Intermittent Claudication
Table of Contents
Introduction
Intermittent claudication is a medical condition characterized by pain and cramping in the legs during physical activity, such as walking or exercising. It occurs as a result of reduced blood flow to the muscles in the legs, usually due to narrowed or blocked arteries.
Typically, it’s a sign of major health issues and consequences such as peripheral artery blood flow issues. However, with early identification and treatment, this illness is typically manageable.
What is Intermittent Claudication?
When you move, you only have intermittent claudication in your muscles, which goes away when you are at rest. A reduction in blood circulation can create pain that is so severe that it even interferes with claudication in some circumstances. Severe medical issues can be indicated by this type of pain.
Why do some people experience Intermittent Claudication?
A component of flow is disrupted by intermittent claudication, a circulatory issue. Ischemia (iss-key- me-uh), a condition when there is a lack of blood flow, causes an oxygen shortage in the affected body parts. The affected area may get damaged, and the affected cells may potentially die, if ischemia persists for an extended period.
Usually affecting your legs, intermittent claudication gets its name from the fact that stopping and taking a break makes it go away. That occurs when you are exerting more energy and need more oxygen than your blood can carry. Since those cells don’t require as much oxygen while you’re sleeping, there is an adequate supply to meet demand.
What are the causes of Intermittent Claudication?
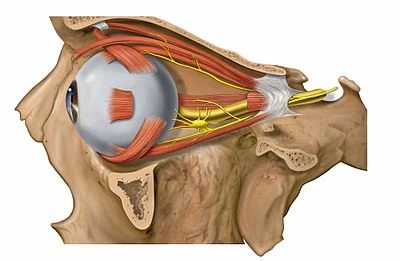
Peripheral artery disease is claudication’s most common cause. The big arteries that carry blood to the arms and legs are called peripheral arteries.
Damage to an artery that reduces blood flow to an arm or leg (a limb) is known as peripheral arterial disease. The restricted blood flow is typically adequate when you’re at rest. But even while you’re moving around, your muscles aren’t getting enough oxygen and nutrients to function properly and stay healthy.
Atherosclerosis is typically what damages peripheral arteries. Atherosclerosis is the term for the buildup of lipids, cholesterol, and other substances in and on the arterial walls. The arteries may narrow as a result of plaque, preventing blood flow. The plaque may crack and cause a blood clot.
What is the risk factor of Intermittent Claudication?
There are several potential risk factors for claudication and peripheral artery disease.
- A family history of atherosclerosis, peripheral artery disease (PAD)
- if you also smoke or have diabetes
- Age older than 70 years
- Chronic kidney disease
- Diabetes
- High blood pressure
- High cholesterol
- Obesity (a body mass index over 30)
- Smoking
What should I expect to feel with Intermittent Claudication?
Claudication typically causes dull, agonizing pain. Additionally, it could feel like a muscle cramp or spasm (also known as a “Charley horse”) or like your muscles are getting tired. The pain will feel worse the more activity or effort you put into it. In some circumstances, you might also experience numbness as a result of inadequate blood flow to the adjacent nerves.
The fact that claudication only affects muscles is important. Joint discomfort and arthritis are not brought on by it. Once you stop and rest, the pain should also subside in a few minutes, if not less. It’s more likely that this is the case if the pain is in one or more joints or persists for many minutes after you stop to rest.
Differential Diagnosis of Intermittent Claudication
- Sciatica
- Atheroembolic disease
- Venous insufficiency
- Vasculitis
- Osteoarthritis of the hip
- Spinal cord compression
- Disc Prolapse Radiculopathy (eg. slipped Disc)
What medical tests are likely with this symptom?
Even though intermittent claudication is a symptom rather than a specific medical issue, if you experience it, your doctor will probably request tests. These tests can assist diagnose the problem, rule out other conditions or issues, and help choose the best course of action.
If you experience intermittent claudication, you could undergo the following tests:
Physical examination
During a physical examination, a medical professional will check several areas of your body for any telltale symptoms of an issue. A stethoscope will listen to the pulses in your legs and feet in addition to a visual examination. If the pulses in your legs or feet feel or sound weaker than usual, or if they are impossible to feel or hear, that is a major warning sign that they are searching for.
Ankle-brachial index
The ankle-brachial index (ABI) test monitors and contrasts your ankle and arm blood pressure. You may develop claudication in one or both legs if the ankle pressure value is much lower than the arm reading.
Many times, medical professionals will take your blood pressure, have you walk on a treadmill, and then take another reading once you’ve finished. If you have a problem, comparing those measurements will help you assess how serious it is.
Arteriogram
In this test, a substance called contrast is injected into an artery in the potential site(s) for intermittent claudication. The circulation in that location can be seen by medical professionals thanks to the contrast’s brightness and visibility on an X-ray. They frequently observe circulation declines that accompany intermittent claudication.
Other imaging tests
Other imaging procedures that can aid in identifying the underlying cause of intermittent claudication may occasionally be tried by medical professionals. These consist of:
- Magnetic resonance imaging (MRI).
- Computed tomography (CT) scan.
- Vascular ultrasound.
What is the treatment of Intermittent Claudication?
Treatment for claudication can take many different forms, but they all aim to increase blood flow to the painful areas. Unfortunately, claudication also raises your risk for major circulatory and cardiac issues, so therapy typically includes precautions to avoid such side effects.
The remedies you can try are those listed below.
Medications
In the management of intermittent claudication, drugs frequently play a significant role. These medications often assist in enhancing circulation or preventing significant issues that are more likely to arise as a result of claudication. These often consist of:
Blood-thinning medications. These medicines lessen the capacity of your blood to clot. This is crucial because it guards against potentially fatal complications including pulmonary embolism, stroke, or blood clots that can form and clog the arteries in your legs.
Statins. These drugs reduce the amount of cholesterol in your blood. A plaque’s ability to form more quickly can be impacted by high cholesterol levels. By bringing those levels down, you can avoid both the accumulation and any associated problems like heart attacks.
Blood pressure medications. Your blood vessels will normally relax and broaden as a result of these drugs, boosting blood flow. Increasing blood flow can significantly reduce or eliminate claudication-related discomfort. Additionally, these drugs aid in the prevention of conditions including heart attacks and stroke.
Diabetes-controlling medications. Blood pressure, cholesterol, and your chance of developing heart disease are all strongly correlated with diabetes. Using medicine to manage your diabetes, if necessary, can also help you avoid difficulties with your heart and circulation system.
Minimally invasive techniques or surgery
Procedures called “revascularization” that increase blood flow can lessen or eliminate the discomfort associated with intermittent claudication. Following are some potential procedures:
In a minimally invasive treatment called percutaneous transluminal angioplasty, a catheter—a long, tube-shaped device—is inserted into a significant blood arterial, typically the one at the top of your thigh. When the arteries are close enough to create claudication, they direct the catheter via your blood vessels to those locations. They can then blow up a balloon to expand the artery after they have reached the narrowed location. They can also insert a stent, a scaffold-like device that keeps the artery open to allow for simple blood flow.
Bypass surgery. This treatment creates a detour-like path for blood to travel by using a blood artery from another part of your body. Once implanted, that bypass offers sufficient blood flow to avoid sporadic claudication.
Atherectomy. Plaque accumulation inside arteries that are already restricted is removed during this operation using a catheter device.
Physical Therapy
Exercise program prescription by physiotherapists is the least invasive and most effective treatment for PAD. Walking until one can tolerate the pain, pausing for a brief rest, and starting to walk again as soon as the pain subsides are all part of exercise therapy. For at least 12 weeks, these walking sessions should last 30 to 45 minutes, three to four times per week. Supervised exercise programs for PAD are more efficient, but insurance companies frequently do not cover them.
The most effective exercise regimen for PAD summarised their results in this way.
Patients with PAD perform better on the treadmill when under supervision.
Exercise on a supervised treadmill improves treadmill walking performance more than exercise at home.
Home-based walking exercise programs that incorporate behavioral techniques are more beneficial than supervised treadmill workouts for people with PAD who are experiencing functional impairment.
Patients with PAD who use upper and lower extremity ergometry walk faster and breathe more deeply.
Although it can help PAD patients perform better on the treadmill, lower extremity resistance training is not as efficient as under supervision treadmill exercise.
Exercise Recommendations for Patients With Claudication Under Supervised Exercise Treadmill Training
Walking on a treadmill while being monitored
Intensity during a 6-MWT that causes claudication within 3–5 minutes or a 40%–60% maximal workload based on a baseline treadmill test.
30 to 50 minutes of intermittent exercise per session; the objective is to walk for at least 30 minutes each time.
Claudication force as tolerated, mild to moderate/severe claudication
The ratio of work to rest To reach moderate to moderately severe claudication, the walking time should be between 5 and 10 minutes, and then the patient should stop walking and rest for 2 to 5 minutes.
3 times per week, under supervision
Program length of 12 weeks at least
Progression Increase the length of each training session by 1-2 weeks until it is 50 minutes. Modify the grade or speed of the exercise prescription to keep the walking bouts within 5 to 10 minutes as individuals can walk for longer than 10 minutes without reaching the prescribed claudication level.
Maintenance lifetime upkeep at least twice a week
Based on data that is currently available. Each patient should receive an individualized exercise prescription based on their tolerance. Six-minute walk test is denoted by 6-MWT.
What can I do to alleviate this condition at home?
There are various things you can take to lessen the intensity of the discomfort and the frequency of your intermittent claudication. Regularly moving around. Intermittent claudication can be relieved by performing something as basic as walking (for at least 30 minutes, three or more times each week). The fact that intermittent claudication makes walking painful and frequently makes you not want to walk is one of the main issues. Inactivity exacerbates claudication, starting a vicious cycle of increasing discomfort and difficulty walking.
Achieve and/or keep a healthy weight. Obesity can make PAD and associated symptoms, such as intermittent claudication, worse.
Adopt a balanced diet. Changing your diet can assist with issues including high cholesterol, high blood pressure, and diabetes (perhaps delaying or even avoiding this condition’s development). Put an end to your cigarette use. This covers smoke-producing goods like cigarettes, cigars, pipes, vaping, and chewing and snuff tobacco.
Take the prescribed prescription. That entails following your doctor’s advice and taking your medication as directed, not just when you experience symptoms. Your risk of serious illnesses like stroke might significantly increase if you abruptly stop taking specific drugs, particularly blood thinners.
Take care of your mental health and stress. All aspects of your body, particularly your heart and circulatory systems, can be significantly impacted by your mental health.
How can this symptom be prevented?
Numerous of the things that you may do at home to aid with this issue and prevent intermittent claudication are described above. It may be feasible to delay its onset even if it can’t always be entirely avoided. This is crucial because intermittent claudication is an indication of PAD, which greatly raises your risk of developing heart disease, a heart attack, a stroke, and other conditions.
The following are the most crucial preventive measures:
Stop using tobacco products, or refrain from using them altogether.
Only consume alcohol in moderation. One drink per day (no more than seven drinks per week) for women and two drinks per day (no more than 14 drinks per week) for males is considered moderate
alcohol consumption.
Maintain a healthy weight.
Eat a healthy diet.
Exercise regularly.
Manage your stress and mental well-being.
When should Intermittent Claudication be treated by a Doctor?
Early identification and treatment of intermittent claudication are crucial to preventing or significantly reducing major issues in the future. Several significantly more dangerous illnesses have symptoms with intermittent claudication. These include popliteal artery entrapment syndrome (PAES), deep vein thrombosis (DVT), and chronic compartment syndrome.
Your healthcare professional is the greatest resource to describe potentially dangerous symptoms, including those necessitating emergency care if you already know you have intermittent claudication.
They are the most qualified to provide advice that is tailored specifically to your requirements and situations. The following are general indications that you should consult a doctor:
signs of severe blood flow issues in a limb, particularly in the feet and legs. You should seek immediate medical attention if any of these symptoms occur, such as if one of your limbs becomes notably paler, colder, or numb. In rare circumstances, this is a severe sign of obstructed blood flow and can lead to amputation.
Delayed healing wounds or new sores and ulcers.
Any indications of infection, particularly those near a wound or sore. These include warmth, discomfort, swelling, and redness.
Shortness of breath or chest pain that occur concurrently with or shortly after leg pain.
Pain that doesn’t go away when you take a break to relax
Pain that suddenly becomes intense or shifts from its typical site.
Overview
Claudication is pain that develops when muscles don’t receive enough blood during exercise. Depending on how severe the illness is, this pain typically hits the legs after a specific period and a given rate of walking. Because the discomfort is typically not consistent, the condition is also known as intermittent claudication. It starts when you’re moving about and ends when you’re relaxing. But when claudication becomes worse, the pain could even happen while you’re sleeping.
Technically speaking, claudication is a symptom of a condition, most often peripheral artery disease, which is marked by a narrowing of the arteries in the limbs, hence reducing blood flow.
The main goals of treatments are to minimize the risks of vascular disease, lessen pain, improve mobility, and stop tissue damage.
FAQs
Can intermittent claudication occur while at rest?
Pain in the calf that is caused by exercise and relieved by rest is known as intermittent claudication. Less frequently, the thigh and buttocks are also affected. The symptoms can be moderate or severe in severity. Muscle ischemia during exercise brought on by arterial flow restriction results in intermittent claudication.
What makes intermittent claudication more painful?
Lack of movement makes claudication worse, resulting in a vicious cycle of increasing discomfort and difficulty walking. Get to a healthy weight and/or keep it there. Weight gain can exacerbate PAD and its symptoms, including intermittent claudication.
Is intermittent claudication bilateral or unilateral?
Claudication describes an uncomfortable, exhausted, cramp-like, and occasionally burning sensation mostly in the legs unilaterally or bilaterally. It often happens with activity and walking a specific distance for a specific length of time and goes away with rest. This disorder is known medically as intermittent claudication.
Is recurrent claudication considered a disability?
Neurogenic claudication refers to a condition that affects the neurological system and results in weakness or excruciating cramping in the legs. You can be eligible for disability compensation provided you can show the required medical records.
Which drug is prescribed for intermittent claudication?
Risk-factor reduction, exercise, and antiplatelet therapy are among the methods used to treat IC with the goals of easing symptoms and slowing the progression of atherosclerosis. Only cilostazol and pentoxifylline have FDA-approved labeling for use in treating IC.