Hip Mobilization exercises
Table of Contents
What is Mobilization for the Hip joint?
- Hip Mobilization is a passive, skilled, manual therapy program that appeals to Hip joints in conjunction with the soft tissue at various speeds and amplitudes utilizing a physiological or accessory movement for therapeutic purposes
- small amplitude force executes at a fast velocity, and a large amplitude force executes at to slow velocity
- it is a manual technique that associates appealing to the target forces on a painful, stiff or negotiated jointly in relation to enhancing its overall function. Which is not convenient in all situations, joint mobilizations help enhance the range of motion, reduce pain, and minimize stiffness.
- Hip Joint mobilization is a hands-on treatment that is repeatedly executed by physiotherapists healthcare professionals who specialize in rehabilitation for movement disorders and chiropractors, health professionals treating conditions of the musculoskeletal system that include bones, muscles, and soft tissue, ligaments
Introduction of the hip

- The hip may be a ball and socket variety of synovial joints that attach the pelvic girdle to the lower limb. during this joint, the highest of the femur is cemented with the acetabulum of the pelvic (hip) bone.
- The hip may be a multiaxial joint and allows a wide range of motion; flexion, extension, abduction, adduction, external rotation, internal rotation, and circumduction. however, the hip sacrifices mobility for stability because it is designed for weight bearing. the full weight of the upper body is conveyed through the hip joint to the lower limbs during standing. The hip is the most balanced joint in the human body.
Articular surfaces of the hip joint
- The hip is cemented within the middle of the ellipsoid head of the femur and the hemispherical concavity of the acetabulum is placed on the lateral aspect of the hip bone. The femoral head is roofed with articular (hyaline) cartilage with the exception of a rough midway depression, the fovea capitis, which can be a surface of cemented for the ligament of the femoral head termed as ligamentum teres capitis femoris.
- The acetabulum is hammered by the fusion of the ilium, ischium, and pubic bones. It plays an enormous role in the stability of the hip joint as it almost entirely surrounds the head of the femur. The acetabulum bears a prominent semilunar region termed the lunate surface that’s covered by articular cartilage. The lunate surface structure is an incomplete ring that lived in the superior and lateral aspects of the acetabulum; absent its inferior segment. This surface is vast anterosuperiorly where it supports most of the trouble during standing. The deficient inferior aspect of the acetabulum configurations the acetabular notch.
- The deep central nonarticular floor of the acetabulum is termed the acetabular fossa. This area is deficient in cartilage and is constant with the acetabular notch. It consists of loose tissue (fibroelastic fat pad) which is covered by a synovial membrane. fabricated to the margin of the acetabulum could also be a fibrocartilaginous collar called the acetabular labrum. This structure deepens the acetabulum by raising the rim of the acetabulum slightly, thereby elevating the acetabular articular area by about 10%. Inferiorly, the acetabular labrum continues because of the transverse acetabular ligament, bridging the acetabular notch and remodeling the notch into a foramen.
- The superior aspect of the acetabulum which of the femoral head supports the best pressure. These areas usually have the thickest articular cartilage. The concave acetabulum and thus the rounded femoral head of the hip joint, in addition to the anatomical connection joining the femur and therefore the pelvis, particularly within the upright position, make this joint incongruent. The articular surfaces are most congruent when the hip is in a partially flexed and abducted position.
The joint capsule of the hip joint
- The hip is inserted by a robust fibrous capsule and lined internally by a synovial membrane. The external fibrous layer of the capsule is hooked to the acetabulum proximally, almost the margin of the acetabular rim, and to the transverse acetabular ligament. From its acetabular connection, the fibrous layer extends laterally to its distal connection on the proximal femur. It connects to the intertrochanteric line anteriorly, the underside of the femoral neck superiorly, about 1cm superomedial to the intertrochanteric crest posteriorly, and on the femoral neck near the lesser trochanter inferiorly. it’s value remark that a part of the femoral neck is intracapsular and part is extracapsular.
- The capsule of the hip is markedly thicker anterosuperiorly, which is the world of maximal stress, particularly within the upright position when the hip is extended. Posteroinferiorly, the capsule is corresponding slim and insecurely cemented. The capsule has two major groups of fibers, longitudinal fibers, and circular fibers. The external longitudinal fibers of the fibrous capsule usually move in a spiral manner from the hip bone to the proximal femur. The deeper circular fibers form a collar around the femoral neck, and thus the zona orbicularis (orbicular zone or annular ligament), and have no bony attachments. The capsule of the hip is reinforced inferiorly by the pubofemoral ligament and posteriorly by the ischiofemoral ligament.
ligaments of the hip joint

- The ligaments of the hip joint can be classified into two groups; capsular ligaments and intracapsular ligaments. the Capsular ligaments are the underlying ligaments of the joint capsule. There are three capsular ligaments that play a major role in conserving the integrity of the joint during various movements: iliofemoral, pubofemoral, and ischiofemoral ligaments. The intracapsular ligaments of the hip joint originate inside the capsule and involve the transverse ligament of the acetabulum and the ligament of the head of the femur.
- The iliofemoral ligament is a thick triangular ligament that stays on the anterior and superior aspects of the hip joint, and blends with the joint capsule. Its proximal association is between the anterior inferior iliac spine and the acetabular rim. Distally, it connects to the intertrochanteric line. The central part of this ligament is thinner and co-relates with its outer bands, offering the ligament an inverted Y-shape. It is the strongest ligament in the body and functions to inhibit hyperextension of the hip joint when standing.
- During extension, this ligament tightens, compression the capsule, and secures the femoral head tightly in the acetabulum. This movement limits the extension of the hip joint above the vertical position to between 10o to 20o
Pubofemoral ligament
- The pubofemoral ligament is situated anteroinferior and builds up the anterior and inferior aspects of the joint capsule. It originates from the iliopubic ramus, the superior pubic ramus, and the obturator crest of the pubic bone. It escapes laterally and inferiorly to the lower aspect of the intertrochanteric line, corresponding with the fibrous layer of the joint capsule and the medial band of the iliofemoral ligament.
- The thinnest area of the joint capsule is among the medial fibers of the iliofemoral and the pubofemoral ligaments where there is a circular aperture. The tendon of the iliopsoas muscle looms over this area. among the muscle tendon and the capsule is the iliopectineal (psoas) bursa which reveals the hip joint cavity. The pubofemoral ligament prevents extreme abduction of the hip joint by tightening during extension and abduction movements
the ischiofemoral ligament
- The ischiofemoral ligament is the most sluggish of all three capsular ligaments. It is located posteriorly and strengthens the posterior aspect of the joint capsule. It is connected medially to the ischial bone down to the acetabulum. It runs superolateral around the capsule and posterior to the femoral neck to connect to the base of the greater trochanter, deep to the iliofemoral ligament. Some of the deeper fibers of the ischiofemoral ligament correspond with the zona orbicularis.
Transverse ligament of the acetabulum
- The transverse ligament of the acetabulum is a strong flat ligament that links the acetabular notch and initiates the acetabular foramen through which neurovascular structures enter the hip joint. It completes the inferior insufficiency of the acetabular rim and is continuous peripherally with the acetabular labrum.
Ligament of the head of the femur” ligamentum teres capitis femoris”
- This ligament is a flattened triangular band of connective tissue that has no significant donation to the strength and stability of the hip joint. Its apex connects to the fovea capitis while its base connects to the acetabular notch and the transverse acetabular ligament. It is enveloped by a synovial membrane and brings a small branch of the obturator artery, the artery to the head of the femur, which donates to the blood supply of the femoral head.
Innervation
- The hip joint is reinforced by the articular branches of multiple nerves that loom from the lumbosacral plexus (L2-S1). The nerve supply to a specific region of the joint typically corresponds to the reinforcement of the muscle that crosses it:
- The femoral nerve reinforces the anterior aspect
- The obturator nerve contributes to the inferior aspect
- The superior gluteal nerve contributes to the superior aspect
- The nerve to the quadratus femoris reinforces the posterior aspect.
- It is important to note that pain sensations from the vertebral column can be attributed to the hip joint, while primary hip pain may be attributed to the knee as they share related innervation.
Blood supply of the hip joint
- The blood supply of the hip joint starts from the medial and lateral circumflex femoral arteries and their branches of the deep artery of the thigh, which is the obturator artery, and the superior and inferior gluteal arteries. in conjunction with this, these arteries form a periarticular anastomosis surrounding the hip joint. the periarticular anastomotic pattern allows elevating to the retinacular arteries which transform the greatest volume of blood to the head and neck of the femur. Extraordinary, the obturator artery gives elevates to the artery of the head of the femur within the ligament of the head of the femur
Movements of the hip joint
- Being a ball-and-socket joint, the hip joint grants movements in three degrees of freedom: flexion, extension, abduction, adduction, external rotation, internal rotation, and circumduction.
- Flexion of the hip joint ties the thigh towards the trunk. When the knee joint is flexed, the hip joint can be fully flexed with the thigh coming in contact with the anterior abdominal wall. The range of movement during passive flexion is about 120degree and arrives around 145degree during active flexion. Hip flexion is narrowed by the tension in the hamstrings when the knee is extended.
- The extension of the hip joint runs away from the thigh far from the trunk. Extension of the joint across the vertical is narrowed to about 30 degrees by the tension of the capsular ligaments and the shape of the articular surfaces.
- Abduction and adduction of the hip joint start in the coronal plane and have a free range of movement of about 45 degrees. With the hip flexed, the range of abduction is far greater than when the hip is extended. Abduction of the hip joint is narrowed by tightness in the adductor muscles and the pubofemoral ligaments. Hip flexion also compose adduction easier. Adduction, on the other hand, is limited by the contralateral limb, the tension in the abductor’s muscles, the lateral part of the iliofemoral ligament, and the fascia lata of the thigh.
- Internal and external rotation of the hip joint demonstrates in the horizontal plane the mechanical axis of the femur on behalf of the long axis of the femoral shaft. The mechanical axis runs in distinction from the head of the femur to the intercondylar notch of the distal femur. During internal rotation, the femoral shaft runs anteriorly, causing the toes to point medially. The rival action starts in the external rotation where the femoral shaft moves posteriorly, responsible for the toes to point away from the midline. External rotation is much more savior and more powerful than internal rotation. For example, the range of internal rotation with the hip extended is about 35 degrees while external rotation is about 45degrees. Rotation at the hip joint is usually much savior with hip flexion rather than an extension. Tightness in the lateral rotators and the ischiofemoral ligament limits internal rotation of the hip joint. in opposition, external rotation is restricted by tightness in the medial rotators of the thigh and the iliofemoral and pubofemoral ligaments.
muscle of the hip joint
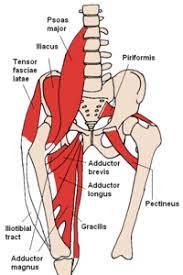
- Flexion: Psoas major, iliacus, and rectus femoris; assisted by pectineus, tensor fasciae latae, and sartorius
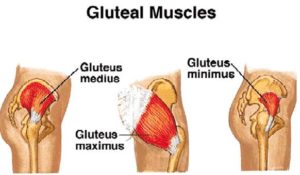
- Extension: Gluteus maximus, biceps femoris, semitendinosus,
- the semimembranosus and adductor Magnus
- Abduction: Glutei medius and minimus; approved by tensor fasciae latae, piriformis, and sartorius
- Adduction :Adductors longus, brevis and magnus, gracilis; assisted by pectineus, quadratus femoris and the inferior fibres of gluteus maximus
- Internal rotation: Gluteus minimus and gluteus medius; assisted by tensor fasciae latae and most adductor muscles
- External rotation :Gluteus maximus, obturator internus, superior and inferior gemelli, quadratus femoris, piriformis; assisted by obturator externus and sartorius
The condition required mobilization of the hip joint
- coxa vara
- coxa valga
- hip dislocation
- irritable hip syndrome
- crush syndrome
- myositis ossificans
The surgical procedure required mobilization of the hip joint
- hip replacement arthroplasty
- excisional arthroplasty
Goals for hip mobilization
pain, muscle guarding, and spasm
- painful joint, reflex, muscle guarding, and spasm can be mediated with gentle joint play techniques to stimulate neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and distraction movement are acclimated to stimulate mechano receptors which will inhibit the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- small amplitude distraction or gliding movement of the joint is acclimated cause synovia motion, which may be a vehicle for carrying nutrients to avascular portions of the articular cartilage
- gentle joint play procedures help to take care of nutrient exchange and prevent the painful and degenerating effects of statis when the joint is swollen or painful, and may not go through a range of motion
- when adapted to treat pain, muscle spasms, and muscle guarding these techniques shouldn’t place stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility is often mediated with progressively vigorous joint play stretching procedure to elongate hypermobile capsular and ligamentous connective tissue
- sustained or distraction stretch forces are applied to distend the shortened tissue mechanically
Positional faults/subluxations
- A faulty position of 1 bony partner with regard to its opposing surface may outcome in limited motion or pain
- positional faults can initiate traumatic injury, after periods of immobility, muscle imbalance
- the faulty position could also be preserved by maladapted neuromuscular control across the joint
- during attempting a lively range of motion, faulty tracking of the joint surface leads to pain or limited motions
Progressive limitations
- diseases that progressively restrict movement are often treated with joint play techniques to maintain available motion or lessen progressive mechanical restrictions
- the patient’s response manner the dosage of distraction or glide to treatment and therefore the state of the disease
Functional immobility
- when the patient can’t functionally move a joint for an extended period of time
- the joints are often mediated with nonstretch gliding or distraction procedure to maintain available joint play and prevent the degenerating and restricting effect of immobility
Grades of mobilization of the hip joint
Non-thrust oscillation techniques
- the oscillation could also be performed using physiological movement
- grade 1:small amplitude rhythmic oscillation is put at the start of the range, rapid oscillation like manual vibration
- grade 2:large amplitude rhythmic oscillation is completed within range, not reach the limit, perform 2 or 3 seconds for 1 to 2 minutes
- grade3:large amplitude rhythmic oscillation is initiated up to an available range of motion, stress into tissue resistance, perform 2 or 3 seconds for 1 to 2 minutes
- grade4:small amplitude rhythmic oscillation is executed at the available range of motion, the strain in tissue resistance, rapid oscillation like manual vibration
- grade 1 and a couple of are used to treat joint limitation of movement by pain or muscle guarding
- grade3 and 4 are useful for stretch maneuver
Nonthrust sustained joint play techniques
- This system interprets only joint play procedures that distribute (distract) or glide the joint surface
- grade 1(loosen): small amplitude distraction is applied when no stress is placed on the capsule, it equalizes cohesive force, muscle tension, and air pressure acting on joint
- grade2(tighten): limitless distraction or glide is applied to tighten the tissue surrounding the hip
- grade3(stretch): a distraction or glide is put with an amplitude large enough to place a stretch on the joint capsule surrounding the periarticular structure
- grade 1 distraction is given with all glide movements
- apply periodic distraction for 7 to 10 seconds with some seconds of rest in between several cycles
- grade 2 distraction is useful to determine the sensitivity of the joint, once the joint reaction is understood treatment dosage increases and decreases
- gentle grade 2 distraction apply periodically wont to prevent pain and maintain joint play when ROM is not allowed
- grade 3 distractions or glides are needed to stretch joint structure, elevate joint play motion
- for limited joints apply a minimum of 6 seconds of stretch force followed by partial release (grade 1 or 2)
- reps:3 to 4-second intervals
Mobilization of the hip joint
- the concave acetabulum obtains the convex femoral head
- patient position: hip flexion 30 degrees, abduction 30 degrees, and slight external rotation
- stabilization: stabilize the pelvis to the treatment table with belts
- treatment plane: acetabulum
hip distraction caudal glide

- patient position: supine with the hip in a relaxed position and the knee extended
therapist position and hand placement
- stand at the end of the treatment table like the patient’s sole foot facing the therapist’s face
- place a belt around your trunk and then cross the strap over the patient’s foot and around the ankle
- place your hand’s right side of the malleoli under the belt
- the belt permits you to use your body weight to apply mobilizing force
mobilizing force
- apply long-axis traction by snatching on the legs as you lean backward
An alternate technique for caudal glide
- patient supine with hip and knee flexed and footed resting on the table
- envelope your hands surround the epicondyles of the femur and distal thigh
- do not compress the patella
- the force comes from your hand and is applied in a caudal direction as you lean backward
hip posterior glide

- patient position: supine with hips slightly outside of the table
- the patient helps stabilize the pelvic and lumber spine by flexing the opposite hip and holding the thigh against the chest with the hands
- demonstrate, the hip to be mobilized is in resting position, progress to the end of the range
therapist position and hand placement
- stand on the bedside the patient’s left thigh
- place a belt surrounding your shoulder and under the patient’s thigh to need for hold the weight of the lower extremity
- place your left hand under the belt and left thigh
- place your right hand on the anterior surface of the right side thigh
mobilizing force
- place your elbow extended and flex your knees, apply force with your proximal hand in a posterior direction
- hip posterior glide is used to increase flexion and internal rotation
Hip anterior glide

- patient position: prone with trunk relaxed on the treatment table and hips over the edge of the treatment table
- the opposite foot is on the floor
therapist position and hand placement
- stand the bedside the patient’s left thigh
- place a belt around your shoulder
- the patient’s thigh use to support the weight of the leg
- place your right hand posteriorly on the right side thigh just below the buttock
mobilizing force
- place your elbow extended and flex your knees
- apply the force with your proximal hand in an anterior direction
alternate position
- position the patient side-lying with the thigh comfortably flexed and supported by pillows
- stand backside to the patient and stabilize the pelvis beyond the anterior superior iliac spine with your cranial hand
- thrust against the posterior aspect of the greater trochanter in an anterior direction with your right hand
Precaution for mobilization of the hip joint
- Never cross your legs or ankles on sitting, standing, or lying down
- Avoid bending your operated leg greater than 90 degrees
- When sitting or standing from a chair, bed, or toilet you must assure that extend your operated leg in front of you.
- Do not stand when dressing, you can either sit at the edge of your bed if it is stable or use a chair
- Never bend over the trunk, raise or cross your legs when dressing
- Use an aid when donning shoes (a reacher or a long-handled shoehorn) or socks
- When undressing ensure you remove clothes from the surgery side last-ever sit for too long in the same position, you can change position every 30 minutes interval
- Always assure your feet are 6 inches (15cm) apart from each other
- Do not cross your legs
- Avoid rocking chairs, cushion chairs, stools, or sofas. Sit in a rigid chair with a straight back and armrests
- Avoid sitting on chairs that are too low, use a pillow if necessary use a special tub seat for sitting in the shower
- Use a rubber mat on the tub or shower floor. assure to keep the bathroom floor clean and dry for preventing slipping
- Do not ever bend, squat, or reach for anything while taking shower. Use a shower sponge with a long handle and have someone wash the part of your body that is hard for you to reach.
- assure you use a raised toilet seat. It will be difficult to get up safely if the seat is too low.
- When climbing up, step first with the unaffected leg (the side that was not operated on)
- When descending, step first with the operated leg.
- Do not sleep on the side of your operated hip or on your stomach. assure you put two pillows in between your thighs if you are sleeping on the other side
- assure you get into the car from street level, not from a curb or doorstep
- assure the car seat is not too much low, and use a pillow if necessary
- Don’t go for long car rides, stop get and walk about every 2 hours
- Ensure you use your crutches or walker until your doctor or physical therapist tells you it is OK to stop using them
- Do not lift up over the amount of weight your doctor or physical therapist advice you to lift on the operated hip
- Take small steps when turning.
- Avoid wearing slippers that can make you fall. Go slowly when walking on slippery and uneven surfaces
Hypermobility
- the joint of a patient with potential necrosis of the ligaments or capsules should not be mobilized with stretching techniques
Joint effusion
- the joint effusion due to trauma or disease
- rapid swelling of the joint usually indicates bleeding in the joint and may occur with diseases like hemophilia
- medical intervention is required for aspiration of the blood to minimize the necrotizing effect on the articular cartilage
- slow swelling for more than 4 hours usually indicates serious joint effusion or edema on the joint due to mild trauma irritation or disease such as arthritis
- do not stretch swollen joint with mobilization because the capsule is already stretched by being distended to accommodate the extra fluid
- the limitation of motion is from extra fluid and muscle response to pain, not from shortened fibers
- gentle oscillating motion that does not stress the capsule may help to block the transmission of a pain stimulus so it is not perceived and may help to improve fluid flow while maintaining available joint play
- if the patient’s response to gentle techniques is increased pain or joint irritability
- the techniques were applied too vigorously or should not be done with the current state of pathology
Inflamation
whenever inflamation is present, stretching increase pain and muscle guarding and result in greater tissue damage
gentle distraction motions may temporarily inhibit the pain response
FAQS
- When do we use joint mobilization for the hip?
The main aim of joint mobilization of the hip is to regain the normal joint movement that might have been compromised by damage or injury. Normal movement of the affected joint will be refilled faster if it is concession early in the treatment program. Also, mobilization is beneficial in cases when the range of motion is absent
- how much time is taken for mobilization after total hip arthroplasty?
after 1 or 2 months of POP, mobilization is given because the synovial formation of bone takes time to connect the bone
- Why is early mobilization important after an injury?
In patients with acute limb injuries, early mobilization decreases pain and swelling and improves functional outcomes correlated with cast immobilization
- How long do you do joint mobilization for the hip joint?
Typical treatment of a hip joint may add a series of three to six mobilizations carried on up to 30 seconds, with one to three oscillations or glide per second
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation is start within range, not reaching the limit of movement, apply the glide for 2 or 3 seconds for 1 to 2 minutes
that passes center way into the joint range of motion, attending any part of the range and yet not reaching the end range. This technique can be given to treat joint stiffness by accelerating the range of motion and joint pain