually recommended for people with acute pain from a recent injury or trauma. In these cases, the main focus is to treat the acute wound and promote healing.
Severe psychological distress:
Individuals with severe psychological distress, such as acute major depression, psychosis, or active suicidal ideation, may not be candidates for PNE. Immediate attention to psychological and psychiatric needs is imperative in such cases.
Cognitive impairment:
PNE may not be suitable for people with significant cognitive impairment as they may have difficulty understanding the complex concepts involved.
Limited cognitive flexibility:
Some people may have rigid cognitive beliefs or strong resistance to new information. PNE may not be effective for such individuals because they may be less receptive to understanding pain from a neuroscientific perspective.
Low health literacy:
People with limited health literacy or language barriers may have difficulty understanding complex concepts presented in PNE. In such cases, alternative training methods or additional support may be required.
Lack of patient interest or motivation:
If the patient is not interested in learning the neuroscience of pain or is not motivated to actively participate in pain management, PNE may not be as effective.
Medical Emergencies:
In the event of a medical emergency or life-threatening condition, immediate medical intervention and treatment take precedence over PNE.
Inadequate healthcare provider expertise:
PNE should preferably be provided by healthcare professionals with expertise in pain neuroscience and pain management. If the healthcare provider does not have sufficient knowledge in this area, the management of PNE may not be appropriate.
- It is important for healthcare professionals to assess each patient’s specific needs, medical history, and readiness for PNE treatment.
- The appropriateness of using PNE as part of a pain management program must be determined on an individual basis, taking into account both potential benefits and potential contraindications or limitations.
- In cases where PNE is not appropriate, alternative pain management methods should be considered, and patients may benefit from other evidence-based therapies tailored to their unique circumstances.
Risk factors
The use of pain neuroscience (PNE) education in the management of chronic pain is generally considered safe and beneficial for most people. However, there are certain risk factors or potential challenges that health professionals should be aware of when using PNE. These risk factors include:
Psychological vulnerability:
- PNE involves providing information about the science of pain that may challenge some individuals’ pre-existing beliefs and perceptions about pain.
- For those who are psychologically vulnerable or who have had maladaptive images of pain, this can be difficult and can increase anxiety and distress.
Patient Expectations:
- If a patient has unrealistic expectations about her PNE outcome, she may become frustrated and discouraged if her pain does not improve quickly with education.
- It is important to set reasonable expectations and emphasize that PNE is part of a comprehensive pain management plan.
Emotional reactions:
- Learning about the complexities of pain and its relationship to psychological factors can provoke emotional reactions in some patients.
- For example, patients may become overwhelmed or irritable, and focusing attention on the pain may temporarily increase the intensity of the pain.
Misinformation:
- Some patients misunderstand or misunderstand information provided during a PNE session, which can lead to confusion and misunderstandings about pain.
- For health professionals, using clear and understandable language is critical to ensuring effective communication.
Rejection of the biopsychosocial model:
- It is possible that not all patients readily accept or accept a biopsychosocial model of pain that considers the interplay of biological, psychological, and social factors in the experience of pain.
- This can lead to resistance and non-compliance with PNE.
Inadequate training of health care providers:
- If healthcare providers performing PNE lack adequate training and expertise in pain neuroscience education, intervention effectiveness may be compromised and misinformation may be disseminated.
Cultural and language barriers:
Cultural beliefs and language barriers can affect understanding and acceptance of PSD, especially in different populations.
Attention and concentration:
- Some patients may have difficulty maintaining attention during a PNE session, especially if they are experiencing significant pain or cognitive impairment.
- Health professionals should be aware of these risk factors and take appropriate measures to combat them.
- It is important to tailor PNE to each individual’s needs, provide additional support as needed, and ensure that patients have the opportunity to discuss any concerns or questions they may have regarding the information presented during the training session.
- In some cases, it may be beneficial to combine PNE with other therapeutic interventions such as cognitive-behavioral therapy and mindfulness-based approaches to address the psychological and emotional aspects of pain management.
FAQ
Yes, PNE deals with the interplay between psychological and emotional factors in the experience of pain. This helps individuals develop coping strategies to deal with the emotional aspects of pain.
PNE is primarily designed for people with chronic pain conditions where pain persists beyond the expected healing time. However, some aspects of PNE may also be beneficial for people with acute pain.
PNE can be performed individually or in groups by medical professionals such as physical therapists, occupational therapists, psychologists, and pain specialists. These can be face-to-face sessions, online resources, or a combination of multimedia formats.
PNE covers a wide range of topics including nociception, neuroplasticity, central sensitization, pain regulation, fear avoidance behavior, biopsychosocial models of pain, and coping strategies for pain management.
PNE does not treat pain. Rather, the goal is to provide patients with a deeper understanding of their pain and the tools and strategies to effectively self-manage it.