Referred Pain
Table of Contents
What is pain?
In its most basic form, pain is a bundle of impulses that are carried to the brain for processing. It is compared to an alarm system that sounds to alert you and avoid harm since it is a crucial bodily process for determining whether your body is in danger. To decide whether you will feel pain, the brain has to be able to comprehend a variety of distinct signals.
These consist of:
- Heat (by contacting a hotplate)
- Pressure (resulting in finger cuts)
- Chemical alterations (your eye being splashed with lemon juice)
What is Referred Pain?
Referred pain is pain that is felt at a different location than the location of the pain stimulus/point of origin. It is the result of an interconnected network of sensory nerves that supply many different tissues. When the signal is interpreted by the brain because of damage at one point in the network, it’s likely that the signals are also felt in the nearby neural tissue.
However, it is important to distinguish this from radiating or radicular pain, which is discomfort brought on by abnormal discharges from a dorsal root or its ganglion. Intervertebral disc herniation, spondylosis, spondylolisthesis, or any disorder involving compression of the dorsal root ganglion can all result in radicular discomfort.
Definition
Referred pain, also known as reflected pain, is pain that is experienced away from the site of the painful stimuli. As an illustration, consider the condition of angina pectoris caused by a myocardial infarction (heart attack), in which pain is frequently experienced in the left side of the neck, left shoulder, and back rather than in the thorax (chest), the location of the injury. The phrase has been defined variably by many writers since the International Association for the Study of Pain has not given it an official definition. Since the late 1880s, reported pain has existed. Despite an expanding body of information on the topic, there are many theories regarding the biological mechanism of transferred pain.
Due to the confluence of several distinct nerves at each level at the same place, these pain signals can occasionally become muddled as they reach the spinal cord. Think of it as a “crosstalk” between the nerves, where impulses from a painful joint are combined with signals from a neighboring skin or muscle location. The majority of the time referred pain radiates from the body’s core outward; for instance, the hip may transfer pain to the knee, and the lower back may transmit pain to the legs.
Referred pain can make it seem as though you have a problem in one area of the body while in reality, it is somewhere else. Because treating the site of the referred pain will not solve the issue, a smart clinician should always evaluate to determine if there are any additional places that may be referring to pain.
In our practice, typical cases of referred pain include:
- A person enduring shoulder discomfort due to a neck ailment, such as problems with one of the cervical joints.
- Lower-back conditions that cause leg discomfort (such as sciatica), can occasionally extend all the way to the calf or toes.
- A person with hip arthritis believes that their knee pain is their primary source of discomfort.
Clinically Relevant Anatomy
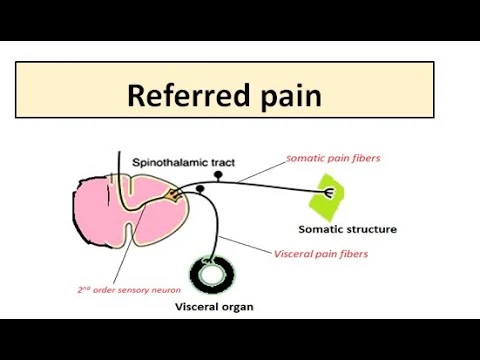
Nociceptive dorsal horn and brainstem neurons may receive convergent input from several organs, according to a number of neuroanatomical and physiological hypotheses. Therefore, higher centers are not able to correctly identify the real source of income. Recent hypotheses have put forth concepts in which the brainstem and dorsal horn neurons’ plasticity is key. Efforts have been made over the last decade to systematically map the regions of musculoskeletal pain indicated in humans.
At the same level of the spinal cord, nerve fibers from lower sensory inputs (such as the stomach) and higher sensory inputs (such as the skin) converge. As a result, stimulation from lower sensory inputs to the brain may be perceived as originating from higher areas, resulting in discomfort localized to the related dermatome of the same spinal segment. This might confuse the brain as to where the feeling or pain is coming from.
The discomfort felt in myocardial ischemia, which is felt in the neck, left shoulder, and down the left arm, is a prime example of this phenomenon. Said pain is caused by the convergence of several primary sensory neurons on a single ascending pathway. When painful stimuli are generated in visceral receptors, the brain cannot distinguish visceral signals from more common somatic receptors. This leads to pain interpreted as coming from somatic areas rather than internal organs.
Imman and Saunders hypothesized that referred pain more usually followed the sclerotomes (muscle, fascia, and bone) than the traditional dermatomes. Clinical and experimental muscle pain has sensory expressions such as generalized aching pain in the muscle, pain transferred to distant somatic structures, and changes in the sensitivity of the superficial and deep tissues in the painful locations. The convergence of nociceptive afferents on dorsal horn neurons is a speculative potential mediator of transferred pain.
Neuro-Physiological Theories
Several neurophysiological theories have been proposed:
Convergence projection theory
It assumes that pain is caused by the convergence of afferent information from organs of visceral and somatic origin in the same segment. Because of this, dorsal horn neurons become hyperactive and are thought to have the same dermatome origin.
Convergent Facilitation Theory
Here, sensory input from lower cutaneous receptors synapses on the same spinothalamic cell body as sensory input from the maxillary nerve.
Axonal reflex theory
The transmission of a skin receptor impulse from the primary axon to surrounding blood vessels in the stimulated skin area is known as an axonal reflex. These pulses release chemicals that cause blood vessels to dilate and leak, causing the skin to sweat and blood vessels to dilate.
Hyperexcitability theory
Thalamic convergence theory
What are the different types of referred pain?
Nerve Pain
In some cases, when the pain signal is sent by a nerve, the pain can be felt along the entire length of the nerve. Patients often describe it as a sharp burning pain along the skin. One of the most common examples of this is sciatica, where a large nerve running down the back of the leg becomes irritated around the lower back. The spine is not far from where the discomfort is coming from. But this pain follows a characteristic pattern in the leg.
Muscle Pain
In other cases, the muscles, not the nerves, redirect the pain. Muscle trigger points are tension bands that develop in muscle tissue when there is abnormal stress. Muscle dysfunction can be brought on by bad posture, inactivity, and overuse. Different pain patterns may emanate from these trigger sites. Trigger points are diagnosed as a source of pain when symptoms recur when the therapist presses a certain point. We are aware that our inside organs may also refer to pain if that wasn’t perplexing enough already. Internal organ pain is generally characterized as a deep discomfort that is typically unaffected by limb or back motions.
Organs frequently disperse pain in extremely hazy patterns and occasionally may not even produce any pain where they exist. For instance, kidney discomfort frequently resembles lower back pain. Tragically, there have been cases of individuals who delayed seeking care because they thought they had a minor backache rather than a dangerous ailment.
Understanding how pain functions is a crucial component of controlling your symptoms. Pain has many other intriguing elements. Speak with your physiotherapist about how referred pain may be impacting you; they can answer any questions you may have. Nothing in this text should be used in place of professional medical advice. Always see a medical expert for guidance on your specific injury.
Causes
Pain emanating from a spinal segment, a sacroiliac joint, viscera, tumors, infections, or concomitant signs are the most typical sources of referred pain.
Additionally, it should be mentioned that the local nerve in this location is always the source of discomfort. For instance, the pain is felt deep inside the ear when the ninth cranial nerve (glossopharyngeal nerve) is affected. This contrasts with the pain that is centered more superiorly when the trigeminal nerve is affected. Simply put, referred pain occurs because your body’s nerves are all interconnected.
Your nervous system sends a signal to your brain when your body receives a stimulus that causes discomfort. The body then receives a signal from the brain informing it that you are in pain. Because of the way your body’s nerves are connected, your brain may occasionally send a pain signal to a place in your body other than the one where the pain originates.
Additionally, pain signals may be delivered to one part of the body as a symptom of a medical condition in another part of the body because of synapses and reflexes perhaps not even being aware of.
The precise process and cause of your body’s reaction are currently being studied by researchers.
The common causes of referred pain
Heart attack
Referred pain is frequently brought on by a heart attack. You may experience referred pain in your shoulders, jaw, and teeth. When your body begins to respond to a blockage in your coronary arteries that may result in a heart attack, discomfort is felt.
Phantom limb pain
It’s typical to experience discomfort that your body believes is coming from the arm, leg, or other limb that was amputated. For instance, pain from an amputated foot may be felt in your upper thigh.
Kehr’s sign
Pain in your shoulder blade is Kehr’s indication. A burst or hurt spleen is especially indicated by this discomfort.
Brain freeze
After consuming ice cream or sipping a milkshake, you could get brain freeze, which is referred to as discomfort.
Heart problems
Resembling a heart attack or angina (chest discomfort brought on by inadequate oxygen to the heart). Chest pains, which you can mistake for heartburn or an upset stomach if you’re suffering a heart attack, can also occur. Additionally, you can have breathlessness and pain in your arm, back, jaw, neck, or other body parts. Make an immediate 911 call if it occurs.
Neck problems
Shoulder discomfort may be brought on by a pinched nerve in your neck or other neck issues.
Belly surgery
You may experience shoulder discomfort if you undergo laparoscopic surgery, which is performed through a small incision on your abdomen to remove your gallbladder, reduce the size of your stomach to aid in weight reduction, or for other reasons. Up to two-thirds of patients who have the operation experience that. Your body may hold on to carbon dioxide in your abdomen after laparoscopic surgery. That could aggravate your spine and nerves, resulting in shoulder discomfort.
Lung problems
Pneumonia or lung cancer are examples of lung issues. Shoulder discomfort may be brought on by lung tumors or edema. You’re experiencing discomfort in your throat and mouth. Your brain and the back of your skull experience the discomfort, albeit your vagus nerve is activated.
Blood clots in your lungs
At first, it may feel like a strained shoulder muscle. However, the discomfort is typically so intense that you can have trouble relaxing or falling asleep. Make a quick call to your doctor if it occurs to you.
Belly problems
These include ovarian cysts, gallstones, pancreatitis (pancreatic inflammation), and ectopic pregnancies (pregnancies that develop in one of your fallopian tubes). Problems in or around your gut might produce discomfort that radiates up to and between your shoulders.
In most cases, you’ll also experience additional symptoms including nausea and excruciating pain in your abdomen or pelvis. Pain in other places, like the shoulder, might strike quickly and seem intense.
Where does it most often occur?
Referral pain can be felt anywhere, making it difficult to properly diagnose. Common areas of reported pain include:
Shoulders and neck
Shoulder and neck pain sign:
- injured spleen
- heart attack
- liver cyst
- Upper back
- Pain in the upper back below and between the shoulders can be a sign that you have a stomach ailment.
Lower back and sides of the body
- Pain on the sides of your back or even near your obliques can be a sign that something is going on in your kidneys or colon.
Teeth and jaws
- Tooth and jaw pain can be a first symptom of a heart attack.
Sign And Symptoms
- The degree and duration of persistent/evoked pain are related to the location of referred pain. It is often characterized as an expanding pressure and is particularly dull, hurting, or gnawing. It is difficult to localize because of how widely it disperses.
- A powerful technique for producing referred muscle pain is a temporal summation.
- The level of referred pain depends on central hyperexcitability.
- Chronic musculoskeletal pain sufferers have larger referred pain zones that are sensitive to experimental stimulation. Patients with persistent musculoskeletal pain frequently experience the proximal spread of referred muscle pain, which is quite uncommon in healthy people.
- A multimodal sensory test procedure should be used during evaluation since modality-specific somatosensory alterations take place in referred locations.
- Since referred pain is not brought on by the compression of nerve roots, there are no neurological signs (such as numbness and paranesthesia) to be observed.
- The length and severity of ongoing/evoked pain have an impact on the extent of transferred pain.
- A powerful technique for producing referred muscle pain is a temporal summation.
- The level of referred pain depends on central hyperexcitability.
- Chronic musculoskeletal pain sufferers have larger referred pain zones that are sensitive to experimental stimulation. Rarely do healthy people experience the proximal spread of referred muscle. pain, which is more common in patients with chronic musculoskeletal pain.
- In preferred regions, there are modality-specific somatosensory alterations, which highlights the value of utilizing a multimodal sensory test regime for evaluation.
- Although it’s not always the case, referred pain is frequently felt on the same side of the body as the cause.
Mechanism
Referred pain has a number of hypothesized mechanisms. There is currently no definite agreement on which is accurate. The thoracic dorsal root ganglia 1-4 hold the cell bodies of the cardiac general visceral sensory pain fibers, which go with the sympathetic back to the spinal cord (5). General visceral afferent (GVA) pain fibers often track sympathetic fibers back to the same spinal cord segments. gave origin to the preganglionic sympathetic fibers in the thorax and abdomen.
The thoracic spinal cord segments 1-4 supply the somatic region of the body, which is where the central nervous system (CNS) interprets pain from the heart as emanating from (5). Myocardial infarction often causes discomfort on the mid or left side of the chest, which is where the heart truly resides. The left arm and the left side of the mouth may also experience discomfort. Rarely, referred pain from a myocardial infarction might appear, and this often happens in elderly or diabetic individuals.
Additionally, the dermatomes of this area of the body wall and upper limb share the same second-order neurons in the spinal cord segments (T1-5) and dorsal root ganglia (T1-5) as the heart’s general visceral sensory fibers. The CNS interprets pain as emanating from someplace on the body wall, such as the substernal region, the left. arm, and hand, or the jaw, but it is unclear whether the pain originates from the body wall or from the viscera.
Convergent projection
One of the oldest hypotheses on referred pain is represented by this. Based on the work of W.A. Sturge and J. Ross from 1888 and TC Ruch from 1961, it was created. Since referred pain is thought to be segmented similarly to the spinal cord, convergent projection hypothesizes that afferent nerve fibers from tissues converge into the same spinal neuron. Additionally, experimental data demonstrates that when referred pain is heightened, local pain (pain at the site of stimulation) is also amplified.
This method has come under fire since it is unable to explain why referred pain begins to manifest later after local pain stimulation. Additionally, experimental data demonstrates that referred pain is frequently unidirectional. For instance, triggered local pain in the anterior tibial muscle transmits pain to the ankle’s ventral region, but there is no experimental evidence to support referred pain traveling the other way. Last but not least, our model predicts that the thresholds for local pain stimulation and referred pain stimulation should be identical.
Convergence-facilitation
J. Mackenzie developed the concept of convergence facilitation in 1893 based on Ross and Sturge’s theories. He thought that the organs inside were not susceptible to outside stimuli. Additionally, he thought that the spinal cord was affected by non-nociceptive afferent impulses, which led to the development of “an irritable focus.” Some stimuli were experienced as referred pain as a result of this emphasis. However, because his theories discounted visceral suffering, they were not universally embraced by critics.
Recently, the concept of central sensitization has given it some newfound legitimacy. After being repeatedly stimulated by peripheral neurons, neurons in the dorsal horn of the spinal cord or the brainstem become more receptive, allowing weaker impulses to trigger them. This process is known as central sensitization. The time needed to develop the central sensitization can be used to explain why referred pain takes longer to manifest in laboratory tests.
Axon-reflex
The afferent fiber may be bifurcated before joining the dorsal horn, according to the axon reflex. Intervertebral discs, skin, and muscles all include bifurcated fibers. However, these specific neurons are uncommon and do not represent the entire body. Additionally, the sensorimotor sensitivity alterations in the location of transferred pain and the delays in the onset of referred pain, as well as the different thresholds for stimulating local and referred pain, are not explained by the axon reflex.
Hyperexcitability
According to the hyperexcitability theory, referred pain lacks a core mechanism. It does, however, mention that there is a dominant primary trait. Animal recordings from the dorsal horn during noxious stimulus experiments showed that referred pain feelings started to appear minutes after muscle activation. A receptive field that was some distance from the initial receptive field experienced pain.
According to hyperexcitability, the opening of latent convergent afferent fibers in the dorsal horn results in the creation of new receptive fields. Then, this signal can be interpreted as referred pain. The dependence on stimuli and the delay in the onset of referred pain relative to local pain are two aspects that are consistent with this mechanism of referred pain. However, the development of new receptive fields, which is considered to be referred to as pain, is at odds with the vast majority of experiments. data from research, even those including investigations of healthy people. Furthermore, referred pain. typically manifests in seconds rather than minutes in humans in contrast to animal models. Some researchers believe that the supraspinal circuits have a mechanism or impact that contributes to this.
Future testing may be able to see the underlying cerebral processing circuits responsible using neuroimaging techniques like PET scans or fMRI.
Thalamic convergence
Thalamic convergence hypothesizes that referred pain is experienced as such because of neural inputs. from the wounded area and the preferred location are combined in the brain rather than the spinal cord. There is a dearth of experimental proof for thalamic convergence. However, research on pain in monkeys found that distinct cortical and subcortical neurons were the culmination of many circuits.
Why Does Referred Pain Occur?
Many medical professionals share your uncertainty about why you might feel pain in a section of your body that isn’t harmed. Why some persons experiencing a heart attack also have jaw discomfort is very difficult to explain.
The human neurological system is flawed, and occasionally the wiring gets crossed, to put it simply this is the most mechanical reason. The receptor pain nerve is interconnected with a large number of other brain neurons in many cases of transferred pain. As a result, many different parts of the body may experience pain if the receptor is triggered.
There are some neurologists who disagree with this view. Numerous referred pain types seem to transfer solely in one way. Consider the situation of a cardiac attack. Even if injuries to the jaw or shoulder might cause heart discomfort, the left chest does not feel painful.
Although referred pain has been acknowledged by medical professionals for millennia, there is no agreement on the underlying cause. There is even less consensus regarding the cause of this phenomenon because it doesn’t seem like nerves producing pain in healthy parts of the body has any evolutionary benefit.
Example
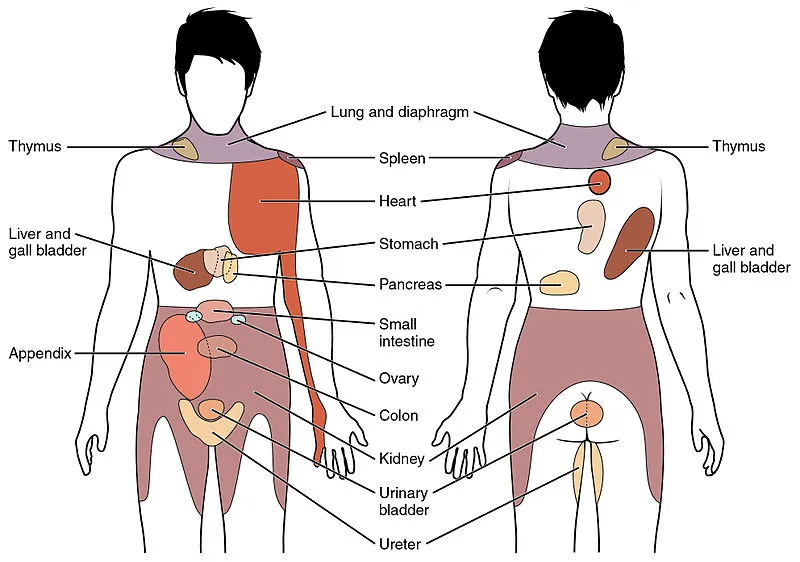
There are several instances of transferred pain, including as
- Cardiac arrest: If you are experiencing a heart attack, your left arm, upper middle back, or jaw may be affected by the pain or numbness that is spreading throughout your body.
- Lung and diaphragm: If you have lung or diaphragm problems, you can have pain in your neck or upper shoulder region.
- Liver or gallbladder: Injury to the liver or gallbladder may cause pain in the neck and upper shoulder region, similar to referred pain involving the lung and diaphragm.
- Pancreas: Back discomfort affects about half of all sufferers of pancreatitis. Some people may also feel tender in their abdomens.
- Colon and appendix: The right middle lower abdomen may be painful in many appendicitis instances.
- The abdomen, pelvis, lower back, upper legs, and any other location where there is a kidney problem might all experience discomfort.
- Ovaries: Serious conditions like ovarian cysts or cancer may result in pain on either side of the abdomen.
- Phantom limb: Some amputees may sense pain in a body part that is no longer there, known as a “phantom limb.”
Laboratory testing methods
Because more control can be exercised there, pain is examined in a lab environment. For instance, far more precise control over the mode, intensity, and timing of painful inputs is possible. There are two basic approaches to studying referred pain in this context.
Algogenic substances
Several different substances, including bradykinin, substance P, capsaicin, and serotonin, have been utilized to produce referred pain in recent years. A solution of hypertonic saline was utilized prior to the widespread usage of any of these drugs. Through numerous trials, it was shown that a number of variables, including infusion rate, saline concentration, pressure, and volume of fluid utilized, connected with the delivery of saline. It is uncertain how the saline causes a pair of local and referred pains. Osmotic variations have been suggested as a possible cause by some studies, however, this has not been confirmed.
Using electrical stimulation
In several experimental and clinical situations, muscle tissue has been subjected to intramuscular electrical stimulation (IMES). IMES systems may be switched on and off, which is a benefit over a standard like hypertonic saline. As a result, the stimulus and response measurement may be carried out with a lot more accuracy and control by the researcher. As it does not require particular instruction on how to be utilized, the approach is simpler to execute than the injection method. Additionally controllable is the electrical pulse’s frequency. For the majority of investigations, both local and transferred pain must be stimulated at a frequency of roughly 10 Hz.
It has been discovered that, when using this strategy, transferred pain requires a substantially stronger stimulation than local pain. The strength of the stimulus and the degree of local and transferred pain are also closely correlated. Additionally, it is thought that using this technique results in greater recruitment of nociceptor units and a spatial summation. The dorsal horn and brainstem neurons get a significantly greater flood of impulses as a result of this spatial accumulation.
Diagnostic Procedures
Because of the disease’s cognitive, emotional, and social elements, studies of clinical pain are constrained by bias. It is particularly challenging to measure and evaluate pain in the therapeutic context since it is a complex and highly individualized experience. Researchers have the ability to regulate the stimulus’s strength, duration, and modality while studying experimental pain. The psychologically elicited reaction to experimental pain can be measured subjectively (for instance, using the McGill Pain Questionnaire) or statistically (for instance, using visual analog scores).
Since endogenous approaches have a high response rate, they are best suited for examining general pain states rather than referred pain. However, they also have the drawback of using several or all muscle groups. Exogenous models are therefore preferable. The intramuscular injection of hypertonic saline is the exogenous model that is most frequently employed. After the infusion, tissues far from the infusion site will experience referred pain. In comparison to local discomfort, it will occur there with a 20-second delay. This pain will be perceived by the sufferer as diffuse and unpleasant. The benefits and drawbacks of hypertonic saline are as follows:
Advantages
- Simple
- Safe
- causes both local and referral pain in the majority of people (40–85%)
Disadvantages
- Prolonged discomfort
Additionally, various allogenic drugs can be employed to induce referred pain, including bradykinin, serotonin, capsaicin, and substance P.
Intramuscular electrical stimulation is a different way to induce referred pain. In contrast to local pain, referred pain requires a much greater stimulus intensity to be elicited, and a statistically positive association has been discovered between the stimulus intensity and the assessments of both local and referred pain severity.
According to the findings, there is a strong association between the assessments of local and referred pain severity and the size of the local and referred pain regions. The extension of referred regions that is observed with an enhanced intramuscular stimulation may also be caused by increased nociceptive input that will go to the dorsal horn or brainstem neurons, which creates an expansion of receptive fields.
Examination
There are several warning signals of transferred pain that should cause you to act right away, even if you might not want to go to the emergency department if you have a brain freeze.
- The fluctuation in the number of anesthetized structures, including skin, subcutis, fascia, muscle, tendons, ligaments, and bone. This is the most crucial need since referred pain sites, particularly visceral referred pain, are frequently discovered to be situated in deep tissues where it is challenging to anesthetize a referred pain site completely.
- The Period of time it hurts and how much.
- The location of the local discomfort (deep structures, viscera, and skin).
- whether the region of transferred pain has sensory alterations (hypersensitivity).
How to Recognise Serious Referred Pain and Take Action?
While you might not want to go to the hospital if you have a brain freeze. There are several warning indications of transferred pain that should make you act right away.
- Heart attack: Always seek medical assistance if you are suffering chest discomfort, but you should be especially worried if you are also feeling pain in your left arm since this might indicate a heart attack. The discomfort may be intermittent, persistent, or abrupt. You could also have discomfort in your upper abdomen, neck, jaw, back, shoulders, or back. You should consider any of these symptoms as a medical emergency and get help as soon as you can. You should be aware that around 14% of those who experience a heart attack will pass away as a result, and many others who survive must deal with the discomfort and weakness of a damaged heart.
- Appendicitis: An appendicitis characteristic pain sign is lower right abdominal pain or discomfort at the belly button. There may infrequently be referred discomfort to the back, lower abdomen, or behind. In order to prevent your appendix from rupturing, which is a potentially fatal condition, you should get to the emergency department as soon as you believe you have appendicitis.
- Ovarian cancer: Some of the early pain signs may manifest in the legs, lower back, or abdomen if the ovaries are affected by cancer. This discomfort might be brought on by a tumor, poor blood flow, kidney or bladder obstruction, or a side effect of some cancer therapies. It goes without saying that you should consult a doctor as soon as possible. if you have any of these pain symptoms.
Use in clinical diagnosis
Referred pain may be a sign of damaged nerves. A sharp ache shot through his arm at the slightest touch. The investigation came to the conclusion that his discomfort may have been brought on by a brain reorganization. following the nerve injury, sensitized areas of his face and back. It is stated that this situation is quite comparable to what people with phantom limb syndrome go through. Based on experimental data acquired by V. S. Ramachandran in 1993, this conclusion was reached, with the exception that the arm that is in agony is still connected to the body.
Orthopedic Diagnosis
From the aforementioned illustrations, it is clear why awareness of referred pain may aid in the accurate diagnosis of a number of disorders and diseases. Physiotherapist Robin McKenzie first used the word “centralization” in 1981. He came to the conclusion that referred pain centralization happens when it shifts from a distal to a more proximal area. During examinations, patients were observed bending backward and forwards, providing evidence in favor of this theory.
According to studies, most individuals with centralization were able to avoid spinal surgery by pinpointing the source of their local discomfort. The individuals who did not suffer centralization, on the other hand, required surgery to identify and address the issues. This finding inspired more investigation into the removal of referred pain by certain bodily motions.
Calf discomfort that is referred to is one illustration of this. McKenzie demonstrated that when the patient repeatedly bent backward in full extension, the referred pain would shift closer to the spine. More crucially, even when the movements were ceased, the referred pain would go away.
General Diagnosis
Similar to myocardial ischemia, referred pain to a specific area of the body can help determine the proper local center. To help in locating the site of pain based on the referred regions, several topographic maps have been created through the somatic mapping of referred pain and the related local centers. For instance, local discomfort induced in the esophagus has the potential to transfer pain to the neck, upper abdomen, and oblique muscles. Localized prostate discomfort may refer pain to in the lower back, calf muscles, and abdomen. As the stone is progressively moved into the excretory system, kidney stones can induce visceral discomfort in the ureter. The lower abdomen wall may experience excruciating referred pain as a result.
Furthermore, sedative ketamine has been shown to have the ability to inhibit referred pain in recent studies. Patients with fibromyalgia, a condition characterized by tiredness and discomfort in the muscles and joints, participated in the study. Due to their heightened sensitivity to nociceptive stimuli, these individuals were examined in particular. In addition, referral pain manifests differently in fibromyalgia patients compared to non-fibromyalgia patients. This discrepancy frequently appears as a difference in the location of the referred pain relative to the local pain (distal vs. proximal). Due to the heightened sensitivity, the region is also significantly more exaggerated.
Treatment
To determine the most effective way to treat your pain, your doctor will need to determine its cause.
Call your doctor if you’ve had shoulder aches for more than a few days without a clear cause. This is crucial if you have severe pain or other symptoms like shortness of breath. Your doctor will inquire into:
- where the pain is felt
- How long it lasted, and whether or not and when it stops
- Your medical background, including any ongoing ailments like high blood pressure
- Any mishaps or injuries that may have contributed to your shoulder pain
- Additionally, your doctor could suggest testing to look for any underlying problems.
Using ultrasound, doctors may quickly examine the muscles, joints, and tendons in your shoulder. To identify issues such as rotator cuff tears.
X-rays, which can identify bone issues.
MRI, which can identify difficulties with your tendons, ligaments, muscles, and other tissues.
Having a CT scan may reveal problems with your bones and some of your tendons.
Blood or other testing, particularly if your doctor thinks your shoulder discomfort is brought on by another medical condition.
Medical Treatment
Numerous investigations have discovered a correlation between the site of the referred pain and the severity and duration of the muscular pain, which is consistent with what has been observed for cutaneous secondary hyperalgesia.
The use of NMDA-receptor antagonists (ketamine) is the most effective treatment for persistent musculoskeletal pain; it produces better outcomes than utilizing traditional morphine management.
Additionally, putting a topical anesthetic eutectic combination to the skin directly above the location of referred pain decreased that area’s suffering by 22.7%. After spraying ethyl chloride into a saline-induced referred pain region, a similar outcome was seen.
To stop all afferents from the referred pain region, there are two methods:
Differential nerve blocking between the stimulation location and the appropriate distal referred region using an inflated tourniquet
Analgesia regionale intravenosa
As a result, the severity of the referred pain decreased by 40.2%.
Other methods of pain management include:
- Acupuncture
- methods used in osteopathic manual medicine
- injections at trigger points
- Laser treatment
- Stretching combined with superficial dry needling is the most efficient.
Physical Therapy Treatment
The major focus of physical therapy management for referred pain syndrome will be pain mechanisms and how to address them. It will have significant symptoms and vary from person to person. Among the methods that may be applied to control pain are:
- Massage with dry needling
- the use of heat or ice
- electrical nerve stimulation transcutaneously
- Spraying with ethanol and the stretch maneuver
- Ultrasound Manual strategies
- Exercise
The majority of the time, treating the underlying medical problem is the best course of action for treating referred pain sensations. However, there are methods for managing the referred pain sensations on their own if the medical problem is resistant to therapy.
Other Medical And Physical Therapy Treatment
- Medication: Aspirin or Tylenol, which are available over the counter, maybe the first medication your doctor prescribes for you. However, if your referred pain feelings continue and become particularly severe, you could be prescribed morphine or ketamine.
- Acupuncture: It is frequently advised for various pain disorders, despite the fact that it has only lately received acceptance from the pain specialty field due to its low cost and minimal risk of adverse effects.
- Heat and ice: Short-term applications of heat and cold can help reduce the symptoms of pain. The warmth stimulates blood flow, which speeds up healing while chilling the injured region can dull the nerves.
- TENS: Transcutaneous Electrical Nerve Stimulation (TENS), which involves applying a moderate electrical current. It can block pain signals and stop the transferred pain’s original source from sending a nerve impulse.
- Exercise: If the referred pain is persistent in nature, your doctor could advise making some lifestyle adjustments, such as engaging in regular exercise. Your doctor could advise low-impact exercise like yoga, walking, or swimming depending on the specifics of your referred pain issue. Exercise should not only help you feel better immediately since endorphins are created, but it should also enhance your general health.
Physiotherapy for referred Shoulder Pain.
For the treatment of referred shoulder pain, physiotherapy is crucial. Your physiotherapist can initially pinpoint the precise source of your pain, the injured tissue or tissues, and the degree of this damage. Using this information, they may devise a precise treatment plan and predict how long the injury should take to recover. The latter frequently includes a series of targeted, gradual strengthening exercises as well as modifications to activity, job, or training as well as electrotherapies, and manual methods including massage, manipulation, and stretching. These exercises can lessen the likelihood that you will experience referred pain in your shoulder in the future, help you recover to regular activities more quickly, and avoid reinjury.
Other methods of treating transferred shoulder pain include:
- Rearranging the body’s posture
- Taping
- Ergonomic assessment
FAQs
When there is local pain, the site of the nociceptive stimulation is also the site of pain perception. The severity of the pain then increases as pressure or stress is applied to this local site. Neuropathic pain, in which the pain is felt in the nerve’s distribution, is distinct from referred pain.
Referred pain, also known as reflected pain, is pain that is experienced away from the site of the painful stimuli.
When there is radiating pain, the discomfort spreads throughout the body. The body is physically moved by the agony. Referred pain doesn’t have a moving or growing pain source. Simply put, the pain is felt elsewhere than where it originated.
The sciatic nerve regulates the leg and foot’s feeling and functionality. Prolapsed or “slipped” discs commonly bulge and push on the intervertebral nerve(s) in sciatica. Referred pain is produced when the nerve is irritated by this pressure. Most sciatica cases go away on their own between six weeks to three months.
Referred pain is frequently brought on by a heart attack. You may experience referred pain in your shoulders, jaw, and teeth. When your body begins to respond to a blockage in your coronary arteries that may result in a heart attack, discomfort is felt.
Referred pain can result from a number of illnesses, including inflammation, back pain, neck pain, and general sickness. For instance, discomfort from a heart attack may be felt in the left arm, whereas discomfort from gallbladder problems may be felt in the right shoulder.







One Comment