Discectomy
Table of Contents
What is the Discectomy procedure?
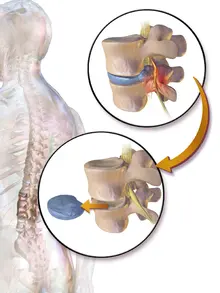
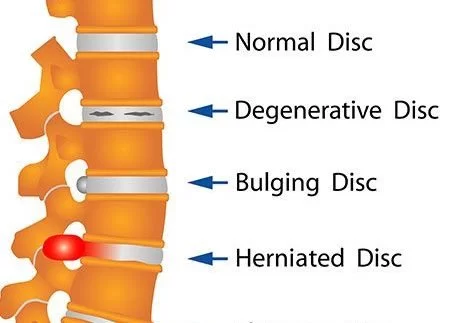
A Discectomy is a surgical procedure used to remove the injured portion of a disc from the spine that has its soft interior protruding through the outer, more robust layer. A herniated disc can aggravate or press on near nerves.
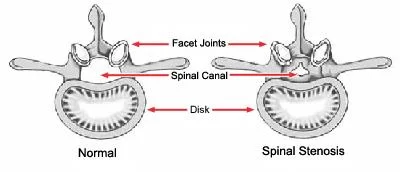
A series of bones known as vertebrae make up your backbone, also known as the spinal column. The spinal column contains your spinal cord. The bones help cover the cord from injury. Discs sit between each backbone to give cushioning and support. Large nerves called nerve roots originate from the spinal cord through foramina, with little openings in the bones. These nerve roots allow the body to send and receive impulses. The signals are transferred to and from your brain through the spinal cord.
On rare occasions, one of these discs’ exterior walls may weaken due to aging or damage. The disc’s soft, inner region protrudes when this occurs. A herniated or bulging disc is what this is. This bulging disc can press on the spinal cord and cause symptoms similar to pain, tingling, or weakness in a near part of the body.
The surgery entails removing a piece of an intervertebral disc, which stresses the spinal cord or radiating nerves and results in pain, weakness, or numbness. The procedure is less helpful for handling pain that is felt only in the back or neck. utmost people who have back pain or neck pain find relief with other treatments, similar to weight loss, arthritis medicine, or physical therapy.
If alternative nonsurgical therapies have failed or if symptoms worsen, a healthcare professional might advise a diskectomy. The process of a discectomy can be done in various ways. Numerous surgeons favor minimally invasive diskectomy, which involves few incisions and viewing of the process with a microscope or tiny video camera.
In 1934, Mixter and Barr used the L3 to sacrum method to introduce the first laminectomy for LDH. The hemilaminectomy procedure was first used in the 1970s.
Ross and Love published Love’s method, also known as the conventional open discectomy, in 1971. Advances have produced visualization enhancements to traditional discectomy techniques (e.g. microdiscectomy, an open discectomy using an external microscope generally done through a 1-inch or larger skin opening), or endoscopic discectomy( the scope passes internally and is generally done through a 2 mm skin opening or bigger, up to 12 mm). A laminotomy is frequently used in conjunction with a standard discectomy or a microdiscectomy to allow access to the intervertebral disc. Laminotomy means a significant amount of generally normal bone( the lamina) is removed from the backbone, allowing the surgeon to better see and pierce the area of disc herniation.
A 3 cm incision was described for microdiscectomy by Caspar and Williams in 1977.
The paraspinal method of treating extra-foraminal discs was first described by Wiltse and Spencer in 1988. During the same time frame, Kambin and Sampson published an extra-foraminal method using a totally endoscopic approach (FE).
Tubular retractor use was described in 1993 by Mayer and Brock. Foley and Smith performed a videotape-supported method using a tubular work canal(Micro-endoscopic discectomy MED) via a 2-cm incision embracing a trans-muscular approach without multifidus release from its insertion in 1997.
Conservative treatment approaches are also available, with oral medication and physical therapy serving as their foundations. The implicit effectiveness of these modalities is well established. Rigorous adherence to the objective association between the patient’s symptoms, physical examination findings, and individual imaging is essential to prognosticate the effectiveness of any planned surgery.
Different surgical strategies for LDH
Open.
Minimally Invasive Open Lumbar Discectomy( MIOLD).
Microlumbar discectomy( MLD).
Micro-endoscopic discectomy( MED).
Completely endoscopic( FE).
The latest surgical procedures only concentrate on lowering assess trauma to the multifidus and improving surgical vision; the fundamental idea of the surgery, which is to remove the nerve impingement, remains unchanged.
Why Discectomy procedure done?
A herniated disc, also known as a slipped, ruptured, bulging disc, or disc prolapse, puts pressure on a spinal nerve; this pressure is relieved by performing a discectomy. A herniated disc occurs when some of the softer material inside the disk pushes out through a crack in the external lining of the disc.
A healthcare provider might recommend a discectomy if:
Nerve weakness causes trouble standing or walking
A lumbar discectomy cannot always be used to relieve back pain. Additionally, not all herniated disc patients require lumbar discectomy. The doctor might advise surgery if you’ve tried alternate therapies but your symptoms are still severe. Other treatments to try first include physical therapy and anti-inflammatory medications.
critical lumbar discectomy is necessary in cases of cauda equina pattern and progressive or new motor deficiency. optional lumbar discectomy is indicated in cases of running radicular symptoms that correspond to radiographic confirmation of nerve root compression by a herniated disc in patients that have failed conservative treatment approaches.
Revision discectomy remains a feasible option should intermittent herniation occur, however, with the removal of further disc material and especially in the setting of large or repeated annular injury, the option to proceed with spinal fusion at the injured position may be a consideration. Before surgery, a high position of correspondence between a patient’s symptoms and pathology on glamorous resonance imaging must be confirmed to enhance the reasonable likelihood of a positive result.
Discuss with your surgeon the drawbacks and advantages of minimally invasive surgery versus open surgery. Minimally invasive surgery may lead to lower pain and brisk recovery. But not all surgical facilities are able to employ this method.
Pain travels into the buttocks, legs, arms, or chest and becomes too important to manage
What are the risks of Discectomy procedure?
Discectomy is considered safe. However, discectomy has a risk of complications much like any other type of surgery. Potential complications include:
- Bleeding
- Infection
- Leaking spinal fluid
- injury to the around the spine to blood vessels or nerves
- Blood clots
- Reaction to anesthetic agents
- Only short-term (temporary) relief & require another surgery
- Your risks might vary depending on your age and your general health. Talk with the healthcare provider about the risks that most apply to you.
How to prepare for Discectomy procedure?
Ask your healthcare provider how you should plan to prepare for your process. Ask if you should stop taking any drugs ahead of time, like blood thinners. Do not eat or drink after night or the night before the procedure.
Your provider may order other imaging tests of your spine, similar to an MRI.
Anesthesia:
Spinal or general anesthesia both had similar results.
Patients enduring general anesthesia( GA) demonstrated significant enhancement in VAS leg and back pain compared to LA in MED. LA minimizes costs and pitfalls.
Surgical aspects:
OT Safety Checklist.
Sterile theatre atmosphere.
Antibiotic prophylaxis is 30 minutes previous to incision.
Proper positioning of the Genupectoral assures free tummy, chest support, eyes protection, shoulders in 90 ° abduction, elbows in 90 ° flexion, and placing the spine in kyphosis to open up the inter-laminar space.
Localization and exposure- Through surface landmarks and fluoroscopic input.
You will probably need to avoid eating and drinking for a certain amount of time before surgery. However, you may need to adjust how important you take ahead of surgery If you take blood-thinning medicines. Specific instructions will be given by the healthcare provider.
How to perform Discectomy procedure?
Standard Discectomy( SD)
The patient is positioned prone on a dedicated table or a spine frame (Wilson or Allen Bow) following the administration of general anesthesia. Hip flexion is made possible by transverse pads at the iliac crest and chest that prevent pressure on the abdomen and lower central venous pressure. This increases interlaminar space. PaVisualisation of the interlaminar space is crucial, as is the surgical field’s removal of anatomized muscle tissue, appropriate retraction, and active electrocautery hemostasis.
The palpation of bony landmarks, including the sacrum and iliac ridges corresponding to the L4- L5 disc position, may guide the beginning point and trajectory of the surgical approach. After applying a sterile skin fix, fluoroscopic control and localization with a spinal needle confirm the target position. The midline is marked using a 3 to 4-cm longitudinal incision that is centered on the radiographic marker.
With a sharp scalpel, a skin incision is performed, and subcutaneous dissection with electrocautery reveals the lumbar fascia, which is incised just off the midline and palpable ipsilateral to the disc pathology treated. At the desired location, this fascia should span the interspinous distance. On a side fluoroscopic image, a radiographic marker may be utilized to validate the spinal location and cranially directed line parallel to the interspinous gap. The paraspinal musculature is elevated subperiosteally by electrocautery from the superior and inferior spinous processes to the laminar junction. Side dissection continues bluntly with a Cobb elevator as far indirectly as the facet joint taking care not to violate its capsule.
The surgeon now uses a curette to cut the ligamentum flavum loose from its attachment to the front portion of the lamina of the superior vertebra. To protect the dura below, a caudally oriented, angled Woodson elevator can also be placed anterior to the ligamentum. In order to retract the ligamentum using a Penfield elevator and see the departing nerve root and surrounding epidural fat, the ligamentum is also forcefully incised. The medium aspect of the inferior facet of the superior backbone may need resection to allow for acceptable exposure. Additionally, a Penfield or blunt probe is inserted into the neuroforamen to loosen the root and allow for its moderate retraction. With acceptable visualization of the intervertebral disc space, the discarding of fragmented or herniated tissue may also be carried out using a pituitary rongeur. However, a scalpel may be necessary to incise the annulus for access, If a portion of the herniation remains beneath the posterior longitudinal ligament. Care must be taken to probe the epidural space using a Woodson elevator in all directions for any fresh disc or ligamentous tissue.
also, it’s judicious to wash the disc space with saline via a bulb syringe to express any loose disc fractions that may have gone unvisualized. scrupulous hemostasis via bipolar electrocautery is achieved, and the wound is generously washed with saline. The skin closure is determined by the surgeon’s preference, and the fascial and subcutaneous layers are closed using absorbable sutures.
Minimally Invasive Surgery( MIS) Tubular Discectomy
The patient is placed and prepped as described over. A1.5 to 2.0 cm surgical incision is pronounced longitudinally,1.5 cm off midline on the affected side. A guide pin or K-wire is introduced through a cut made with a #15 scalpel and advanced underside fluoroscopy to ensure appropriate depth and docking to the lamina cranial to the afflicted spot. Once the beginning point and line are verified, the full skin incision is made, and a fascial incision is centered over the line. successional dilator retractors are placed to produce a working channel that may be anchored to the operating table. Magnifying surgical loupes or intra-operative bitsy are useful adjuncts to help in visualization. Utilizing instruments congruously designed for a tubular approach, the remainder of the procedure takes place as described over. scrupulous hemostasis is achieved, the tubular retractor system is removed, and the check of subcutaneous tissue and skin completes the case.
Micro-endoscopic Discectomy (MED)
The patient is prepared and positioned as previously mentioned. The anatomical space bounded by the traversing nerve root, exiting nerve root, & superior aspect of the caudal vertebra known as a Kambin triangle is reached at the targeting level utilizing a spinal needle beginning at a start position 1 to 2 cm off of midline same side to pathology. A 5 to 10 mm skin incision is created, and then an 18 mm operating canal is introduced under fluoroscopic guidance. This allows the endoscope to be inserted and used to view the disc space, traverse and exiting nerve roots, and pass tools. Targeted nerve roots may be released from compression utilizing endoscopic curettes, rongeurs, drills, and bipolar electrocautery when a cranial vertebra is laminotomized. Herniated disc material might thus be eliminated. A single little endoscopic incision is closed with a subcuticular suture.
Full endoscopic discectomy (FE)
The technique is lateral & trans-foraminal.
The entrance location is 20° to 30° off the midline and 12 to 14 cm away.
This approach is not advised for sequestrated intra-canal fragments.
What happens after the Discectomy procedure?
The surgery is generally an outpatient procedure. You can therefore leave for home today. After the procedure, you’ll probably need to stay for a few hours. For the drive home, make sure you have a designated driver.
You’ll receive instructions from your medical professional on how to use your back. You might need to restrict your bending and lifting. After the treatment, your doctor may advise you to wear a back brace for a brief period of time. utmost people can go back to work within a week or so. After surgery, you might require physical therapy to help strengthen your back.
After surgery, you are moved to a recovery room where the healthcare squad watches for complications from the surgery and anesthesia. You might be suitable to go home on the day of surgery. But a short hospital stay might be required particularly for those who have serious medical conditions.
Light conditioning can be continued at 2 weeks.
Routine conditioning can be continued at 6 weeks.
emphatic labor or contact sports can be continued after 12 weeks.
Rehabilitation plays an integral part. Rehabilitation preoperatively was performed in only 35 centers, postoperatively as an inpatient in all centers, and postoperatively as an outpatient in 82 centers. Enhanced Recovery Rehabilitation Surgery conceptions favor stylish clinical results.
Depending on the measure of lifting, walking, and sitting your job involves, you may be suitable to return to work in 2 to 6 weeks. However, you might have to stay 6 to 8 weeks before returning to work, If you have a job that includes heavy lifting or operating heavy machinery.
Your tiny incision may be dripping some fluid. This is normal. Tell your provider right down if there’s a large measure of drainage from the incision point. Call your healthcare professional if you get severe localized pain or a fever.
occasionally the procedure causes slightly further pain for a while. But you can take pain medications to ease the pain. generally, this goes down fast. Your pain should go lower than it was before your surgery.
Keep all of your doctor’s instructions to heart and be sure to show up for your follow-up appointments.
What are the complications of the Discectomy procedure?
Dehiscence or other wound infections happen at a rate of 1 to 2%, while wounds or deep infections happen at a rate of 2 to 3%. In 1 to 2% of cases, a direct intra-operative nerve root injury has been reported. In the literature, the incidence of inadvertent durotomy varies from 0 to 4%. Dehiscence or other wound infections happen at a rate of 1 to 2%, while wounds or deep infections happen at a rate of 2 to 3%. In 1 to 2% of cases, a direct intra-operative nerve root injury has been reported. In the literature, the incidence of inadvertent durotomy varies from 0 to 4%.
Following discectomy, the rate of LDH recurrence ranges from 1 to 25%, and the rate of intragenic dural rupture is close to 9%. Risk factors include smoking, strenuous labor, and male gender. An 8-year follow-up from the SPORT database suggests that patients with simultaneous retrolisthesis at L5-S1 appear to have the same long-term clinical results as patients without retrolisthesis. Since the risk of recurrence has been examined at a variety of follow-up intervals and by a number of outcome measures, such as recurring symptoms and reoperation, patient-specific considerations ought to guide a straightforward preoperative discussion.
After lumbar disc surgery, the patient could experience ongoing pain, which could be a symptom of failed back surgery syndrome.
Complications pertaining to lumbar discectomy can be enlisted as:
- Dural tear:
To expose the tear and do the initial repair with a 5/0 non-absorbable suture, place a Patti neurosurgery sponge and prolong the laminectomy edges. Use of biological glue.
Intraoperative dural damage is possible if there has been a history of epidural steroid injections within three months of the procedure.
Epidural bleeding and CSF leak are more likely to occur when the nerve is subjected to too much traction when the disc is exposed.
- Iatrogenic Neuropraxia:
Epidural bleeding:
compresses venous “lakes” with Patti sponge.
the application of surgical and surge flow hemostatics.
- Vascular injury:
Less than 1% of incidents have been reported.
The iliac arteries are at risk at L4-L5 and L5-S1, as well as the aorta and inferior vena cava in the region of L1-L4.
Large vascular injury: may need laparotomy or embolization.
- Disc not identified:
Verify the imaging dates, which should be no older than two months.
Verify the appropriate surgical level.
enlarge the operating room corridor.
Failed-back surgery syndrome: During ten years of follow-up, a recurrence rate of 3-15% and an instability rate of 20% were noted.
- Recurrence:
The 3% to 15% reported occurrence.
Most of the cases of recurrences were found at the same level and on the same side.
The recurrence rate at 5-year follow-up was 6.27% in one research.63% of them happened within a year.
An important correlation was found between moduli changes, disc height index (DHI), and facet orientation (FO).
Higher chances of recurrence were associated with modic type-II and included discs.
Diabetes, disc protrusion, and smoking are all important recurrence predictors.
Obesity increases the risk of LDH development and recurrence.
- Reoperation:
In research of 1850 patients, 130 individuals received reoperations, and 62% of them were successful. In 98%, 54%, and 38% of patients, respectively, herniation at different levels, recurrences at the same level, and scar formation had favorable outcomes.
- Postoperative discal pseudo-cyst :
- Iliac arteriovenous fistula:
- Epidural hematoma:
- Retained Non-absorbable Haemostatic Material (RNHM) such as gossypibomas & melanomas:
What is the result of the Discectomy procedure?
Most people with herniated disc symptoms who can clearly identify a compressed nerve, such as pain that radiates down the legs, benefit from diskectomy. The relief that a diskectomy offers might not be long-lasting since it does not address the underlying issue that led to the disc to become injured or herniated in the first place.
To help avert re-injury of the spine, it might assist to attain and keep a healthy weight, eat a healthy diet, do low-impact exercises, and limiting activities that involve repeated bending, twisting, or lifting.
What is the Physiotherapy Treatment of Discectomy procedure?
Physiotherapy before a lumbar discectomy:
Before your surgery, you will have physiotherapy treatment that will teach you how to stretch and strengthen the muscles that support your back in order to get ready for the procedure and speed up your recovery. Before your surgery, a physiotherapist might also see you go over what to expect after your procedure.
To try to avoid the necessity for surgery, physiotherapy offers lumbar disc prolapse physiotherapy.
Symptoms following a lumbar discectomy:
Following your operation, you can feel some pain and stiffness in your lower back. However, a few hours following surgery, you should be able to get out of bed. You will be taught how to move and transfer safely and comfortably by a physiotherapist. You will be released after your condition is stable and your physiotherapist is certain that it will be safe for you to mobilize at home.
Bending and lifting should be avoided during the first several weeks, according to your physiotherapist’s advice. Your physiotherapist will also give you some easy exercises, which you should do regularly at home to speed up your recuperation. the physiotherapist’s passive stretching of the lower back muscles.
Physiotherapy following a lumbar discectomy
Following lumbar discectomy, we offer individuals specialized and personalized care. For the best possible recovery, physiotherapy treatment should continue following your procedure. In order to speed up your recovery and get you back to where you were before, your physiotherapist will lead you through an organized rehabilitation program catered to your needs, allowing you to resume enjoying the activities you value the most.
1-2 weeks
The primary goals of physiotherapy during the first few weeks following surgery are to reduce pain and inflammation while promoting soft tissue repair. At this time, physiotherapy treatments could include:
- Ice
- Ultrasound
- Massage
- Stretching and gentle active range of motion exercises.
Your physical therapist will also demonstrate safe housekeeping techniques for activities like entering and exiting the bath, climbing stairs, and getting in and out of bed.
2-6 weeks
You will start a planned workout program with your physiotherapist at this point in your recuperation. To enhance energy levels and increase physical fitness, it will be advised to engage in stationary cycling, swimming, and walking.
Exercises to assist strengthen and control the muscles that stabilize the lower back may potentially be a part of your treatment plan. As you perform the exercises to increase confidence and independence with functional activities, your physiotherapist will assist you and provide guidance. As you start to engage in more demanding activities and lift and carry heavier objects, it is crucial to learn how to protect your back. At this point, your physiotherapist will also demonstrate how to get in and out of a car because you might be able to drive short distances safely. Depending on their line of employment, people can return to light duty in 2-4 weeks. At this point, your rehabilitation regimen can include:
- Walking
- Swimming
- Stationary bicycle
- Stretching exercises to increase flexibility
- Exercises to encourage muscle control
- Correcting & varying posture during activities of daily living such as lifting, reaching, and bending
6-12 weeks
Your treatment plan will focus on advancing your prior workouts to strengthen the muscles in and around your lower back and improve your range of motion throughout this period. Your physiotherapist will also consider strategies to make you more comfortable at work, such as posture and positioning. At this time, physiotherapy treatments could include:
- Abdominal strengthening exercises
- Progressing walking distance
- Exercises based on your work or sporting life
To maintain your fitness and achieve your ideal weight, you should keep up with swimming, walking, and stationary cycling. People whose professions require demanding manual labor should be recommended to look into alternative careers.
12+ weeks
With the assistance of your physiotherapist, you will continue to advance at this point in your recovery. The main goal of your rehabilitation will be to increase your confidence in handling routine chores at work or home and ensure that they are completed safely and effectively. You must follow the suggested program exactly if you want to maximize your potential and get back to work.
Every patient experiences a varying period of recovery time before they may resume their regular activities. Pain relief through physical therapy will increase your functional abilities and independence with activities that are essential to you.
FAQ (frequently asked questions)
How Successful Is a Microdiscectomy Procedure? Even though it’s challenging to measure surgical recovery success (because to varying patient lifestyles and activity levels), a constant 80–90% microdiscectomy success rate has been observed in various studies.
Up to 8 weeks may pass before you can resume your regular activities. Your doctor might suggest that you train with a physiotherapist to develop a stronger core and back muscles. To avoid overtaxing your back, you’ll need to learn how to lift, twist, and bend.
An incision needs seven to fourteen days to fully heal. Till you are certain that your stitches won’t be compromised, hold off on hard pounding. If you’ve undergone any form of lumbar spinal fusion surgery, you’ll probably need to wait about six months before you can resume running.
Microdiscectomy, percutaneous discectomy, and lumbar discectomy
There is a little possibility that the surgery won’t lessen the discomfort, or that there will be some short alleviation before the discomfort returns. The disc will herniate again in 5% of instances. Because a discectomy doesn’t stop or undo the cause of the herniated disc, it is not a permanent treatment.
There is a chance of paralysis following discectomy surgery. Like with most spine operations, there is a chance that the spinal cord will be injured, which could cause weakness or paralysis in the torso or limbs. Although extremely unlikely, paralysis can occur, particularly during a microdiscectomy procedure.



One Comment