Parkinsonian Gait
Table of Contents
What is Parkinsonian gait?
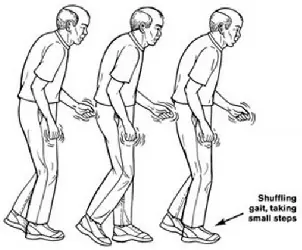
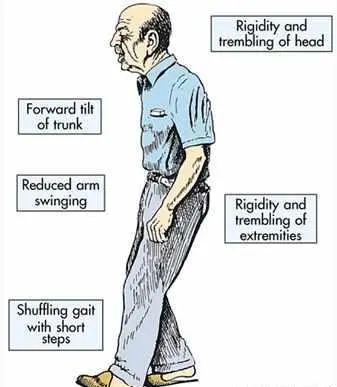
Parkinsonian gait is a type of gait abnormality that is commonly seen in people with Parkinson’s disease. It is characterized by a stooped posture, a shuffling gait, and a lack of arm movement while walking. People with Parkinsonian gait may also have difficulty initiating movement and may experience freezing of gait, which is when they suddenly stop and have difficulty starting again.
Other features of Parkinsonian gait may include a reduced stride length, a slower walking speed, and difficulty with balance and coordination. These symptoms are caused by the degeneration of dopamine-producing neurons in the brain, which are responsible for controlling movement.
There are a variety of treatments that can help manage Parkinsonian gait, including medication, physical therapy, and assistive devices such as walkers or canes. It is important for people with Parkinson’s disease to work closely with their healthcare providers to develop an individualized treatment plan that addresses their specific symptoms and needs.
A distinguishing characteristic of Parkinson’s disease, particularly in later stages, is Parkinsonian gait. Compared to other Parkinson’s symptoms, it is frequently thought to have a worse effect on the quality of life. Parkinsonian gait patients typically move slowly and clumsily. They could find it very difficult when it comes to standing up.
Parkinsonian gait abnormalities might be intermittent or persistent. Episodic alterations, like a freeze of the gait, might appear out of nowhere. Constant gait alterations, such as walking slower than you should, frequently occur while you are moving.
How does it appear?
Along with slowness of movement and tremors, Parkinson’s disease is known for a number of motor symptoms, including Parkinsonian gait.
Parkinson’s disease motor symptoms are caused by a lack of control over movements and trouble launching muscles.
Although the specific characteristics of Parkinsonian gait can vary from person to person. most persons have a few extremely distinctive characteristics. They consist of the following:
going more slowly than is reasonable for someone your age or when your strides shorten and get smaller than they should, which can give the impression that you’re rushing.
Walking with fewer arm movements will result in frequent falls and gait freezing.
Parkinsonian gait characteristics such as festination, stooped posture, and freezing are likely to get worse with time. As you age, your range of motion may change, and you may become less active as a result. This can weaken your muscles and slow your reflexes. This in turn can result in musculoskeletal alterations that exacerbate hunched shoulders and bad posture, raising the risk of falling.
It is simple to lose confidence due to a fear of falling if you start to become less mobile or feel shaky. Seeking advice on how to improve gait is vital because this could have an impact on your social life and quality of life.
Gait training
With your body in the best possible functional condition, physiotherapy seeks to keep you moving safely and on your own. Physical therapists, often known as physiotherapists, are frequently part of multidisciplinary teams, which are groups of experts from many fields who work together to help you manage your symptoms and improve your quality of life.
Exercise and other types of physical therapy are used by physiotherapists to help you maintain your functional independence. Along with working in patients’ homes, physiotherapists also practice in hospital and community settings.
Parkinson’s disease physical therapy’s main objectives are:
- to minimise the danger of falling; to maintain strength and flexibility;
- to maintain a safe walking pattern;
- to maintain and improve functional capacity and independence;
- to correct and improve posture and balance;
- to enhance everyday activities (e.g., getting out of bed and sitting up from a chair); (with or without mobility aids)
- If freezing is apparent, coping mechanisms including auditory or visual cues may be taught to increase manual tasks (reaching and grabbing), maintain respiratory function through breathing exercises, and teach relaxing techniques to educate carers and improve freezing.
The objectives of physiotherapy in Parkinson’s patients will change depending on the stage of the disease being experienced.
Early stage
Preventing inactivity and enhancing physical ability in terms of aerobic capacity, muscle strength, and joint mobility are the main goals in the early stage of the condition. Your physiotherapist could provide you with an exercise regimen to follow, either alone or with others, along with tips and recommendations for keeping up your fitness levels.
Mid-stage:
Physiotherapy at this time will focus on enhancing the use of the upper limbs, particularly in terms of reaching and gripping, as well as posture, balance, gait, and transfers. Your physical therapist might recommend a variety of exercises to assist with these duties, such as hand exercises to improve manual dexterity so you can, for instance, button a shirt more effortlessly. To make your home secure and lower your chance of falling, he or she might also work with an occupational therapist.
Late stage: Physiotherapy at this point seeks to avoid issues that could come from using a wheelchair or being bedridden. In order to do this, you must maintain your breathing, prevent pressure sores, and cooperate with your carers to ensure that you are positioned correctly and that they don’t hurt themselves while lifting you.
Work on Balance

Proper balance is a result of the interaction between your inner ear, which aids in orientation, what you perceive (visual feedback), and how your feet feel the earth under them. Parkinson’s disease can damage this balance system, causing instability in your stride (the way you walk), which may make you anxious in crowded or public places. Walking drills, or gait training, can be beneficial. A physical therapist should supervise any exercises meant to improve balance since they may help you identify any balance problems and teach you workarounds.
Flexibility and stretches
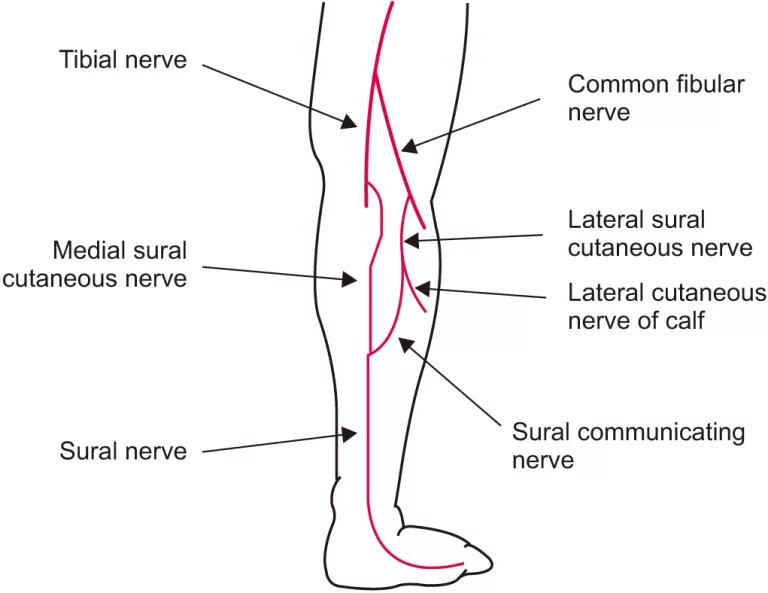
Parkinson’s disease patients frequently have tight hip flexors, hamstring, and calf muscles. It’s important to stretch throughout the day at regular times rather than just once to combat that stiffness. Request instruction from a trained professional specializing in Parkinson’s therapy or training.
Training in Strength
Due to Age-related muscle weakness strengthing training is essential for everyone. Yet, evidence indicates that patients with Parkinson’s disease may experience more difficulties due to muscle weakness. A therapist may ask you to perform resistance exercises with light dumbbells or a resistance band, depending on the stage of the condition you are in (a kind of thick rubber band). Pool-based exercises that use the water’s resistance to build muscle can also be beneficial.
Sensory training
The motor nerve function in your feet and up through the rest of the leg is improved when you walk on a Sensory mat because it stimulates more sensory nerves there.
Besides helping to raise exercise difficulty for advancement, the Sensa mat enhances foot stability.
Have a partner beside you when practicing exercises that require balance, stability, agility, or any other skill where you might feel unsure of yourself.
When necessary, use something to aid your stability, such as sticks, a walking frame, parallel bars, a firm chair, or a wall.
FAQ
PD sufferers typically walk with a narrow base.
Hand, arm, leg, jaw, or head trembling. muscle stiffness, where the muscle is continuously tensed. sluggishness of motion. impaired coordination and balance, which can result in falls.