Iron-deficiency Anemia
Table of Contents
Introduction
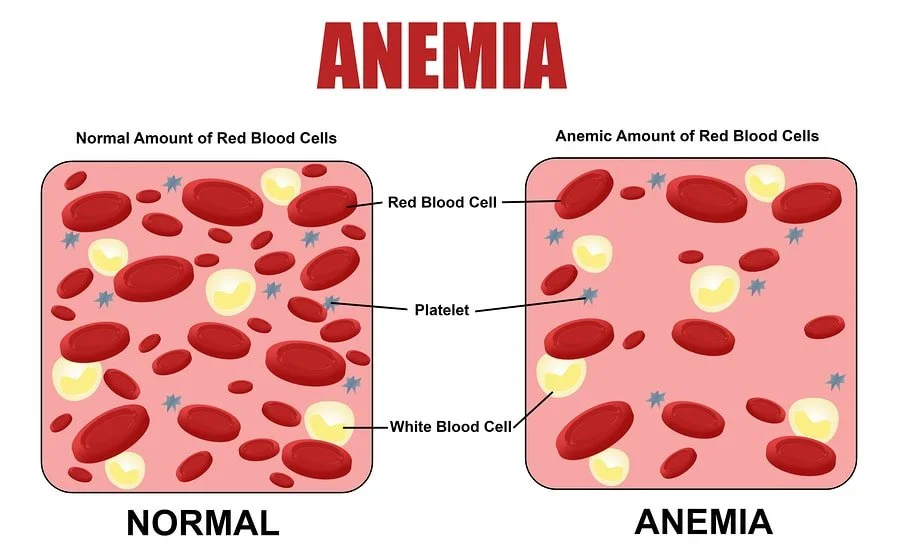
Iron-deficiency anemia is a prevalent medical condition characterized by a deficiency of iron in the body, leading to a reduction in the production of hemoglobin, a critical component of red blood cells.
Hemoglobin plays a vital role in transporting oxygen from the lungs to various tissues and organs, and when its levels are insufficient, individuals can experience a range of symptoms, such as easy fatigue, muscle weakness, pale skin, and shortness of breath. Iron deficiency anemia is a typical type of anemia. RBC carry oxygen to the body’s tissues.
Iron insufficiency causes iron deficiency anemia, as the name implies. If you don’t receive enough iron, your body won’t be able to produce enough haemoglobin, which is necessary for red blood cells to deliver oxygen. As a result, iron deficiency anaemia may cause you to feel exhausted and out of breath.
Iron supplements are typically effective in treating iron deficiency anaemia. Additional testing or treatments for iron deficiency anaemia may occasionally be needed if your doctor suspects internal bleeding.
What is Iron-deficiency Anemia?
A person may have iron-deficiency anaemia if iron levels are low. It can happen for a variety of causes, such as not getting enough iron or losing blood. Red blood cells are affected by anaemia, a blood condition.
When the amount of haemoglobin in your red blood cells (RBCs) declines, anaemia results. Haemoglobin, a protein found in your RBCs, is in charge of carrying oxygen to your tissues.
The most typical type of anaemia is this one. Iron is essential for a number of body functions, including the production of haemoglobin, the oxygen-carrying molecule in your blood. It takes place when your body is unable to produce enough haemoglobin, a component of red blood cells that enables them to transport oxygen throughout your body, due to a lack of available iron. You may experience exhaustion or shortness of breath as a result of an iron deficiency. These signs gradually worsen. If it is determined that you are iron deficient, you might be given iron supplements. The maintenance of healthy cells, skin, hair, and nails also need iron.
Only a small portion of the iron you consume gets absorbed by the body from the food you eat by the cells that line the gastrointestinal tract. When the iron is released into the bloodstream, a protein called transferrin attaches to it and delivers it to the liver. Iron is kept in the liver as ferritin and released as necessary to help the bone marrow produce new red blood cells. When red blood cells are no longer functional (after 120 days in circulation), the spleen reabsorbs them. The body can also recycle iron from these aged cells.
Iron is required for the formation of hemoglobin, a substance found in red blood cells that carries oxygen and eliminates carbon dioxide (a waste product) from the body. Hemoglobin is where the body stores the majority of its iron. Additionally, the liver, spleen, and bone marrow all store around one-third of the body’s iron as ferritin and hemosiderin.
Pathophysiology:
Normally, iron from the food you eat enters your body in a continuous stream. Your body stores extra iron so that it will be available when haemoglobin is needed. When your body uses up its iron reserves more quickly than they can be replenished or when the rate at which iron enters your system has slowed, iron deficiency anaemia develops. There are three steps to this:
First stage: Depletion of iron reserves is the first stage. The amount of iron needed to produce new haemoglobin and red blood cells is currently decreasing, but it has not yet had an impact on your red blood cells.
Second stage: When iron levels are low, the regular synthesis of red blood cells is disrupted. Latent iron deficiency, also known as iron-deficient erythropoiesis, is something you develop. The process of creating new red blood cells is known in medicine as erythropoiesis. Your bone marrow produces red blood cells at this stage but not enough haemoglobin.
Third stage: Iron-deficiency anaemia develops when there is insufficient iron to generate haemoglobin for red blood cells. The haemoglobin concentration will fall below the normal range at this point. At this point, you can start to experience the signs of iron deficiency anaemia.
Risk factors:
Anemia is a common illness that affects both men and women of any age and from any ethnic group. Some individuals may be more susceptible to iron deficiency anemia than others, including:
- Pregnant women
- Women of childbearing age
- Those who eat poorly
- Babies and children, particularly those born preterm or going through a growth spurt,
- People who regularly give blood
- Vegetarians who don’t substitute another iron-rich item for meat
- Teens who need additional iron at periods of rapid growth
- High-performance and endurance adults over 65 persons exposed to lead in the environment or water athletes who run marathons
Nearly anyone can develop iron deficiency anaemia. Women who have menstrual cycles, are pregnant or are nursing, however, are more likely to develop iron deficiency anaemia than men or women who have had menopause. Additionally, the following people are more prone to developing iron deficiency anaemia:
Several newborns between the ages of 6 and 12 months: Iron from the individual who carried the baby throughout gestation is present in the baby when it is born. It takes four to six months for this iron supply to run out. Infants who are exclusively breastfed or who drink formula without iron supplements may not get enough of it.
- Children between 1 and 2 years old: Young youngsters who consume a lot of cow’s milk may frequently not get enough iron.
- Teenagers: Growth spurts may deplete iron stores more quickly, leading to an iron shortage.
- Adults over 65: Because older adults are eating less food, they could not obtain as much iron as they need.
Those who suffer from autoimmune illnesses, bone marrow problems, or other long-term medical concerns.
Causes of Iron-deficiency Anemia
Red blood cells help to carry oxygen to the body’s tissues. In your bone marrow, healthy red blood cells are created. Your body’s red blood cells circulate for three to four months. Your body has organs that get rid of old blood cells, such as your spleen.
Red blood cells need iron to function properly. The blood cannot properly deliver oxygen without iron. Normally, iron enters your body through your diet. Iron from used red blood cells is also recycled.
The body’s iron reserves deplete, which causes iron deficiency anaemia to develop. This is possible because:
- More iron and blood cells are lost than your body can replace.
- The body struggles to properly absorb iron.
- Although your body can absorb iron, you aren’t eating enough meals that are rich in it.
- The body requires more iron than usual (for example, if you are pregnant or nursing).
Iron loss can result from bleeding. Typical reasons for bleeding include:
- Heavy, protracted, or regular menstrual cycles
- Esophageal, stomach, small bowel, or colon cancer
- Esophageal varices, frequently caused by cirrhosis
- Consuming long-term amounts of aspirin, ibuprofen, or arthritis medications, which Might result in gastrointestinal bleeding
- Stomach ulcer illness
A diet’s iron intake may not be fully absorbed by the body because of:
- Celiac illness
- Crohn’s Disease
- Having a gastric bypass
- Consuming excessive amounts of tetracycline or antacids
Other causes:
One of the following may be the cause of iron deficient anaemia:
- Low-iron diets: Our diets provide us with iron, but only 1 mg of that iron is actually absorbed for every 10 to 20 mg taken orally. A person who cannot consume a well-balanced diet high in iron may experience some degree of iron deficiency anemia.
- Body alterations: When the body is through changes, such as growth spurts in kids and teens or during pregnancy and lactation, more iron is needed and more red blood cells need to be produced.
- Anomalies in the gastrointestinal system: Iron malabsorption is frequent following several gastrointestinal procedures. The upper small intestine is where the majority of the iron consumed by meals is absorbed. Any GI (gastrointestinal) tract abnormalities could affect how iron is absorbed and cause iron-deficiency anaemia. The formation of stomach acid is stopped by surgery or medication, which reduces iron absorption.
- Losing blood: Anemia from iron deficiency can develop as a result of blood loss. Injuries, menstrual bleeding, or gastrointestinal bleeding can all cause blood loss.
Iron is lost along with blood. There are several ways that blood might lose:
- Bleeding in the GI tract is caused by colon cancer, ulcer, inflammatory bowel disease, or other GI problems such as celiac disease.
- Surgical procedures or severe wounds
- Bleeding during childbirth or during particularly heavy periods
- Regular use of medications that can cause GI tract bleeding, such as aspirin or nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen and naproxen,
- Bleeding in the urinary tract
- Having issues absorbing iron
Iron-deficiency anaemia can result from a body’s inability to absorb iron, which can be caused by certain illnesses or medications. These circumstances include:
- There are some uncommon genetic disorders that prevent your intestines from absorbing iron or make it more difficult to stop bleeding.
- Sports requiring a lot of endurance can cause athletes to lose iron through their GI tracts and the deterioration of red blood cells.
- Gastrointestinal disorders like Helicobacter pylori infection, Crohn’s disease, ulcerative colitis, and celiac disease
- Including weight loss surgery, stomach and intestinal surgery
Additional medical issues:
Anaemia due to iron deficiency can also result from:
- Kidney disease: An ingredient called erythropoietin is not produced enough in individuals with renal disease. Erythropoietin is required by your body to produce red blood cells. If you have kidney illness, your doctor might advise you to take erythropoietin.
- Chronic diseases that cause inflammation: These include obesity or congestive heart failure. They may make it challenging for your body to manage and utilize its iron.
- If young children do not consume enough iron in their diet, they may occasionally develop iron-deficiency anaemia. This commonly happens as a youngster progresses to eating whole meals between the ages of 9 months and 1 year.
Symptoms of Iron-deficiency Anemia
If the anaemia is minor, you might not have any symptoms.
The majority of the time, symptoms start out modest and worsen gradually. Some signs could be:
- Feeling weaker or less energised than usual, particularly after exercising
- Headaches
- Dizziness
- Palpitations
- Difficulty focusing or thinking
- Broken nails
- Eye whites that are blue Have the urge to eat ice or other non-food items (pica)
- When you get up, you feel dizzy
- Light skin tone
- Breathing difficulty
- Inflamed or sore tongue
- Oral sores
- Uncontrolled leg movement when sleeping
- Hair fall
The following conditions (linked to bleeding) can result in iron deficient anemia:
- Faeces that are tar-coloured or have blood in them
- (Women’s) heavy menstrual bleeding
- Upper abdominal pain as a result of ulcers
Signs of anaemia caused by a lack of iron:
The most typical signs of iron deficiency anemia are listed below. However, each person may have different symptoms. Some signs could be:
- Abnormal skin colour or a lack of colour of skin
- Irritability
- Being low on energy or easily getting tired
- Heartbeat speeding up (tachycardia)
- A sore or enlarged tongue
- Increased spleen
- An urge to eat odd items, such as dirt or ice (also known as pica),
Iron deficiency anemia symptoms can resemble those of other blood disorders or health issues.
Diagnosis:
From general observations on a thorough medical history and physical examination, such as symptoms of easily becoming tired, unusual pallor or loss of color of the skin, or a rapid heartbeat (tachycardia), iron-deficiency anemia may be suspected. Typically, iron-deficiency anemia is identified during a physical examination using a blood test that counts the number of red blood cells and iron levels in the blood.
Exams and Tests:
A healthcare practitioner might request these blood tests to identify anemia:
- Complete blood count
- Reticulocyte count
- Hemoglobin
The following tests may be prescribed by your doctor to screen for iron deficiency anemia:
Size and color of red blood cells: Red blood cells that have iron deficiency anemia are often smaller and lighter in color.
Hematocrit: This is the proportion of red blood cells in your blood that make up the entire volume. For adult women, normal levels are typically between 35.5 and 44.9 per cent, and for adult men, between 38.3 and 48.6 per cent. Depending on your age, these standards could alter.
Haemoglobin: Anemia is indicated by haemoglobin levels below normal. Men should have haemoglobin levels between 13.2 and 16.6 grams per deciliter of blood, while women should have levels between 11.6 and 15 grams per deciliter of blood.
Ferritin. A low amount of ferritin typically denotes a low level of stored iron. This protein aids in the storage of iron in your body.
Anemia caused by iron deficiency is diagnosed through blood testing. Your doctor may order additional tests if you have iron-deficiency anaemia to determine the cause. Your doctor may conduct the following actions to identify iron deficiency anaemia:
- They could examine your red blood cells under a microscope. If you have iron-deficiency anemia, your red blood cells will be smaller than average and pale instead of bright red.
- Your blood’s iron levels will be measured.
- They will assess how much transferrin is in your blood. Transferrin is the name of the protein that carries iron.
- They will measure the ferritin level in your blood. Iron is stored in a protein known as ferritin.
- To ascertain the cause of your low iron, they can advise a colonoscopy or other testing.
Your doctor could issue the following orders to check your iron levels:
- Biopsy of the bone marrow if the diagnosis is unclear
- Iron binding capacity (TIBC) in the blood
- Serum ferritin
- Serum iron level
Your provider may request the following tests to look for iron deficiency causes (blood loss):
- Colonoscopy
- Faecal occult blood test
- Upper endoscopy
- Tests to find the origins of blood loss in the uterine or urinary tract
Added diagnostic procedures:
Your doctor could request additional tests to rule out other potential causes if your bloodwork reveals iron deficiency anemia. These tests might include:
Endoscopy: Using this procedure, doctors can look for bleeding from the stomach, an ulcer, or a hiatal hernia. During this procedure, a tiny, lighted tube with a video camera is passed down your throat and into your stomach. This enables your doctor to examine your stomach and the esophagus, the tube that connects your mouth to your stomach, in order to check for any bleeding.
Colonoscopy: Your doctor might advise having a colonoscopy to rule out lower intestine sources of bleeding. The rectum is used to guide a small, flexible tube fitted with a video camera to your colon. This test frequently involves sedation. Your doctor can look inside your colon and rectum with a colonoscopy to check for internal bleeding.
Ultrasound: In order to rule out uterine fibroids as the source of excessive monthly bleeding, women may also have a pelvic ultrasound.
Depending on the results of a trial period of treatment with iron supplements, your doctor may prescribe these or additional tests.
In addition to a thorough medical history and physical examination, further iron-deficiency anaemia diagnostic techniques may include the following:
Other iron-related blood tests
- Aspiration and/or biopsy of the bone marrow: In order to check the quantity, size, and maturity of blood cells as well as any abnormal cells, a small amount of bone marrow fluid (referred to as an aspiration) and/or solid bone marrow tissue (referred to as a core biopsy) are typically taken from the hip bones. Usually, there is no need for this examination.
- A lower or upper endoscopy: These tests could be able to identify the cause of the blood loss.
Treatment of Iron-deficiency Anemia
Iron deficiency anaemia treatment:
Your doctor will choose a specific course of treatment for iron deficient anaemia based on:
- Age, general health, and medical background
- How severe is the anaemia
- The root of the anemia
- Your level of tolerance for a given procedure, medication, or treatment
- Expectations for the anemia’s course
- Your opinion or preference
Supplementing iron:
To raise the blood’s iron levels over several months, iron supplements can be administered. The stomach may become irritated from iron supplements, and bowel motions may become discolored. To enhance absorption, they should be consumed on an empty stomach or with orange juice. Compared to dietary changes alone, they are significantly more effective. IV iron may be required in cases of malabsorption or intolerance.
Consuming iron-rich meals and taking iron supplements are possible forms of treatment.
The iron stores in your body are increased by taking iron supplements, most frequently ferrous sulfate. Your doctor will typically check your iron level before you start taking supplements.
If you are unable to consume iron orally, you may need to inject it into the muscle or provide it intravenously.
Women who are pregnant or nursing should take additional iron supplements because their diets frequently don’t provide them with enough of the mineral.
Usually, after starting iron therapy, your hematocrit should recover to normal in 6 weeks. To replenish the body’s iron stores in the bone marrow, you will need to continue taking iron for another 6 to 12 months.
Although they are generally well tolerated, iron supplements may:
- Nausea
- Vomiting
- Constipation
Iron-rich foods include:
- Chicken and turkey: Poultry, particularly dark-meat poultry such as chicken, duck, and turkey liver
- Dried lentils, peas, and beans
- Fish: Fish such as sardines, anchovies, and shellfish such as clams, mussels, and oysters
- Meats (liver is the highest source): Beef, hog, lamb, liver, and other organ meats are examples of meats.
- Soybeans, baked beans, chickpeas
- Whole-grain bread
- Iron-fortified white bread, pasta, rice, and cereals
- Leafy greens from the cabbage family, including collards, kale, broccoli, and turnip greens
- Green peas and lima beans, as well as pinto beans, black-eyed peas, and canned baked beans, are examples of legumes
Additional sources include:
- Oatmeal
- Peanuts, raisins, apricots, and prunes
- Kale, spinach, and other greens
Iron absorption by your body is aided by vitamin C. Healthy sources of vitamin C include:
- Grapefruits
- Oranges
- Strawberry
- Kiwi
- Broccoli
- Tomatoes
Complications of Iron-deficiency Anemia
Mild iron deficiency anemia typically has no repercussions.
However, if untreated, iron deficiency anaemia can deteriorate and lead to a variety of medical conditions, including the following:
- Heart problem: When you are anaemic, your blood doesn’t carry as much oxygen, therefore your heart has to pump more blood. An enlarged heart or cardiac failure may result from this.
- Complications throughout pregnancy. Severe iron deficiency anaemia in pregnant women has been associated with early births and low birth weight newborns. However, the condition can be prevented in pregnant women who receive iron supplements as part of their prenatal care.
- Growth issues: Severe iron shortage in children and infants can result in anemia and stunted growth. Anaemia brought on by iron deficiency is also linked to a higher risk of contracting infections.
Summary:
The most typical type of anemia is caused by iron deficiency. It happens when the body do not have enough iron. A few possible causes include menstrual blood loss, difficulty absorbing iron, and a shortage of meals high in iron.
Anemia can be detected using blood tests.
You should refrain from trying to diagnose and treat iron deficiency anemia on your own. Your blood may become too iron-rich, which might cause additional health problems like constipation and even liver damage.
FAQs:
What is a normal level of iron?
For men, normal iron values range from 70 to 175 mcg/dL. Women range from 50 to 170 mcg/dL. For kids, the range is 50–120 mcg/dL.
Is anaemia caused by a lack of iron serious?
Untreated iron deficiency anaemia can increase your chance of getting sick or infected because iron deficiency weakens the immune system. It could increase your risk of developing heart or lung conditions like tachycardia (excessively rapid heartbeat) or heart failure.
What food contains the most iron?
Iron-rich foods
Suitable sources include:
Morning cereal and toast supplemented with iron.
Seeds and nuts.
Dried fruit.
Legumes, including chickpeas, lentils, baked beans, and mixed beans.
Dark leafy greens, including broccoli, spinach, and silver beet.
Tofu.
Iron deficiency anemia is detected in what ways?
Your doctor will request a blood test to assess your complete blood count (CBC), hemoglobin levels, blood iron levels, and ferritin levels to help identify iron-deficiency anemia. Your doctor might inform you that you have low blood iron levels.
Can anemia lead to hair loss?
Despite contradicting results from different research about the link between iron deficiency and hair loss, the majority of medical professionals concur that a dangerously low level of iron in the blood can affect the physiological function of hair follicles, harming them and causing hair loss