Chondromalacia Patellae: Physical therapy Management
Table of Contents
What is Chondromalacia Patellae?
Chondromalacia patellae, or CMP, is a degenerative condition caused by improper loading of the knee. The symptoms of CMP include pain and inflammation in the patellar area, which often causes difficulty when climbing stairs, squatting, and prolonged sitting.
CMP is a common cause of knee pain, especially in young adults. Physical therapy is a treatment option for CMP, and the goal of therapy is to reduce pain and inflammation and improve mobility.
Chondromalacia patella Defination
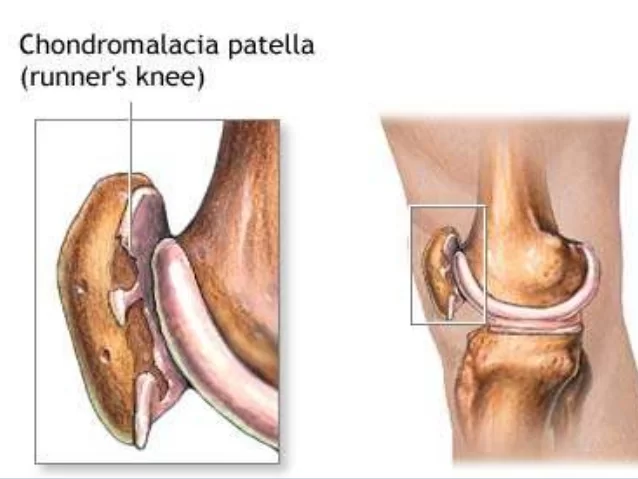
Chondromalacia patellae, also known as “runner’s knee”.
It is a condition where the cartilage on the undersurface of the patella deteriorates and softens.
This condition is common in young, athletic individuals, but may also occur in older adults.
Physical therapy for chondromalacia patellae refers to an exercise and rehabilitation program to help people with this condition. The main goal of physical therapy for chondromalacia patellae is to reduce pain and improve mobility. Physical therapy for chondromalacia patellae is also used to help people with this condition adjust to changes in their activity level, such as when they first return to an exercise program after an injury or illness.
Causes of CMP:
- Poor alignment due to a congenital condition
- An abnormal Q angle is the common cause: The Q angle angle is 14 degrees in men and 17 degrees in women.
- repeated stress to knee joints, such as from running, skiing, or jumping
- a direct blow or trauma to the knee
- Weak hamstrings and quadriceps muscles
- muscle imbalance between the adductors and abductors
- Muscle tightness mainly Rectus femoris, Tensa Fascia late, and Hamstring muscles creates extra pressure on the patellae and knee.
- Patella alta is a condition in which the patella is positioned in an abnormally high position. This may increase the length of the patellar tendon by 20% greater than the height of the patella.
Risk Factor:
- Age: Adolescents and young adults are at high risk
- Previous injury
- gender
- Arthritis
- Obesity
Symptoms:
Pain around the knee.
The pain is usually located at the front of the knee, around or behind the patella.
The pain is typically worse when going up or down stairs.
It may be brought on by sitting for long periods.
crepitus present.
Rarely effusion of the knee joint.
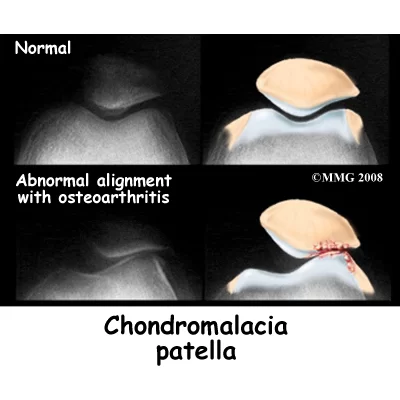
Chondromalacia patella is graded based on the basis of arthroscopic findings, the depth of cartilage thinning, and associated subchondral bone changes.
Moderate to severe stages can be seen on MRI.
- Stage 1: softening and swelling of the articular cartilage due to broken vertical collagenous fibres.
- Stage 2: blister formation in the articular cartilage due to the separation of the superficial from the deep cartilaginous layers.
Cartilaginous fissures affecting less than 1,3 cm2 in area with no extension to the subchondral bone. - Stage 3: fissures ulceration, fragmentation, and fibrillation of cartilage extending to the subchondral bone.
- Stage 4: crater formation and eburnation of the exposed subchondral bone more than 50% of the patellar articular surface exposed, with sclerosis and erosions of the subchondral bone.
Osteophyte formation also occurs at this stage.
Epidemiology
The higher Q angles in women are thought to be the reason why more women than males are impacted. The variance does not seem to have a hormonal explanation. Chondromalacia is more common in active young adults who play running sports or work jobs that put stress on the patellofemoral joint through frequent stair climbing and/or kneeling.
Investigation:
X-ray: an AP view of the patellofemoral joint is needed to detect any radiological change.
In all but the most advanced cases, there is no convincing radiological change.
In the latter stages, patellofemoral joint space narrows, and osteoarthritic changes begin to appear.
Patellar grind test or Clarke’s sign
Extension-resistance test
Physical Therapy treatment:

conservative treatment of chondromalacia patellae is both physical and highly advised.
Short-wave diathermy helps to relieve pain and to increase the blood supply to the area, improving the nutrition supply to the articular cartilage.

Care must be taken when planning an exercise programme.
Isometric quadriceps strengthening and stretching exercises: restoration of good quadriceps strength and function is an important factor in achieving good recovery.
The most effective exercises are isometric and isotonic in the inner range.
stretching of the vastus lateralis and strengthening of the vastus medialis.
Hamstring stretching exercise
Temporary modification of activity
Patellar taping
Foot orthoses
NSAIDS Pain relieving Medicine such as Aceclofenac, and Diclofenac.
Hip strength and coordination training, as well as hip positioning and strength, has a significant influence on anterior knee pain.

Hip abductors strengthening as an increased hip adduction angle is associated with weakened hip abductor
Although stretching can improve flexibility and knee function, it doesn’t necessarily directly improve pain.
Ice medication.
Taping and Braces:
Supporting the patella and knee joint by bracing is a way to reduce pain and symptoms.
but it will also alter patella tracking and reduce the active function of the quadriceps.
Bracing may be used in short-term goal patients for some support and pain relief.
If you want to know more about KT Taping for Chondromalacia patellae pain click here.
Complications
Patients suffering from chondromalacia patella may experience secondary complications due to the usage of NSAIDs (such as gastrointestinal symptoms) or bracing, which can occasionally cause dermatologic responses due to the skin’s reaction to the brace material. It is rare for therapeutic exercises to aggravate symptoms. When an activity is associated with worsening symptoms, the patient, therapist, and clinician should collaborate to adjust the activity (e.g., change the frequency, length, or intensity of the activity or halt the activity temporarily if necessary.)
Prognosis
Reversibility of chondromalacia patellae is possible, as is the possibility that it may develop into patellofemoral osteoarthritis. Patients with chondromalacia patella often heal completely from their knee pain. Recovery times might range from a month to years, depending on the circumstances. Because their bones are still growing, teenagers frequently make a long-term recovery, and their symptoms usually get better as they become older.
Doctors / Consultations
- Orthopedist
- Radiologist
- Rheumatologist
- Physical therapist
FAQs
Treatment options for chondromalacia patellae include medicines, activity modification, soft tissue therapy, physical therapy, and in rare cases, surgery. Exercises for strengthening the hips and knees as well as stretches and massages are possible treatments at Samarpan Physio Clinic.
There is no treatment for true chondromalacia patella, which results in the surface of the cartilage breaking down. However, a weight loss program, avoiding activities that aggravate it, Physical therapy, exercising, and/or injections may enable one to make it go away.
Chondromalacia can arise as a result of post-traumatic injuries, microtrauma wear and tear, and iatrogenic drug injections. Any joint can develop chondromalacia, but the knee and patella are particularly susceptible due to stress and abnormalities in these areas.
Simple conservative techniques are initially used to treat chondromalacia patella. You might be instructed to rest your knee and avoid any motions that put undue strain on the knee joint. To ease pain and reduce swelling, your doctor may recommend physical therapy, painkillers, and anti-inflammatory medications.
Chondromalacia can sometimes improve on its own, but it may not fully heal. It often requires management and treatment to alleviate symptoms and prevent further damage to the cartilage in the affected joint.




3 Comments