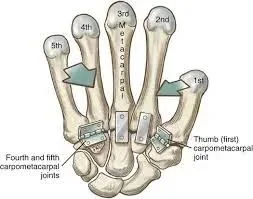
Carpometacarpal joints (CMC joints)
Table of Contents
Introduction
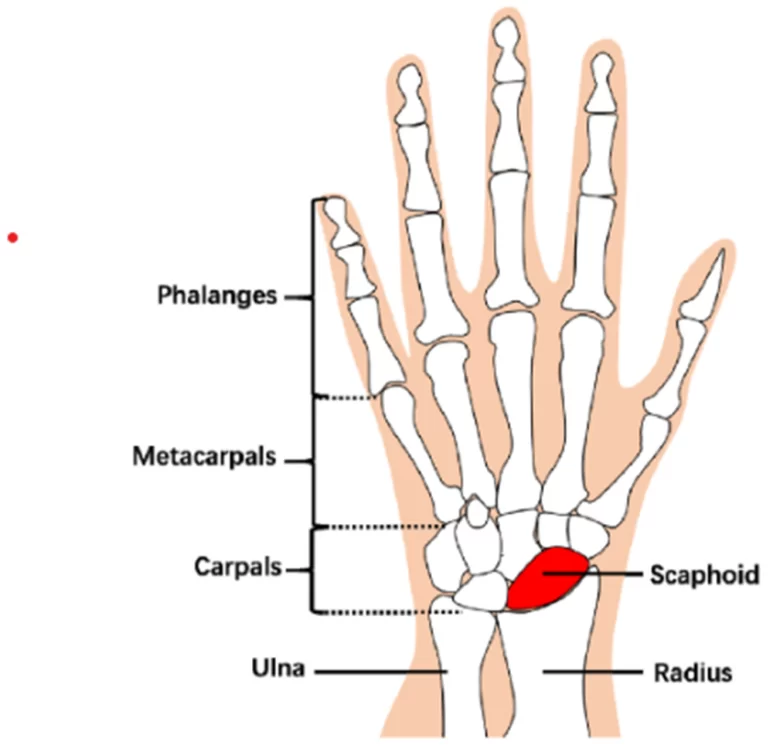
The carpometacarpal (CMC) joints are five wrist joints that connect the distal row of carpal bones to the proximal bases of the five metacarpal bones. The CMC joint of the thumb is also referred to as the trapeziometacarpal (TMC) joint.
The carpometacarpal (CMC) joints connect the carpal (carpo-) and metacarpal (-metacarpal) bones of the hand. The carpometacarpal joint of the thumb (trapeziometacarpal joint) is the most specialized and flexible of the five CMC joints.
The four remaining CMC joints are functional plane synovial joints that connect the medial four metacarpal bones (metacarpals 2, 3, 4, 5) to the distal row of carpal bones (trapezium, trapezoid, capitate, hamate). The common carpometacarpal joint is made up of the three most medial CMC joints.
As one moves medially, the four CMC joints increase their ranges of motion; metacarpals 2 and 3 are almost immobile, metacarpal 4 has a small degree of gliding, and metacarpal 5 can glide to such an extent that it produces flexion and rotation. These characteristics make the medial four CMC joints extremely stable, allowing for a strong connection between the wrist and hand while remaining flexible enough to allow for palm cupping or Object grasping with the thumb during opposition movements.
As the articular surfaces of the CMC joints become more curved, their mobility increases from the radial to the ulnar sides of the hand. There are five CMC joints in total. The first CMC joint is between the trapezium and the first metacarpal base. The second CMC joint is between the trapezoid and the second metacarpal base.
The third CMC joint is situated between the capitate and the third metacarpal base. The fourth CMC joint is between the hamate and the base of the fourth metacarpal. Between the hamate and the base of the fifth metacarpal is the fifth CMC joint.
First Carpometacarpal Joint
The first carpometacarpal joint is also known as the trapeziometacarpal joint (TMC) or The carpometacarpal joint of the thumb (pollex). because it connects the trapezium to the first metacarpal bone and is essential to the thumb’s normal function. Osteoarthritis of the TMC, the most important joint connecting the wrist to the metacarpus, is a severely disabling condition that is up to twenty times more common in elderly women than in the general population.
The first metacarpal’s pronation-supination is especially important for opposition action. The first CMC’s movements are constrained by the shape of the joint, the capsulo-ligamentous complex surrounding the joint, and the balance of involved muscles. If the first metacarpal fails to sit well ‘on the saddle,’ such as due to hypoplasia, the first CMC joint tends to be subluxated (slightly displaced) towards the radius.
The capsule is sufficiently slack to allow for a wide range of motion and a 3 mm distraction while reinforcing ligaments and tendons to provide joint stability. It is slightly thicker on the dorsal side than on the ventral side.
Osteoarthritis of the first carpometacarpal joint is common in postmenopausal women.
Type
Saddle variety of synovial joints (because the articular surfaces are concavoconvex).
Articular Surfaces
- The distal surfaces of the trapezium
- Proximal part of the first metacarpal bone.
Trapeziums’ articulating surfaces are concave in the sagittal plane and convex in the frontal plane.
The concavoconvex nature of the articular surfaces allows for a wide range of movements.
Ligaments
The number and names of the ligaments of the first CMC vary considerably in the anatomical literature. three intracapsular and two extracapsular ligaments as the most important in thumb stabilization.
Anterior oblique ligament (AOL)
A strong, thick, intracapsular ligament that originates on the trapezium’s palmar tubercle and ends on the first metacarpal’s palmar tubercle. It is taut in abduction, extension, and pronation, and it has been reported that it has an important retaining function and that it is elongated or absent in CMC joint arthritis.
Ulnar collateral ligament (UCL)
The UCL is an extracapsular ligament that runs ulnarly to the AOL. It originates on the flexor retinaculum and is inserted on the first metacarpal’s ulnopalmar tubercle. It is taut in abduction, extension, and pronation and is frequently elongated in the presence of CMC joint arthritis. The importance of the UCL varies greatly among researchers.
First intermetacarpal ligament(IML)
This ligament connects the bases of the second and first metacarpals and inserts onto the first metacarpal’s ulnopalmar tubercle, where its fibres intertwine with those of the UCL. In abduction, opposition, and supination, it is taut. Several researchers have reported that it was the most important restraining structure of the first CMC joint. Some believe it is too weak to stabilize the joint on its own, but it does represent an important restraining structure when combined with the UCL.
Posterior oblique ligament (POL)
The posterior oblique ligament (POL) is an intracapsular ligament that runs from the trapezium’s dorsal side to the first metacarpal’s ulno-palmar tubercle. It is not a vital ligament to the first CMC joint, but it does tighten during forced adduction and radial abduction.
Dorsoradial ligament (DRL)
The DRL, like the previous ligament, is unimportant to the first CMC. It connects the trapezium’s dorsal and first metacarpal sides.
Relations
- Anteriorly: The thenar eminence muscles cover the joint.
- Posteriorly: The thumb’s long and short extensors are located
- Medially: First dorsal interosseous muscles and the redial artery
- Laterally: Tendon of the abductor pollicis longus
Movements
Flexion
opponens pollicis
flexor pollicis brevis
flexor pollicis longus
Extension
abductor pollicis longus
extensor pollicis longus
extensor pollicis brevis
Abduction
abductor pollicis longus
abductor pollicis brevis
Adduction
adductor pollicis
extensor pollicis longus
Opposition
Movement of the thumb pulp across the palm to approach the pulps of the digits.
simultaneous abduction, flexion, and pronation of the thumb generate opposition
Retroposition
The thumb pulp is elevated into extension and ulnar adduction.
extensor pollicis longus
Circumduction
The sequential occurrence of extension, abduction, flexion, and abduction (or the reverse) results in circumduction.
Flexion and extension in the plane of the palm are permitted, as are abduction and adduction in a plane at right angles to the palm, circumduction, and opposition. The tip of the thumb comes into contact with the volar surfaces of the slightly flexed fingers due to the movement of opposition. This movement is made possible by a small sloping facet on the anterior lip of the saddle-shaped articular surface of the greater multangular. The Flexor muscles pull the corresponding part of the articular surface of the metacarpal bone onto this facet, and the Adductors perform the opposing movement.
Flexion of this joint is initiated by the Flexores pollicis longus and brevis, with assistance from the Opponens pollicis and Adductor pollicis. The abductor pollicis longus is primarily responsible for extension, with assistance from the Extensores pollicis longus and brevis. The Adductor performs adduction; abduction is performed primarily by the Abductores pollicis longus and brevis, with assistance from the Extensors.
Joint Capsule
The fibrous joint capsule is lined with a separate synovial membrane.
Arterial supply
The carpal joints are supplied by the radial and ulnar arteries’ posterior carpal branches, as well as the anterior interosseous artery.
Dorsal metacarpal branch of the radial artery.
Innervation
Lateral antebrachial cutaneous nerve
Palmar cutaneous branch of the median nerve.
Superficial radial nerve
Second to fifth carpometacarpal joints
Articular surfaces
The CMC joints connect the distal surfaces of the four distal carpal bones to the metacarpal bases of the four medial metacarpal bones.
The trapezium, trapezoid, capitate, and second metacarpal bones combine to form the second CMC joint. The trapezium’s distal portion medially directs a quadrilateral and flat bony protrusion (facet) connecting with a quadrilateral facet on the second metacarpal base. The trapezoid’s triangular distal surface is concave coronally and convex in the transverse plane, ‘cupping’ a concave groove on the second metacarpal base.
A deep ridge medial to this groove articulates with the capitate bone’s concave, anterolateral corner. These characteristics identify the second CMC joint because it is the only one with three carpal bones involved in the articulation.
The third CMC joint connects the capitate to the third metacarpal bone. Through its triangular and primarily concave distal surface, the capitate articulates with a convex facet on the metacarpal base.
The capitate bone, along with the hamate and fourth metacarpal bones, helps to form the fourth CMC joint. In this case, the anteromedial corner of the capitate projects an articulating facet towards the fourth metacarpal base’s large, oval dorsal facet. A small, anterolateral facet on the distal surface of the hamate bone meets the partially convex and concave quadrangular proximal surface of the metacarpal base.
The neighbouring larger, anteromedial facet on the same distal surface of the hamate, along with the fifth metacarpal bone, contributes to the formation of the fifth CMC joint. A transversely concave and coronally convex laterobasal surface connects this metacarpal base to the hamate. This transition from concave to convex is not abrupt but rather slopes downwards, almost flatly. This rounded edge on the articular surface of the hamate bone allows the fifth CMC joint to move more freely than the other CMC joints.
Ligaments
Three types of ligaments stabilize the CMC joints: dorsal carpometacarpal ligaments, palmar carpometacarpal ligaments, and interosseous ligaments. These soft tissue structures are thickenings of the fibrous joint capsule that surrounds the CMC joints.
Dorsal carpometacarpal ligaments
The dorsal carpometacarpal ligaments, which are located on the dorsal side of the hand, are the strongest and provide the most support to the CMC joints. They are made up of seven ligamentous bands that run obliquely between the dorsal surfaces of the carpal bones in the distal row and the four medial metacarpal bases.
Metacarpals 2, 3, and 4 each receive two bands: the trapezium and trapezoid for metacarpal 2, the trapezoid and capitate for metacarpal 3, and the capitate and hamate for metacarpal 4. The fifth metacarpal is an exception in that it only receives one ligamentous band from the hamate bone. To form an incomplete capsule, this band connects to the corresponding palmar carpometacarpal ligament.
Palmar carpometacarpal ligaments
The palmar carpometacarpal ligaments are very similar to their dorsal counterparts and are located on the palmar aspect of the hand. The third metacarpal base is the only exception, as it receives three ligamentous bands: one lateral from the trapezium/trapezoid, one intermediate from the capitate, and one medial from the hamate.
Interosseous ligaments
The interosseous ligaments are the smallest CMC joint stabilizers. They are made up of two thick, fibrous bands that run between the inferior aspect of the capitate and hamate bones’ distal margins and the third and fourth metacarpal bases.
These bands can be completely separated or proximally united. If separated, the lateral band connects the capitate to the third metacarpal base and the medial band to the fourth metacarpal base. Furthermore, by creating a separate synovial cavity between the hamate and the fourth and fifth metacarpal bones, the medial interosseous ligament can sometimes divide the CMC joint space into medial and lateral compartments.
Movements
According to their structural makeup, the four CMC joints are all synovial. However, their articular surfaces, functional classification, degrees of freedom, and ranges of movement (ROM) divide them into two groups. As one travels medially across the four CMC joints, the latter gradually rises.
Moving from the radial to the ulnar side, the range of motion of the second to fifth carpometacarpal joints increases. The long flexor and extensor digitorum muscles contract to produce minor gliding movements at these joints. The fifth carpometacarpal joint is extremely mobile; contraction of the opponens digiti minimi produces flexion and lateral rotation at this joint, allowing for palm ‘cupping’
Muscles acting
The movements of the four medial CMC joints are not dependent on direct muscle action. The flexor digitorum profundus and extensor digitorum muscles, on the other hand, influence joint translational movements. Because these antagonistic muscles act on the phalanges, they indirectly cause the CMC joints to glide and produce flexion and extension in the fourth and fifth CMC joints, respectively.
The direct involvement of the opponens digiti minimi in the rotational movement of the fifth CMC joint is the only exception. When the muscle acts as an agonist, it brings the fifth finger to the palm, externally rotating it and hollowing the palm. The antagonists of opponens digiti minimi: adductor pollicis, opponens pollicis, flexor pollicis brevis, and abductor pollicis brevis oppose and smoothly control these movements. Palmaris brevis, abductor digiti minimi, and flexor digiti minimi work together to stabilize the joint during movement.
Several soft tissue structures are linked to the four medial CMC joints. The tendons of several muscles, including the flexor digitorum superficialis, flexor digitorum profundus, flexor carpi radialis (laterally), and flexor carpi ulnaris (medially), overlaid the CMC joints on the palmar aspect of the hand. The hypothenar muscles also provide superficial covering to the medial CMC joints.
The CMC joints are located on the dorsal aspect of the hand, close to the tendons of the extensor forearm muscles. Extensor carpi radialis longus, extensor carpi radialis brevis, extensor pollicis longus, extensor indicis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris are some examples.
Joint capsule
A common fibrous capsule surrounds and stabilizes the four CMC joints. A synovial membrane lines this fibrous capsule and secretes viscous synovial fluid, which acts as a lubricant. The synovial membrane is usually continuous with the intercarpal joint lining.
The CMC joint cavity extends proximally and distally, communicating with the midcarpal and intermetacarpal joint spaces. Hyaline cartilage lines the articular surfaces of the CMC joints.
Arterial supply
Posterior carpal branch of the radial artery
Posterior carpal branch of the ulnar artery
Anterior interosseous artery
Innervation
Dorsal ulnar nerve
Anterior interosseous nerve
Superficial radial nerve
Synovial membranes of carpometacarpal joints
The synovial membrane is a continuation of the intercarpal joint membrane. A synovial membrane separates the joint between the hamate and the fourth and fifth metacarpal bones on occasion.
The synovial membranes of the wrist and carpus are thus counted as five:
The first runs from the lower end of the ulnar to the radius’s ulnar notch and lines the upper surface of the articular disc.
The second runs from the articular disc and lower end of the radius above to the first row of bones below.
The third, and most extensive, runs between the contiguous margins of the two rows of carpal bones, and occasionally, if one of the interosseous ligaments fails.
Clinical importance of carpometacarpal joints
Carpometacarpal joint osteoarthritis is a type of joint disease caused by the breakdown of joint cartilage and underlying bone. Traeziometacarpal osteoarthritis is the term used when it affects the thumb.
The presence of a small immovable protuberance over the joint is referred to as carpometacarpal bossing.
Summary
The carpometacarpal (CMC) joints are five wrist joints that connect the distal row of carpal bones to the proximal bases of five metacarpal bones. The first CMC joint, also known as the trapeziometacarpal (TMC) joint, is essential for the thumb’s normal function and is more common in elderly women.
The first CMC joint has three intracapsular and two extracapsular ligaments, covering the muscles of the thenar eminence, long and short extensors of the thumb, first dorsal interosseous muscles, and the radial artery. The CMC joints are stabilized by dorsal carpometacarpal ligaments, palmar carpometacarpal ligaments, and interosseous ligaments.
The movements of the CMC joints are synovial, but their articular surfaces, functional classification, degrees of freedom, and ranges of movement divide them into two groups. The four medial CMC joints are indirectly affected by the flexor digitorum profundus and extensor digitorum muscles. The CMC joints are located on the dorsal aspect of the hand, close to the tendons of the extensor forearm muscles.
FAQs
Which carpometacarpal joint is the most mobile?
The first CMC joint (also known as the thumb’s saddle joint) is the most mobile, especially during opposition movement.
What kinds of movements take place at the carpometacarpal joint?
The CMC joint functions as a universal joint, allowing extension, flexion, adduction, and abduction motion. These movements, when combined, allow for complex thumb movements such as opposition, retropulsion, palmar and radial abduction, and adduction.
Where does CMC joint pain occur?
That CMC joint, in particular, wears out as we age, causing pain at the base of the thumb.”
What is the weakness of CMC?
Osteoarthritis of the thumb carpometacarpal (CMC) joint is a common degenerative disease that causes significant morbidity and functional impairment. Patients with early CMC OA typically have hand weakness when pinching, grasping, or twisting objects.
Is the carpometacarpal joint small or medium in size?
Because the carpometacarpal joint is considered a small joint, code 20600, Arthrocentesis, aspiration and/or injection, small joint or bursa (eg, fingers, toes); without ultrasound guidance, is appropriate for this procedure.
References:
- Chaurasia, B. D. (2019, June 30). Bd Chaurasia’s Human Anatomy, Volume 1. CBS Publishers & Distributors Pvt Limited, India.
- Carpometacarpal joint. (2023, January 29). Wikipedia. https://en.wikipedia.org/wiki/Carpometacarpal_joint#:~:text=The%20carpometacarpal%20(CMC)%20joints%20are,of%20the%20five%20metacarpal%20bones.&text=Ligaments%20of%20wrist.
- BSc, A. R. (2023, July 5). Carpometacarpal (CMC) joints. Kenhub. https://www.kenhub.com/en/library/anatomy/carpometacarpal-cmc-joints
- Micheau, A., & Hoa, D. (2023, September 5). Carpometacarpal joints. e-Anatomy – IMAIOS. https://www.imaios.com/en/e-anatomy/anatomical-structure/carpometacarpal-joints-1537028652
- Weerakkody, Y., & O’Shea, P. (2020, October 28). Carpometacarpal joint. Radiopaedia.org. https://doi.org/10.53347/rid-83565