Amputation
Table of Contents
What is Amputation
Amputation is the surgical removal of all or part of a limb or extremity such as an arm, leg, foot, hand, toe, or finger. It is done by trauma, prolonged constriction, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventative surgery for such problems.
A special case is that of congenital amputation, a congenital disorder, where fetal limbs have been cut off by constrictive bands. In some countries, amputation of the hands, feet, or other body parts is or was used as a form of punishment for people who committed crimes. Amputation of the leg — either above or below the knee — is the most common amputation surgery.

Causes of Amputation
There are many reasons an amputation may be necessary. The most common is poor circulation because of damage or narrowing of the arteries, called peripheral arterial disease. Without adequate blood flow, the body’s cells cannot get oxygen and nutrients they need from the bloodstream. As a result, the affected tissue begins to die and infection may set in.
Circulatory disorders
Diabetic foot infection or gangrene (the most frequent reason for infection-related amputations)
Sepsis with peripheral necrosis
Neoplasm
Transfemoral amputation due to liposarcoma
Cancerous bone or soft tissue tumors (e.g. osteosarcoma, chondrosarcoma, fibrosarcoma, epithelioid sarcoma, Ewing’s sarcoma, synovial sarcoma)
Melanoma
Trauma
Three fingers from a soldier’s right hand were traumatically amputated during World War I.
Severe limb injuries in which the limb cannot be saved or efforts to save the limb fail.
Traumatic amputation (an unexpected amputation that occurs at the scene of an accident, where the limb is partially or entirely severed as a direct result of the accident, for example, a finger that is severed from the blade of a table saw)
Amputation in utero (Amniotic band)
Deformities
Deformities of digits and/or limbs (e.g., proximal femoral focal deficiency, Fibular hemimelia)
Extra digits and/or limbs (e.g., polydactyly)
Infection
Bone infection (osteomyelitis)
Diabetes
Frostbite
Athletic performance
Sometimes professional athletes may choose to have a non-essential digit amputated to relieve chronic pain and impaired performance. Australian Rules footballer Daniel Chick elected to have his left ring finger amputated as chronic pain and injury were limiting his performance. Rugby union player Jone Tawake also had a finger removed. National Football League safety Ronnie Lott had the tip of his little finger removed after it was damaged in the 1985 NFL season.
Legal punishment
Amputation is used as a legal punishment in a number of countries, among them Saudi Arabia, Yemen, United Arab Emirates, Iran, Sudan, and the Islamic regions of Nigeria.
Congenital amputation: what is it?
This is a word used to describe an incompletely formed or absent hand, foot, arm, or leg that exists from birth rather than a procedure. Congenital amputation children may have artificial limbs or surgery later in life if the kid, parents, and care team think that this will enhance the child’s quality of life and function.
Amputation types
Amputation types are categorized according to the level of Amputation
LEVEL OF AMPUTATION
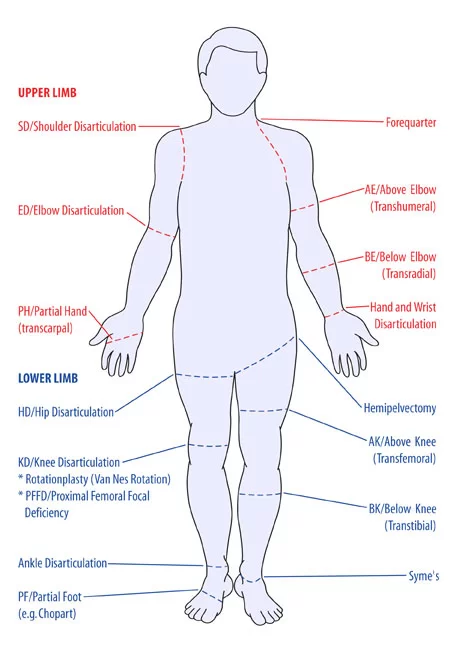
Amputation in the Upper Limb
- Forequarter
- Shoulder Disarticulation SD
- Transhumberal (Above Elbow AE)
- Elbows Disarticulation ED
- Transradial (Below Elbow BE)
- Hand/ Wrist Disarticulation
- Transcarpal (Partial Hand PH)
Amputation Lower Limb
- Hemipelvectomy
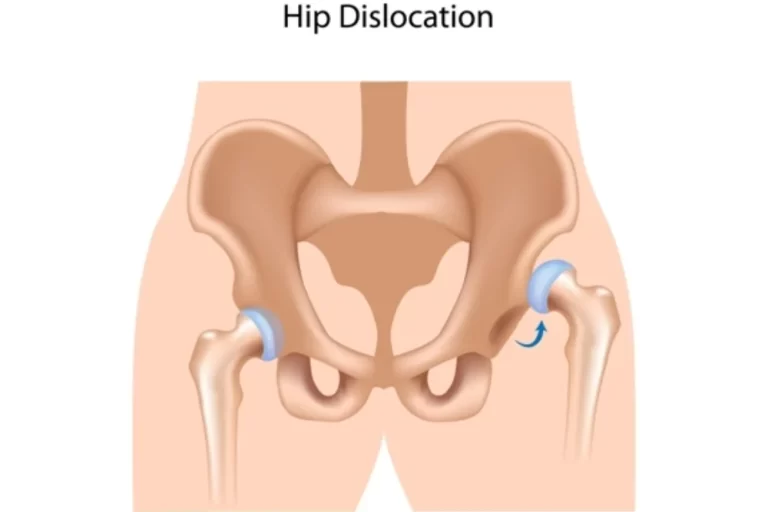
- Hip Disarticulation HP
- Transfemoral TF (Above Knee Amputation – AK)
- Knee Disarticulation KD
- Transtibial TT (Below Knee Amputation – BK)
- Ankle Disarticulation
- Symes
- Partial Foot PF (Chopart)
PROCEDURE
The first step is ligating the supplying artery and vein, to prevent hemorrhage (bleeding). The muscles are transected, and finally, the bone is sawed through with an oscillating saw. Sharp and rough edges of the bone are filed down, skin and muscle flaps are then transposed over the stump, occasionally with the insertion of elements to attach a prosthesis.
Distal stabilization of muscles is recommended. This allows effective muscle contraction which reduces atrophy, allows functional use of the stump, and maintains soft tissue coverage of the remnant bone. The preferred stabilization technique is myodesis where the muscle is attached to the bone or its periostium. In joint disarticulation amputations tenodesis may be used where the muscle tendon is attached to the bone. Muscles should be attached under similar tension to normal physiological conditions.
Ideal stump
skin flaps: skin should be mobile, sensation intact, no scars
muscles are divided 3 to 5 cm distal to the level of bone resection
nerves are gently pulled and cut cleanly so that they retract well proximal to the bone level to reduce the complication of neuroma
Location of pulses
- Femoral Triangle
- Foot pulse (Medial malleolus or dorsum of the foot)
- Popliteal (behind the knee)
- Femoral (within the femoral triangle)
- If a leg has been amputated because of gangrene, the remaining leg is examined for a pulse
The surgeon may choose to close the wound right away by sewing the skin flaps which called as closed amputation. Or the surgeon may leave the site open for several days in case there’s a need to remove additional tissue.
The surgical team then places a sterile dressing on the wound and may place a stocking over the stump to hold drainage tubes or bandages. The doctor may place the limb in traction, in which a device holds it in position, or may use a splint.
SPECIAL INVESTIGATION
- X-rays
- CT scan
- Angiogram (outlines blood vessels)
- Doppler ultrasound (occlusion of vessels)
- Venogram and arteriogram
- Radioactive dye injected into the blood
The Team for Amputation Surgery
Surgical amputation is performed by orthopaedic and orthopaedic oncologic surgeons in collaboration with a plastic and reconstructive surgeon, several nurses, and surgical technicians. They collaborate to remove the ill or injured bodily part, and then they use the soft tissue and leftover bone to form the stump. The surgical team may decide to leave the bone in place for later osseointegration (OI) or shape the soft tissue at the end of the limb to better accommodate a prosthetic.
Treatment:
Pre-Operative Management
If the patient has problems with phantom pain (a sense of pain in the amputated limb) or grief over the lost limb, the doctor will prescribe medication and/or counseling, as necessary.
Physiotherapy, beginning with gentle stretching and Strengthening exercises, often begins soon after surgery. Practice with the artificial limb may begin as soon as 10 to 14 days after surgery.
After Amputation, Healing and Wound Management
The recovery process and a personalized rehabilitation program can provide you the best opportunity to continue your daily activities, regardless of whether you want to use a prosthetic.
The post-amputation stump needs to be kept dry, clean, and bandaged until the sutures can be taken out. Your surgeon and you will examine the surgical site to look for any spots that are healing poorly or are open.
To stop the stump from enlarging as the blood vessels repair, the doctor could prescribe a shrinker sock after the first bandaging is removed. If you intend to use a prosthesis, this procedure helps get the stump ready for one. Usually, you start wearing it for a short while to make sure it doesn’t pinch the skin, and then you work your way up to wearing it for 23 hours a day.
Phantom Limb and Additional Sensory Problems Following Amputation
Amputation patients almost always feel phantom limb sensations and pain. It’s possible that after amputation, the residual nerve connections in the spinal cord and brain “remember” the amputated bodily part, however, the exact explanation is yet unknown.
This leads to severe pain or the feeling that the body part is still present, a condition called “phantom limb syndrome.” The exact causes of this condition is unknown. These signs and symptoms can be rather upsetting.
The nerves that return feelings that affect pain and phantom sensations to the brain can be addressed by the surgeon during the amputation procedure. While these actions might not completely solve the issues, they can lessen both the likelihood and severity of problems occurring. Patients who have already had an amputation but are still in severe pain may also have the nerve treatments done later.
Risk of Falling After Amputation
After amputation of a foot or leg, patients are at high risk of falls during the early stages of their recovery. This is more likely to happen if they attempt to get out of bed in the middle of the night and forget that they have been amputated. These falls have the potential to be quite dangerous, as they may worsen the surgical site and require extra attention or even surgery. A wheelchair or walker next to the bed might serve as a helpful reminder to never try standing and walking by yourself.
The patient can learn to live with the loss of the leg and prevent falls with the assistance of rehabilitation treatment and exercises done in front of a mirror.
Pain Management Following Amputation
Any procedure has the potential to cause uncontrollable pain, thus the amputation team makes every effort to ensure that pain is tolerable. If at all possible, pain management plans should start before surgery. To manage pain and phantom limb symptoms, a peripheral nerve block may be required.
Physiotherapy Treatment
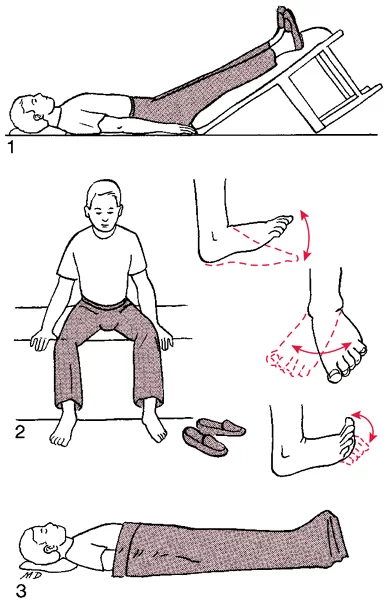
Burger’s Exercise
Stimulates collateral blood flow in the patient’s leg
It is performed for 20 min.
The leg is elevated until the toes go white, then lowered, then level
Repeat 2-3 times to improve collateral circulation
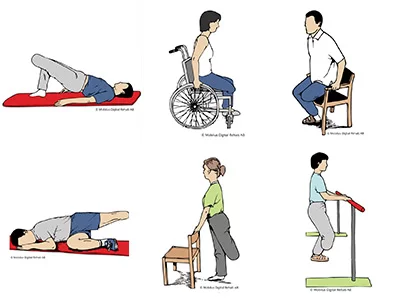
Post-Operative Management
- Connective tissue massage
– Effleurage massage
– Rolling
– It relieves tightness and loosens the muscles - Dynamic stump exercises


- Balance exercise and gait retraining
– Improve static and dynamic balance
– Use Parallel bars, a walking frame then Crutches (in that order)
– Therapist stands on the amp side, using a belt around the patient’s waist to support
– Rest if the patient feels tired - Maintain function in the remaining leg and stump to maintain peripheral circulation
- Maintain respiratory function (important with smokers and those patients under general anaesthesia)
Stump Care
- For hygiene and skin care see the handout on amputations
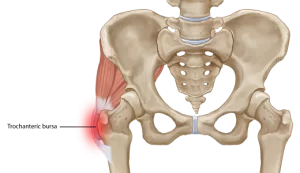
- A hip flexion Contracture may develop because of elevation to reduce swelling
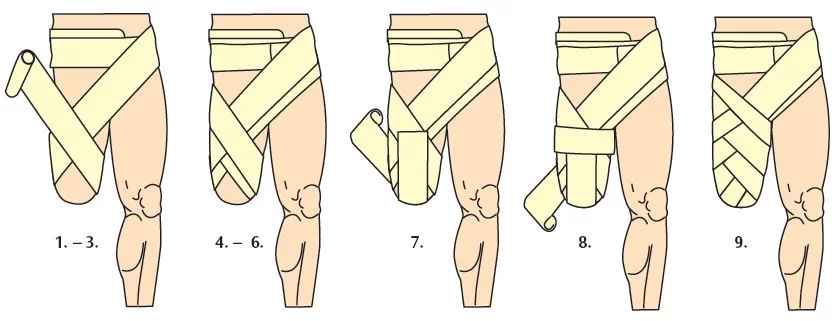
- Stump bandaging is done to ‘cone’ the stump, thereby preventing oedema, which occurs because there is no muscle pump and the stump hangs
- Swelling must be prevented to allow proper attachment of the Prosthesis, and the prevention of Pressure sores
- The stump sock is put on first, then the prosthesis
- The prosthesis must be cleaned and maintained (Children who are still growing, grow out of their prostheses)
Mobility Aids
The choice of mobility aids depends on the level of fitness, strength, balance skills of the individual:
- Walking frame
- Axillary crutches
- Elbow crutches
- Walking stick

- For bilateral lower limb amputees a wheelchair is indicated (high energy expenditure during gait with prostheses)

Complications of Amputation
After Amputation have few complications. There is also a risk of additional problems directly related to the amputated limb.
There are too many factors that have the risk of complications from amputation, such as your age, the type of amputation you’ve had, and your overall fitness /health.
The risk of serious complications is lower in pre-planned operations than in emergency amputations.
Following Complications associated with having an amputation include:
- stump pain (phantom limb” pain)
- slow wound healing
- wound infection
- heart problems such as heart attack
- DVT (deep vein thrombosis)
- pneumonia
In some cases, further surgery may also required to correct symptoms that develop or to help relieve pain. eg. if neuromas (thickened nerve tissue) are thought to be causing radiating pain, the affected cluster of nerves may need to be removed.
FAQs
Following the inspection, the Pathology department is often presented with two options: either the excised body part is used for medical study or it is disposed away as “specific hospital waste”. After that, this garbage is disposed away alongside regular hospital waste.
Losing a limb can have two effects. The pain of an amputation, both physically and mentally, comes first. The persistent pain that follows can be almost as crippling as the initial injury for almost 80% of amputees. Some people report that the discomfort originates from the excised limb.
Amputations can be performed using spinal anaesthesia, which numbs the body from the waist down, or general anaesthesia, which puts the patient to sleep. The surgeon removes all diseased tissue during an amputation while preserving the greatest amount of good tissue.
Traumatic amputations result from accidents or injuries, whereas surgical amputations are caused by a variety of conditions, including blood vessel illness, cancer, infection, excessive tissue damage, malfunction, discomfort, etc. Congenital amputation is the term for missing a part of the body before birth.




2 Comments