Inter-Scalene Triangle
Table of Contents
Introduction
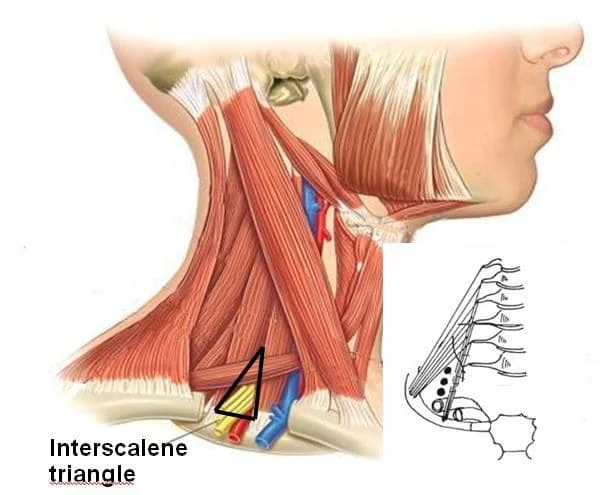
The region of the neck known as the Inter-scalene triangle, or scalene triangle, is crucial to the operation of the upper limbs. The brachial plexus roots and the third segment of the subclavian artery both pass across it.
The peak of the paired inter-scalene triangle points superiorly in the direction of the base of the skull. Surgical decompression may be required if the issue significantly impairs daily activities or compromises the upper limb.
The triangle’s borders are as follows:
- The posterior border of the scalenus anterior muscle is located anteriorly.
- The anterior border of the scalenus medius muscle is located posteriorly.
- The first rib’s superior aspect is inferior.
Structure
The peak of the paired inter-scalene triangle points superiorly in the direction of the base of the skull. It is situated at the neck’s root. The horizontal base of the triangle is formed by the superior edge of the first rib. The anterior covering of the scalene triangle, or the triangle’s “roof,” is made up of the prevertebral fascia of the neck, which extends from the body of the T4 vertebra to the base of the skull.
The little aperture between the scalenus anterior and medius muscles admits just the roots of the brachial plexus and an equivalent part of the subclavian artery.
It articulates with the manubrium sternum on the medial half and the T1 vertebra’s body on the head. Its upper side has a subclavian artery groove and the scalene tubercle, which is connected to the scalenus anterior.
The anterior scalene, a narrow tendon that arises at the first rib and is connected to the scalene tubercle on its top side, is derived from the transverse processes of the anterior tubercles of C3 to C6. The quadrangular space between the first rib’s neck and subclavian groove is where the middle scalene enters the rib. It comes from the transverse processes of the posterior tubercles of C3 to C7, as well as the lateral parts of C1 and C2 (atlas and axes).
Function
These muscles facilitate first rib elevation, which lessens the effort needed for breathing, as well as postural stability, neck flexion, and rotation.
Embryology
The anterior and middle scalene muscles, as well as the neck muscles, originate from the embryonic mesoderm. They next create the sclerotome and dermomyotome, the latter of which gives rise to the body wall muscles.
Blood Supply and Lymphatics
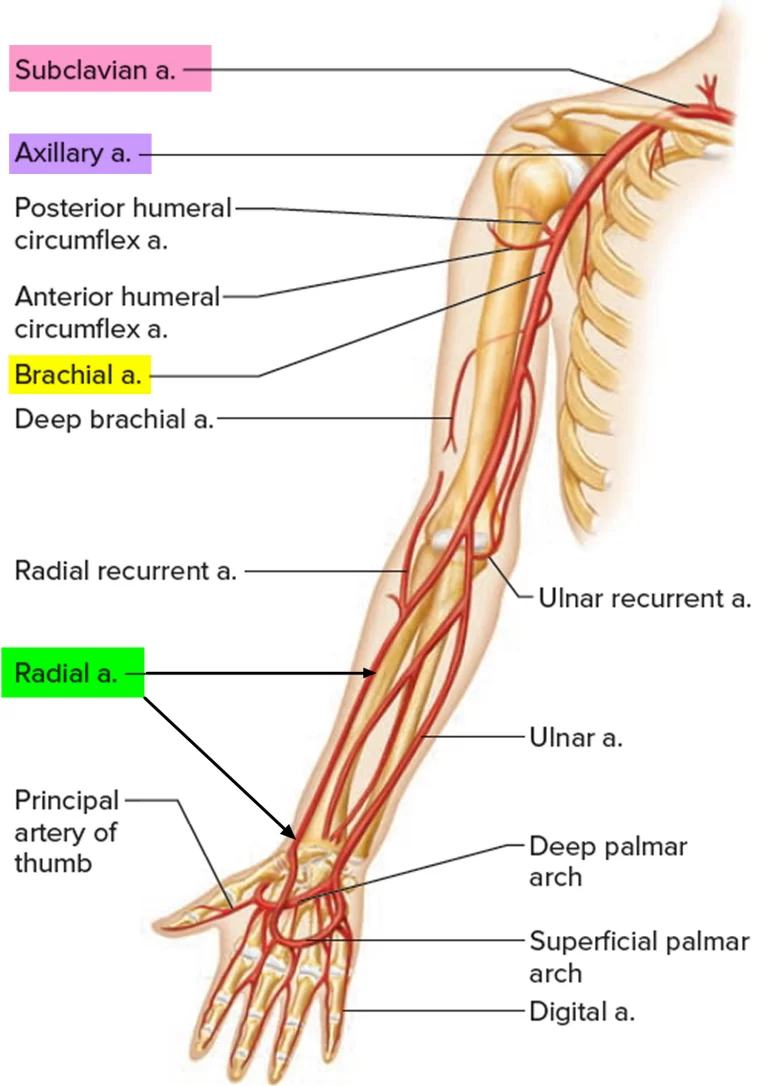
The subclavian artery passes right through the triangle the brachial plexus forms. It originates on the right side of the brachiocephalic artery and on the left side of the aortic arch. Compression of these vascular structures can lead to vascular dysfunction, weakness, and numbness.
Nerves
The upper part of the inter-scalene triangle contains the anterior rami of the third through fifth cervical spinal neurons. The base of the triangle is where the brachial plexus is situated. Injuries to this plexus can result in significant reductions in quality of life.
The brachial plexus divisions extend distally with regard to the axillary artery after crossing behind the collarbone. Eventually, they terminate in distinct branches that supply the cutaneous and muscular innervation of the upper limbs.
The phrenic nerve is comparable to the subclavian vein in that, despite not being inside the inter scalene triangle, it is easily compromised by disorders that affect the triangle because of its close closeness to it. Breathing-related diaphragmatic muscles are controlled by the phrenic nerve.
Another nerve that is related to the inter-scalene triangle but is not a component of it is the long thoracic nerve. This nerve, which enters the subcutaneous layer at the first and second ribs, innervates the serratus anterior muscle.
Muscles
The anterior scalene, a narrow tendon that arises at the first rib and is connected to the scalene tubercle on its top side, is derived from the transverse processes of the anterior tubercles of C3 to C6. The quadrangular space between the first rib’s neck and subclavian groove is where the middle scalene enters the rib. It comes from the transverse processes of the posterior tubercles of C3 to C7, as well as the lateral parts of C1 and C2 (atlas and axes). These muscles facilitate first rib elevation, neck flexion and rotation, and postural stability, all of which lessen the effort needed for breathing.
Anatomical Variantions
The anterior scalene muscle can originate from a variety of locations, including C2 to C6, C3 to C5, and the second or third rib, among other possible locations. In contrast to the anterior scalene, the middle scalene can arise from C1 (the atlas) and can also be implanted into the second rib. The anterior scalene in particular may enlarge in certain individuals, which may eventually result in changes to the subclavian artery aneurysmal. This is an important consideration while doing surgery in this area. Beyond the muscle-related variances, there are further variations.
A healed fracture, rib fusion, or an odd location are examples of structural abnormalities that can limit the amount of space that is accessible in the first rib. Any alteration could make the structures harder to see and call for more non-surgical or surgical interventions.
Surgical Considerations
Splenectomy
You can also administer both treatments at the same time for the best results. Either way, their purpose is to increase the amount of access that the remaining upper extremities’ nerves and vasculature have to them. This procedure can be performed using either a trans-axillary or a supraclavicular approach, and the data that are currently available do not indicate any discernible differences in the safety or complication rates between the two techniques. In lieu of surgery, scallopine muscle injections are another conservative method for reducing pain.
Clinical Importance
Interscalene Block
After surgery, nerve blocks can be used to reduce the patient’s pain while they heal. One often-cited example of such a nerve block is the inter-scalene nerve block, which is notably used in various upper extremity injuries. This nerve block can be administered either before or after shoulder surgery to anesthetize the axillary, musculocutaneous, suprascapular, lateral pectoral, and part of the cervical plexus.
The needle is inserted mediolaterally to reduce the possibility of damaging important nearby neurological structures, such as the dorsal scapular and long thoracic nerves. Even though interscalene nerve blocks have a 0.4% chance of causing long-term issues, any impairment has a major impact on a patient’s quality of life because upper limb function is so vital to daily functioning.
Thoracic Outlet Syndrome
Thoracic outlet syndrome (TOS) is a common syndrome that occurs 3–8 times per 1000 people and is typically caused by aberrant regional anatomy or injury to adjacent systems.
This condition may be caused by a variety of reasons, including additional scalene muscles, congenital malformations of the first rib, cervical ribs, fibrous bands, aneurysms, and trauma.
Thoracic outlet syndrome has historically been seen as being difficult to diagnose because of these variables as well as the lack of a specific clinical diagnostic tool. The clinical history may include paraesthesia, weakness, or heaviness in the affected upper limb in addition to pain in the neck, occiput, chest, shoulder, and upper limbs. Thoracic outlet syndrome is known for lacking a clear clinical presentation.
The compression of the subclavian artery is more indicative of TOS than the compression of the subclavian vein since vein compression can occur in people without TOS. This condition is diagnosed using both imaging and clinical approaches.
Diagnostic procedures that may be used to investigate suspected thoracic outlet syndrome include ultrasonography, chest radiography, CT angiography, magnetic resonance angiography, specialized venography or arteriography, nerve conduction tests, or needle electromyography. Different criteria could be used to identify TOS.
FAQs
What is the longest side of a scalene triangle?
the base of the hypotenuse
The hypotenuse, or h, is the side of the triangle that is opposite the right angle. Of the three sides of a right triangle, it is the longest.A unique scalene triangle is what?
Describe the Scalene Triangle. A scalene triangle is a triangle with three different lengths for each side and three different measurements for each angle. But the total of all interior angles is always equal to one hundred and sixty degrees.
What is the distance between the inter-scalene?
the posterior side by the anterior portion of the middle scalene muscle, and the inferior side by the superior aspect of the first rib.
Which triangle’s sides aren’t equal?
the Scalene Triangle
A triangle with three distinct lengths on each side is called a scalene triangle. The sides and angles of a scalene triangle are not congruent since there are no equal side lengths or equal angle measurements.What five characteristics define a scalene triangle?
Scalene Triangle’s characteristics
A scalene triangle has three unequal sides. The Scalene triangle has no angles that are equal to one another. A scalene triangle’s interior angles can be acute, obtuse, or right, but sometimes they are 180 degrees.Is the interscalene block shallow or deep?
The space between the skin and the brachial plexus block is frequently less than 1 cm and infrequently deeper than 2 cm, indicating how superficial the brachial plexus is at this site.
What is Interscalene’s level?
The C5 and C6 nerve roots are located in the inter-scalene groove between the middle and anterior scalene muscles at the level of the sixth cervical vertebra, or roughly at the level of the cricoid cartilage, as the block’s name implies.
What elements make up a scalene triangle?
A scalene triangle has three angles with varying measures and three sides, each with a distinct length. It also complies with the triangle’s angle sum property. A scalene triangle lacks symmetry because the angles are uneven and the side lengths are not equal.
Which three kinds of scalene triangles are there?
Three categories can be applied to a scalene triangle:
Scalene triangle with an acute angle:
Inside the triangle is the circumcenter.
Scalene triangle with an obtuse angle: The circumcenter is outside the triangle.
Scalene triangle with a right angle: The hypotenuse’s midpoint is the circumcenter.What is the Infratrochlear triangle’s perimeter?
triangle infratrochlear
The trochlear nerve medially, the ophthalmic division of the trigeminal nerve laterally, and a line connecting the posterior limit of the medial and lateral boundaries posteriorly define the infra-trochlear triangle.Which landmarks are interscalene?
The external jugular vein, the clavicle, and the clavicular head of the sternocleidomastoid are the three main landmarks needed for the block. The cricoid cartilage is another useful marker.
What is the syndrome of the scalene triangle?
Definition. Pain, numbness, tingling, alterations in sensation, and weakening in the muscles of the upper extremities could be the clinical presentation.
What limits do the Interscalene spaces have?
Between the two muscles’ insertion sites, the inter-scalene triangle is bounded on the anterior side by the posterior edge of the anterior scalene muscle, on the posterior side by the anterior edge of the middle scalene muscle, and on the inferior side by the superior aspect of the first rib.
Regarding thoracic outlet syndrome, what are the triangles?
The term “thoracic outlet syndrome” (TOS), which describes a group of diseases that constrict the neurovasculature exiting the thoracic outlet, was first used in 1956. The three areas where TOS typically arises are the subcoracoid space, the costoclavicular region, and the scalene triangle.
The Interscalene triangle: what is it?
The region of the neck known as the inter scalene triangle, or scalene triangle, is crucial to the operation of the upper limbs.
References
- Physiotherapist, N. P. (2023, December 13). Inter-scalene Triangle – Structure, Function, Border. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/inter-scalene-triangle/
- Georgakopoulos, B., & Lasrado, S. (2022, November 9). Anatomy, Head, and Neck: Inter-scalene Triangle. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK544222/


One Comment