What Is Physiotherapy?
Table of Contents
Overview
Physiotherapy (Physical Therapy) is a healthcare profession focused on restoring, maintaining, and maximizing a person’s movement, function, and overall well-being. It addresses physical issues caused by injury, illness, disability, or aging.
Physiotherapy (PT) management frequently involves the use of targeted exercises, manual therapy, manipulation, mechanical devices such as traction, education, and electrophysical modalities such as heat, cold, electricity, sound waves, and radiation. The use of other therapies and assistive technology, such as orthoses and prostheses, is also common. They provide services that assist individuals in gaining, maintaining, and regaining their mobility.
maximum functional ability and range of motion for the length of one’s life. This is the provision of care when aging, diseases, accidents, or environmental conditions compromise a person’s ability to move and perform daily duties.
Good health requires the ability to move freely. Musculoskeletal, orthopedic, cardiology, neurology, endocrinology, sports medicine, geriatrics, pediatrics, women’s health, wound care, and electromyography are just a few of the many specialties that physiotherapy offers.
The field of neurological rehabilitation, in particular, is growing quickly. PTs are employed in a variety of situations, including privately owned physical therapy (PT) establishments.
Outpatient clinics or office centers, sports training facilities, schools, study and instruction facilities, individual houses, funeral homes, long-term care facilities, skilled nursing homes, and health and wellness centers.
Physiotherapists not only treat patients but also work in non-patient care roles like executive, administrative, insurance, and health policy roles in the medical industry.
Physiotherapists offer impartial medical evaluations and peer reviews in the area of medical-legal expertise.
Countries have very different approaches to education. From some countries with very little formal education to others with doctorates, fellowships, and post-doctoral residencies, the range of educational achievement is wide.
Compared to other healthcare occupations, physiotherapy is categorized as an allied health profession. A “memorandum of understanding” has been agreed by World Physiotherapy and the other four members of the World Health Professions Association to “increase their collaboration on protecting and investing in the medical field to deliver secure, successful, and impartial treatment everywhere.”
What is Physiotherapy?
Physical therapy, sometimes known as physiotherapy or PT, is a medical specialty that uses disease prevention, physical intervention, patient education, and health promotion to maintain, improve, or regain health.
These specialists are referred to as physical therapists in the United States, while “physiotherapist” is the word used in many other countries.
Electromyography, neurology, endocrinology, orthopedics, cardiac, musculoskeletal, geriatrics, sports medicine, and women’s health are just a few of the many specializations available in this field.
PTs work in both public and private environments. Physiotherapy contains clinical care, research, teaching, consultancy, and health management.
In some legal systems, such as the UK, physiotherapists can write medication prescriptions.
What is Physiotherapy Video
History
Following the development of orthopedics in the seventeenth century, tools such as the gymnastic were developed to treat gout and other diseases by systematically strengthening the joints, much like later developments in physical therapy.
This term implies “someone who participates in gymnastics with individuals who are ill.”
Women were hired to assist wounded troops in regaining their physical function during World War I, when physiotherapy was institutionalized. Physical therapists were known as “Reconstruction Aides” when they were first hired in 1918.
These new locations included geriatric settings (skilled nursing homes), public schools, health centers at colleges and universities, outpatient orthopedic clinics, and medical facilities.
In 1974, as orthopedics gained popularity as a specialty among physical therapists in the United States, the American Psychological Association established the Orthopedic Section to assist these practitioners.
Since its founding that same year, the International Federation of Orthopedic Manipulative Physical Therapists has made a substantial contribution to the development of manual therapy on a worldwide scale.
Education
Depending on their state, nation, and degree of professional responsibility, physical therapists are required to complete different levels of education. Physiotherapists (PTs) and PTAs are recognized by the physical therapy practice statutes of the majority of US states; some also recognize physical therapy technicians (PT Techs) or assistants.
To start operating as independent practitioners, physical therapists need to be members of the licensing bodies in most countries.
Canada
Fifteen universities in Canada provide physiotherapy programs, most of which are run by their respective medical faculties.
It is not necessary for practicing professionals who currently hold a BScPT certificate to enhance their credentials.
It takes two years on average. Physiotherapy and rehabilitation majors pursue a Bachelor of Science degree after getting accepted. The B.Sc. curriculum normally takes three years to complete. Physiotherapists may choose to specialize in physiology, sports medicine, kinesiology, or rehabilitation sciences.
Technical school graduates can continue their studies at a university after earning their diploma, possibly earning a bachelor’s degree in occupational therapy, kinesiology, exercise science, or physiotherapy.
For its health sciences and rehabilitation programs, several universities in Quebec, including Montréal, Laval, and Sherbrooke, hire physical rehabilitation therapists.
Under these programs, college courses are also accepted for credit. As of right now, no bridge programs are offered to help people transition from the BScPT to the MPT certification.
All universities do, however, grant Doctor of Philosophy (Ph.D.) and Master of Science (MSc.) degrees with a focus on research.
In addition to conducting scholarly research, practitioners can improve their qualifications and skill sets by enrolling in courses and continuing education programs. Ongoing education is necessary for provincial regulatory agencies.
The following physiotherapy regulating organizations are members of CAPR and are accepted in their respective provinces and territories:
- Yukon Government, Consumer Services
- British Columbia College of Physical Therapists
- Alberta College + Association of Physiotherapy
- The Saskatchewan College of Physical Therapy
- Manitoba College of Physiotherapists
- Ontario College of Physiotherapists
- Quebec’s Professional Organization for Physiotherapy
- The College of Physiotherapists in Nova Scotia
- The Physiotherapy College of Prince Edward Island
- Physiotherapists at the Newfoundland and Labrador College
The program consists of seven training phases, each of which includes continuous evaluation and mentoring.
Each of the seven training phases that make up the program includes continuous coaching and assessment. After passing the related tests and completing both of these courses, physiotherapists can apply for a fellowship with the Canadian Academy of Manipulative Physiotherapy (CAMPT).
FCAMPT is a worldwide recognized certification because it has connections with the World Health Organization (WHO), World Physiotherapy (formerly known as the World Confederation of Physical Therapy; WCPT), and the International Federation of Manipulative Physiotherapists (IFOMPT).
Scotland
Students must register with the Health and Care Professions Council, a UK-wide regulating agency, if they intend to operate as “physiotherapists” after graduation.
United States
The primary practitioners of physical therapy are physiotherapists (PTs), who are licensed and qualified to evaluate, diagnose, and treat patients’ or clients’ disabilities, functional limitations, and impairments.
Although some licensed practitioners are also certified with a Master of Physiotherapy or a Bachelor of Science, physical therapy education programs in the United States lead to a Doctor of Physical Therapy (DPT) degree. After earning a bachelor’s degree, students can pursue the entry-level Doctor of Physical Therapy degree, which typically takes three years.
Since the APTA wants all physiotherapists to have a doctorate, PTs who have earned bachelor’s or master’s degrees in the area are encouraged to earn their DPT.
According to the WCPT, four years or more of university-level coursework that has been independently validated and approved should serve as the foundation for entry-level physical therapy education programs.
Cardiovascular, pulmonary, endocrine, metabolic, gastrointestinal, genitourinary, integumentary, musculoskeletal, and neuromuscular systems are examples of clinical sciences material.
The professional curriculum for physiotherapists includes information on the medical and surgical issues that they commonly encounter.
The number of post-doctoral residency and fellowship programs is steadily increasing, with 219 resident and 42 fellowship programs authorized in 2016.
The goal of residency programs is to train physiotherapists in a specialization, whereas fellowships train specialists in a subspecialty (such as division 1 sports, hand therapy, and critical care).
Such as acute care, neurology, geriatrics, wound care, women’s health, sports, cardiovascular and pulmonary, and clinical electrophysiology. Residency programs give them the chance to take the specialized certification exam in their area of specialization.
For example, graduates who complete an orthopedic physical therapy residency are eligible to apply, undergo the clinical, pass the orthopedics specialist exam, and subsequently obtain the OCS designation.
It also symbolizes the trend toward more education to provide patients with the best care possible for their movement disorder.
Physiotherapy assistant-specific associate of applied sciences programs are being taught in the US by CAPTE-accredited standards.
The curriculum for the physical therapy assistant associate’s degree program consists of:
- Physiology and anatomy
- Physiology of exercise
- Human physiology
- Physics,
- Kinesiology,
- Biomechanics,
- Neuroscience
- Pathology in clinical practice
- The behavioral sciences
- Interaction
- Morals
- Investigate
- Additional coursework as specified by each program
Though the qualifications often range from completing a two-year degree program comparable to a high school diploma, physiotherapy technicians and assistants may have different job responsibilities and educational requirements depending on their employer.
64% of PT Aides/Techs have a high school degree or its equivalent, 21% have some college experience but no degree, and 10% have an associate’s degree, according to O-Net.
Some jurisdictions allow physical therapists to employ technicians, assistants, or therapy assistants to do certain, regular tasks related to physical therapy under the strict supervision of a physical therapist.
Depending on the jurisdiction, physical therapy assistants and technicians may need to have specific qualifications.
Employment
Although physical therapy employment in North America has increased rapidly in recent years, employment rates and average salaries may differ significantly across countries, states, provinces, or regions.
According to a Polish study, physiotherapists who are going through professional burnout exhibit symptoms of both increased emotional exhaustion and a decreased sense of personal achievement. Hospital-employed physical therapists who treat adults report significantly higher levels of emotional fatigue.
United States
These workers receive far higher pay—nearly $113,500 a year—for doing temporary assignments that last anywhere from eight to twenty-six weeks.
It can be difficult to evaluate data on PTAs and Techs because the Bureau of Labor Statistics typically provides statistics on both jobs together rather than separately.
Definitions and licensing criteria vary across the United States since each state has established a physical therapy practice act that defines the profession within its boundaries.
The Federation of State Boards of Physical Therapy has, however, also created a model definition to lessen this variance.
United Kingdom
To ensure compliance with ongoing professional development (CPD), all professionals listed on the HCPC registry may undergo audits regularly.
Specialty Areas
Physiotherapists have the option to specialize in a certain therapeutic field due to the abundance of information available regarding physiotherapy.
In addition to the standards established by each specialty board, individuals can currently appear for their specialist examination following 2,000 hours of concentrated practice in their designated specialty population.
The vast majority of physical therapists who work in a specialty will have finished further education, such as a recognized residency program.
Cardiovascular and Pulmonary
Numerous cardiopulmonary disorders can be treated by physiotherapists and respiratory specialists who specialize in cardiovascular and pulmonary rehabilitation. They can also offer preoperative and post-treatment care for patients undergoing heart or lung surgery. One kind of cardiac surgery is coronary bypass surgery.
Manual therapy is used in this field to aid in the release of pulmonary secretions linked to cystic fibrosis.
Geriatric
While geriatric physical therapy treats a variety of conditions that affect people as they age regularly, its primary focus is on older persons.
Numerous conditions, including arthritis, osteoporosis, cancer, Alzheimer’s disease, hip and joint replacement, balance problems, incontinence, and more, can affect people as they age. Experts in addressing these conditions in elderly patients are geriatric physical therapists.
Physical rehabilitation can improve physical health in many ways, including everyday functioning, mood, memory, strength, flexibility, balance, exercise tolerance, and fear of falling, accidents, and mortality, according to the data that is now available.
In addition to lowering handicap and potentially improving mental and physical health, it may be safe, effective, and less likely to have negative side effects.
Physiotherapy may be a helpful intervention with few adverse effects for people in long-term care institutions, according to the research currently available.
However, there is little information to assess if the benefits are cost-effective and durable. Moderate evidence backs up the conclusions.
Wound Management
Among the common conditions treated are burns and wounds. Physiotherapists can use surgical tools, bandages, wound irrigations, and topical drugs to remove contaminated or damaged tissue and promote tissue repair.
Physical therapists in the integumentary specialization carry out duties that are similar to those carried out by doctors or nurses in emergency rooms or triage centers.
Neurology
Neurological illnesses are frequently associated with deficiencies in vision, balance, ambulation, activities of daily living, mobility, muscle strength, and loss of functional independence.
Numerous techniques are used in neurological physical therapy, many of which require specialized expertise.
This is especially important because physical treatment and psychotherapy together can enhance a patient’s neurological condition.
Orthopedics
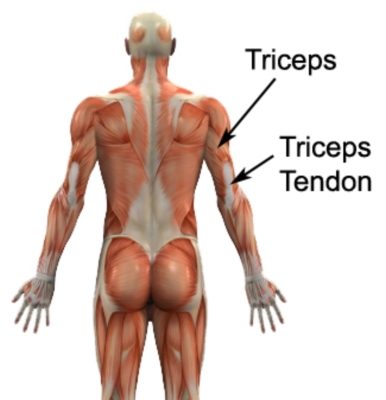
Conditions affecting the musculoskeletal system, including post-orthodontic rehabilitation, acute trauma (sprains, strains), injuries that develop gradually (tendinopathy, bursitis), and deformities (scoliosis), are evaluated, tracked, and treated by orthopedic physical therapists. This specialty of physical therapy is most commonly encountered in the outpatient treatment context.
Another recent development in diagnosis and treatment is the use of sonography to guide therapies such as muscle retraining.
Pediatrics
A variety of techniques are used to provide physical therapy for disorders in the young population, and pediatric physical therapy helps identify health problems early.
These therapists focus on diagnosing, treating, and caring for a variety of congenital, developmental, neuromuscular, skeletal, and acquired disorders and illnesses in children, adolescents, and young adults.
Strength and endurance, balance and coordination, fine and gross motor abilities, and cognitive and sensory integration and processing are the main objectives of treatment.
Sports
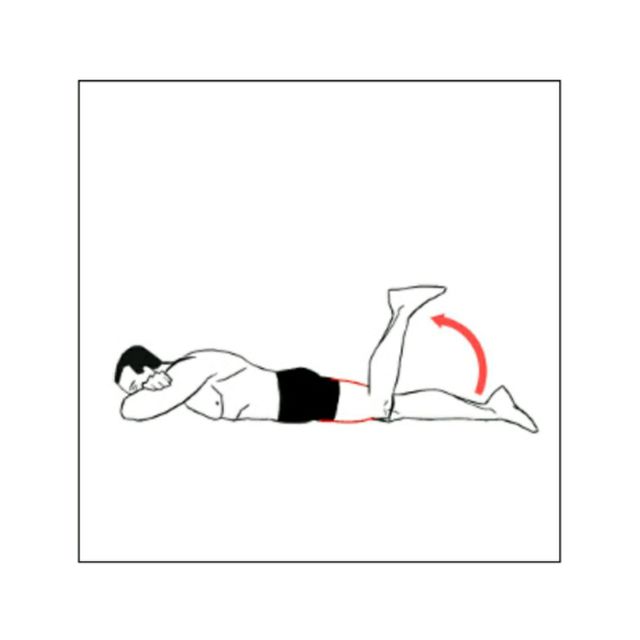
Whether an athlete is semi-professional (paid), professional (full-time), or recreational, physical therapists are essential to their health and well-being. This area of practice covers sports injury care under five main headings:
- The assessment and identification of a fresh injury is known as acute care.
- treatment: the application of specific expertise and techniques to encourage healing;
- Rehabilitation: progressive care that culminates in a complete return to sports.
- Prevention is identifying and fixing defects (such as mobility assessment) that are known to directly cause injuries or act as risk factors for injuries.
- Transferring specialist knowledge to teams, organizations, or individual athletes to aid in injury prevention or treatment is known as education.
Physical therapists are often required by professional sports teams to possess a certain sports accreditation from their national certifying body.
Collaborative sports medicine programs engage most physical therapists who work in athletic contexts.
Women’s Health
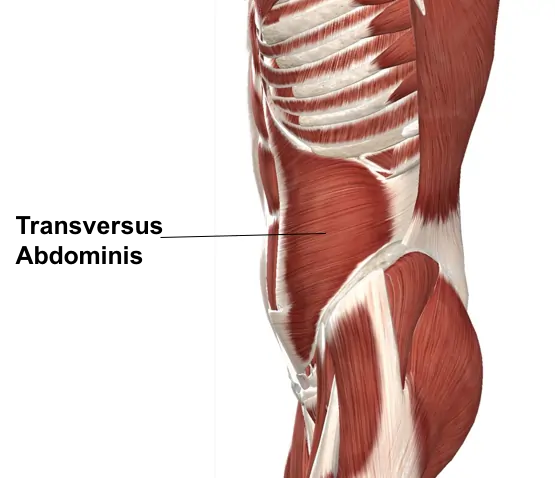
The female reproductive system, childbirth, and the postpartum phase are the main topics of pelvic floor physiotherapy and women’s health.
It treats incontinence, pelvic pain, and pelvic organ prolapse in addition to other disorders associated with pelvic floor dysfunction.
Several studies have demonstrated that manual physical therapy improves infertile women’s chances of becoming pregnant.
Oncology
In the domains of cancer and palliative care, physical therapy is a specialty that is continuously expanding and evolving for both malignant and non-malignant illnesses.
Physical therapy is now recognized as an essential part of the clinical pathway for both patient groups because of advancements in treatment and early diagnosis.
It is generally accepted that patients should have access to an appropriate level of rehabilitation regardless of their expected lifespan to optimize their quality of life and function with the least amount of dependence.
Physiotherapist–Patient Collaborative Relationship
Patients with a variety of illnesses, musculoskeletal diseases, heart conditions, and brain impairments benefit from positive partnerships between therapists and patients.
The results include the ability to perform daily activities, manage pain, complete specific physical function tasks, depression, general physical health assessment, treatment compliance, and treatment satisfaction.
When it comes to patient-therapist interactions, four topics have been examined: interpersonal and communication skills, practical skills, customized patient-centered treatment, and organizational and environmental aspects.
Physical therapists must have effective communication with their patients on several levels. When explaining patients’ illnesses and suggested treatment plans, physical therapists need to take into account that patients have varying degrees of health literacy.
The use of communication strategies that are tailored to the patient’s health literacy level has been shown to improve communication between the patient and their healthcare provider.
Patients also stated that cooperative decision-making will lead to a good connection. Professional expertise and practical skills, such as the ability to educate patients about their conditions, are seen as crucial elements of inpatient care.
When a professional can clearly and confidently communicate their problems, patients value that.
Furthermore, when physical therapists are very proficient in their technical skills and successfully rehabilitate their patients, patients prefer it.
According to recent studies, the physiotherapist should respect the patient, spend adequate time with them, communicate and listen well, explain the treatment in detail, and allow the patient to make decisions on their care.
These are the most important variables affecting the interactions between the patient and the therapist.
Effectiveness
Physiotherapy has been demonstrated to improve pain and function in a variety of musculoskeletal conditions. Patients with lower back pain can benefit from safe spine manipulation by physical therapists.
According to randomized control trials, patients with osteoarthritis of the knee who get both manual therapy and physiotherapist-supervised exercise therapy experience functional improvements and may even avoid surgery.
Another randomized controlled study found that the use of physiotherapy and surgical decompression treatment is increasing.
In addition to stretching exercises, it has been suggested in some studies to be either just as beneficial as or even more successful than surgery in treating Carpal Tunnel Syndrome.
Spine manipulation and therapeutic massage are excellent therapies for neck pain, however, electroacupuncture, strain-counterstrain, relaxation massage, heat therapy, and ultrasound therapy are less effective and therefore not recommended.
Studies show that physical therapy can also help people with a variety of illnesses. Asthma patients may have a decrease in symptoms and medication consumption, along with an improvement in their overall quality of life.
Inspiratory pressure, cardiovascular fitness, and physiotherapy treatment. Because early mobilization can reduce hospital and critical care unit stays and improve long-term functional ability, patients in the intensive care unit may occasionally receive physical therapy.
Adult intubated intensive care unit patients receiving mechanical ventilation can safely and effectively begin early progressive mobilization.
Psychologically informed physical therapy (PIPT) improves patient outcomes, especially before and after spine, hip, or knee surgery.
where patients are treated by a physical therapist and other members of a multidisciplinary care team help with preoperative planning for pain management and quality of life.
Telehealth
The increasing need for physical therapy services led to the development of a new form of physical therapy termed telehealth, also referred to as telerehabilitation.
Telehealth, or online communication between the patient and the clinician, has been evaluated differently from more traditional, in-person care. It can happen in sessions that are pre-recorded or live.
Enhanced accessibility in remote areas, cost-effectiveness, and improved usability for those who are bedridden, housebound, or physically disabled are just a few benefits of telehealth.
Considerations for telehealth include limited evidence of effectiveness, issues with payment and licensing regulations, privacy violations, and compliance, which are more significant than those for in-person therapy.
There is disagreement over research on the effectiveness of telemedicine for people with more serious conditions, such as multiple sclerosis, stroke, and lower back pain.
The interstate agreement, which permits physical therapy to be practiced across state lines, was in effect in 21 US states as of March 2018.
Because patients could not come in person safely during the COVID-19 epidemic, particularly if they were old or had chronic conditions, telemedicine became increasingly important.
As the number of persons who were unable to attend classes decreased, telehealth was seen as a preventative approach. Later physical decline in at-risk people is difficult to cure or reverse.
Platform development or licensing is thought to be the biggest cost in telehealth. Despite telehealth, physiotherapists are still needed to oversee the program.
FAQs
What is meant by physical therapy?
Physiotherapy aids in the restoration of movement and function in those who have been impacted by disease, trauma, or disability. Additionally, it may lower your future risk of disease or damage. It demands an all-encompassing strategy where the patient actively participates in their care.
Are physiotherapists considered doctors?
However, in a 1996 ruling, the Supreme Court (SC) declared that only medical practitioners with an MBBS degree or higher could be “Doctors.” Physiotherapists are not allowed to use “Dr.” as a prefix to their names. Rather, like therapists, they have to register with their council.
Is physical treatment beneficial?
Better mobility, stronger muscles, and pain reduction are just a few of its many benefits. You will engage with a therapist to establish short- and long-term goals once they have evaluated your condition and reviewed your medical history.
What is the significance of physiotherapy?
Physiotherapy (PT) employs a range of methods to help cure diseases, injuries, or deformities. These include massage, heat therapy, exercises, electrotherapy, patient education, and counseling. The medical specialty known as physical therapy, or PT for short, treats orthopedic, neurological, and cardiac diseases.
Is physical treatment superior to going to the gym?
Your physical therapist knows how to optimize your performance given your current goals and limitations, so the 30-minute workout you finish is better than any gym routine. A physical therapist by your side ensures that your exercise routine is successful and keeps you involved.
Referances
- Professional, C. C. M. (2025, January 24). Physical therapy (Physiotherapy). Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/physical-therapy
- Website, N. (2025, April 15). Physiotherapy. nhs.uk. https://www.nhs.uk/conditions/physiotherapy/
- What is physiotherapy? (2023, March 7). The Chartered Society of Physiotherapy. https://www.csp.org.uk/careers-jobs/what-physiotherapy
- Doug. (2025, January 16). What is Physiotherapy – College of Physiotherapists of Ontario? College of Physiotherapists of Ontario. https://collegept.org/patients/what-is-physiotherapy/
- Healthdirect Australia. (n.d.). Physiotherapy. Healthdirect. https://www.healthdirect.gov.au/physiotherapy
- What is physiotherapy? (n.d.). World Physiotherapy. https://world.physio/resources/what-is-physiotherapy