Delayed Illiacus Compartment Syndrome
Table of Contents
What is a Delayed Illiacus Compartment Syndrome?
Compartment syndrome is a medical condition characterized by increased pressure within a confined space in the body, leading to reduced blood flow and potential tissue damage. One specific manifestation of this syndrome is Delayed Iliacus Compartment Syndrome, which involves elevated pressure within the iliacus muscle compartment of the pelvis. This condition is relatively rare but can have serious consequences if not promptly diagnosed and managed.
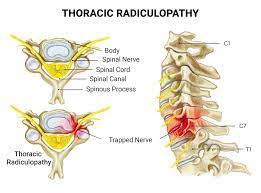
Iliacus compartment syndrome, a very uncommon kind of retroperitoneal compartment neuropathy, occurs on by bleeding inside the iliacus muscle, which compresses the femoral nerve and causes hematoma development, impairing sensory and motor function.
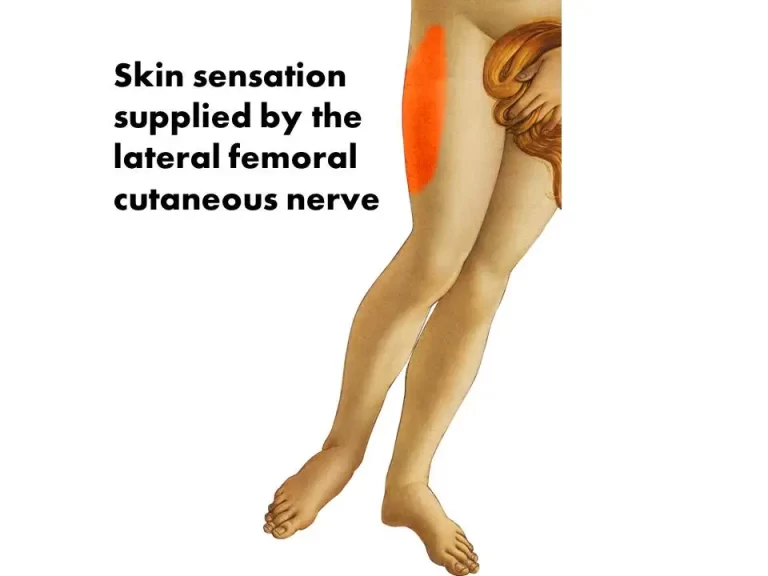
It then manifests symptoms such as iliopsoas muscle weakness, numbness, loss of knee-jerk, and sensory loss of the anteromedial thigh.
Anatomy
The largest pelvic bone, the iliac fossa, has a curved surface and a triangular-shaped, flat muscle called the iliacus that fits into it precisely.
It is also known as the iliopsoas muscle, as well as the psoas major muscle. A part of the illiacus muscle is attached to the iliac fossa, two-thirds from its top. Another part is connected to the inside portion of the iliac crest, the top, outer portion of the pelvic bone.
Other muscle fibers are connected to the anterior sacroiliac and iliolumbar ligaments which run from the base of the sacrum up to the anterior iliac spines (bony projections that are located toward the edges of the iliac). The psoas major muscle, which extends from the lumbar spine in the lower back to the lower pelvis, is where these muscle fibers converge and insert into the tendon. A few of these fibers go as far as the femur, or thighbone.
Origin:
The internal lip of the iliac crest, the lateral side of the sacrum, the ventral sacroiliac section of the iliolumbar ligament, and the upper two-thirds of the iliac fossa.
Insertion:
Lesser trochanter of femur. The fibres of this muscle typically enter in front of the psoas major muscle’s and extend distally across the lesser trochanter of the femur.
Action:
The femur is externally rotated and flexed by the iliacus muscle.
It is also one of the essential muscles for maintaining good posture.
Together with the psoas muscle, these two muscles are regarded as the body’s strongest hip flexors. An anterior tilt of the pelvis (down and forward) can also be enhanced by the iliacus muscle. Hip flexion is controlled by both the iliacus and the iliopsoas. Additionally, whether you complete a sit-up or bend over to tie your shoes, this muscle bends the trunk forward.
The psoas major muscle only becomes active (during gait) just before and during the early swing phase of gait as opposed to the iliacus muscle, which is constantly active during walking. The lateral bending of the trunk is eccentrically controlled by the iliacus muscle.
Causes:
Delayed illiacus compartment syndrome typically occurs as a consequence of trauma or injury to the hip region. It is often associated with blunt trauma, fractures, or muscular strains affecting the illiacus muscle, which is located deep within the pelvis. The injury may cause swelling, hematoma formation, or bleeding within the muscle compartment, which could end in elevated pressure.
Symptoms:
- Severe pain in the hip or groin region, which may worsen with movement.
- Swelling and tightness in the affected area.
- Restricted range of motion, especially with hip flexion.
- Numbness or tingling sensations in the leg or thigh.
- Weakness or difficulty in walking.
Diagnosis:
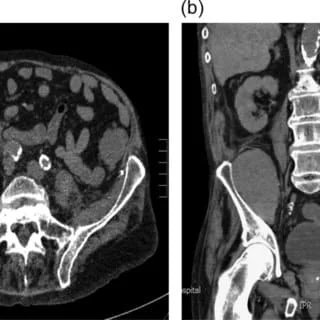
Delayed illiacus compartment syndrome can be challenging to diagnose since its symptoms often overlap with other hip-related conditions. However, a thorough physical examination, medical history review, and imaging tests such as X-rays, CT scans, or MRI scans can help in ruling out other potential causes and identifying the increased pressure within the illiacus muscle compartment.
Treatment:
Treatment options can range from conservative approaches like rest, pain management, and physical therapy to more invasive interventions such as surgical decompression to relieve pressure. The choice of treatment depends on the severity of the condition and the individual patient’s circumstances.
- Immediate medical attention: If DICs is suspected, it is crucial to seek immediate medical attention to prevent further complications. Delayed treatment may lead to muscle necrosis, nerve damage, or even the need for surgical intervention.
- Conservative management: Initial treatment involves reducing the pressure within the iliacus muscle compartment. This is achieved through measures such as rest, immobilization of the affected hip, ice application, and elevation of the leg to minimize swelling. Non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed to manage inflammation and pain.
- Fasciotomy: In severe cases where conservative management fails, surgical intervention in the form of fasciotomy may be necessary. This procedure involves making incisions in the fascia surrounding the iliacus muscle to relieve the pressure. Fasciotomy allows decompression of the muscle compartment, restoring blood flow and preventing further damage.
- Rehabilitation: After the acute phase, a comprehensive rehabilitation program is essential to restore strength, flexibility, and functional mobility. Physical therapy may include exercises to improve hip range of motion, muscle strength, and coordination. It is essential to follow the guidance of healthcare professionals during the rehabilitation process to achieve the best possible outcome.
Exercises:
1. Hip Flexor Stretch:

A conventional hip flexor stretch can be a helpful addition to any hip mobility strategy. Both joint flexibility and muscular strength can be improved by this stretch. Therefore, it could be far more advantageous than a simple flexibility stretch alone.
Do the following to stretch your hip flexors:
- To begin, kneel on one leg with your other leg extended and bent at a 90-degree angle.
- Maintain hip and shoulder alignment with the kneeling leg. The heel and ankle of the front foot should be parallel to the other knee at all times.
- Your hands should be on your front knee, gently pressing down. As a consequence, your core muscles will be worked.
- You should tuck your hips and tailbone beneath your body.
- To stabilize your spine during the workout, tighten your glutes and abs.
- When you start to feel it in your hips, lean slightly forward. Hold this position for few minutes.
- Then, as your knee tries to advance, press your rear foot firmly into the ground. Hold for approximately 30 seconds.
- Remain in the beginning position for 30 more seconds while relaxing.
- After moving your legs, repeat the complete movement on the other leg.
2. Clamshells:
With this workout, you may strengthen your thighs, hips, and glutes. Your pelvic muscles are supported. It can also relieve lower back stress, reducing the possibility of overuse problems. Once you have learned the basic exercise, do some variations.
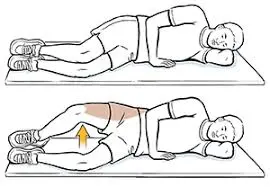
Instructions:
- With your knees bent, lie on the side.
- Rotate your upper leg as far as it will go and hold for a brief moment.
- Lower to the beginning position.
- Perform 1-3 sets of 10–15 repetitions.
3. Bridges:

- Lay down on your back on the ground to begin.
- As you press your core into the floor and feel your hips align with your spine (without arching), check to make sure there is no space between your back and the ground.
- Start drawing the feet towards the glutes from here until you achieve a 90-degree angle.
- Pressing your feet firmly on the ground, keeping your arms at your sides, and tucking your chin to keep your spine straight, Exhale, then raise your bottom back up off the ground.
- Hold this high position for 10-15 seconds.
- Now lower your back to the floor and repeat this 5-10 times in one session.
- You will also do this exercise three to four times a day.
- You can make it more difficult by adding weight, strap, or other equipment.
4. Leg Raises:
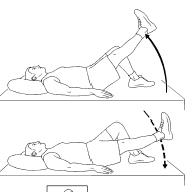
To start the straight leg raise:
- Lie on your straight back with your hips straight and your feet should be comfortably flat on the ground.
- Bend the knee of the uninjured leg to a 90-degree angle and put one foot on the ground.
- Stabilize the rectus leg muscles by contracting the quads.
- Lift your straight leg six inches off the ground while taking a slow, deep breath.
- Hold for three seconds.
- Exhale slowly, and lower your leg under control to the ground.
- Repeat on the other side.
- Relax and repeat this 10 more times.
5. Standing Hip Abduction:

- To provide stability, place a table or chair next to you as you stand with your legs shoulder-width apart.
- Protect your back from harm by drawing in your abdominals. Pulling your umbilicus (belly button) towards your back will do this.
- Kick your leg smoothly out to the side of your body while keeping your knee straight and toes pointing.
- Throughout the workout, be sure to maintain a straight upper body and back.
- Go back to your starting point.
- 3 consecutive times, repeat 15 to 20 times.
- Continue with the other leg.
6. Standing Hip Extension:
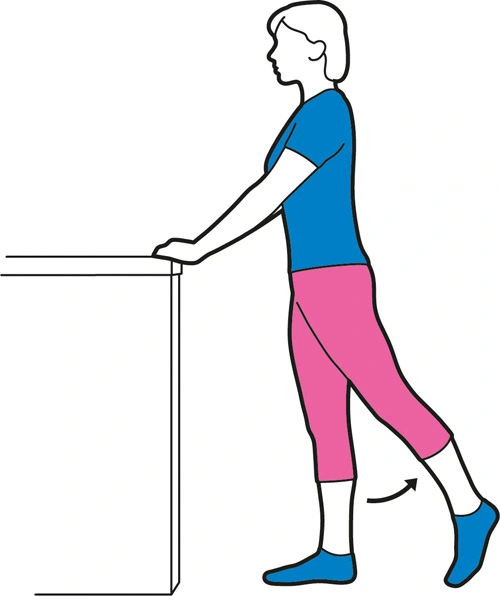
- For balance, stand with your hands on a solid surface like a table or countertop.
- Keep one knee mostly straight and extend the other leg backward and upward.
- Hold this posture while concentrating on tightening your butt muscles.
- Return to your starting posture by relaxing your leg.
- Since everyone is unique, you might need to adapt the standing hip extension to suit your requirements.
7. Static Lunges:
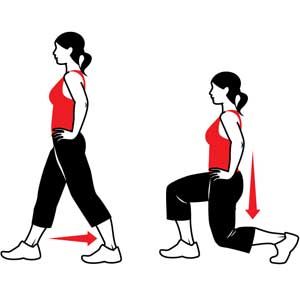
- Stack your shoulders over your hips, tense your abs, and keep your head up.
- Directly advance with your right foot. Step back and lengthen your stance while bending both of your knees 90 degrees.
- For joint protection, cross your front knee over your ankle. According to Levy, injuries to the knees, ankles, and other parts of the body can develop over time if tension is wrongly applied to sections of the body that are not supposed to be under strain.
- Consequently, maintain the proper posture by keeping your knees higher than your toes.
- Your back heel will lift as you bring your back knee towards the floor. Place your heel over your foot’s ball mount.
- Put on your best form and squat as low as you can. Push off your foot with your left leg to stand up straight again while keeping your feet in a split stance. A rep is one.
- Steps should be repeated when switching sides.
8. Prone Hip Extension:
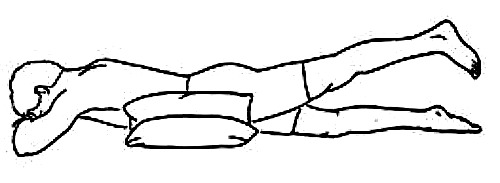
- Your legs should be straight when you lay on the ground on your stomach. On a mat or towel, you can lie down. Put your arms over your head.
- Lift your right leg about one inch above the ground. the right knee must remain straight. Take a 5-second hold.
- Return your leg to the ground slowly.
- Five times, or as directed, repeat.
- If directed, switch legs and repeat.
9. Seated Leg Lifts:

- Your legs should be spread out in front of you while you sit on your butt.
- Straighten your back, keep your body upright, and spread your arms out to either side. Squeeze your biceps and core to fully contract your upper body.
- As high as you can without endangering your posture in the upper body, lift one leg.
- Make careful to maintain tension in your upper body while you hold for two counts.
- After lowering the leg, repeat on the other side.
- 2 to 3 sets of 10 repetitions on each side should be repeated.
Conclusion:
Delayed Iliacus Compartment Syndrome is a rare but potentially serious condition that can occur following trauma or injury to the hip region. Timely diagnosis and appropriate treatment are important to prevent long-term complications. If you experience persistent hip or groin pain, swelling, or restricted mobility after an injury, consult a healthcare professional for an accurate diagnosis and proper management. Remember, early intervention greatly improves the chances of a successful recovery.
FAQs
The condition is often caused by excessive exercise, trauma, or overuse of the iliacus muscle. Swelling within the muscle compartment can result in increased pressure, leading to compression of nearby structures.
Symptoms can include severe pain or discomfort in the groin or hip area, numbness or tingling in the thigh, weakness in the leg, and difficulty walking.
Diagnosis involves a physical examination, medical history review, and possibly imaging studies such as MRI or ultrasound to assess muscle swelling and pressure within the compartment.
Treatment may include rest, ice, anti-inflammatory medications, and physical therapy to reduce muscle swelling. In some cases, surgical intervention might be necessary to relieve pressure.
Avoiding excessive or repetitive activities that strain the iliacus muscle, proper warm-up and stretching, and gradually Increasing exercise intensity can help reduce the risk of developing this condition.
People who engage in activities that involve repetitive hip flexion or intense physical exertion, such as long-distance running, cycling, or certain sports, may be at a higher risk.
The pain associated with delayed iliacus compartment syndrome is often more intense and localized, and it might not improve with rest. It can also cause numbness, tingling, or weakness in the affected leg.
Yes, the symptoms of this condition can overlap with other hip and groin-related issues such as hernias, muscle strains, and nerve compression. Proper diagnosis is important for proper treatment.