Pulmonary Rehabilitation
Table of Contents
Introduction
Pulmonary rehabilitation is a comprehensive program designed to improve the physical and emotional well-being of individuals with chronic respiratory conditions. It plays a crucial role in the management of various pulmonary diseases, including chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease, and pulmonary hypertension. This structured and multidisciplinary approach aims to enhance lung function, reduce symptoms, and improve overall quality of life for those living with chronic respiratory issues.
Pulmonary rehabilitation typically involves a combination of exercise training, education, and psychosocial support tailored to the unique needs of each patient. The primary goals are to optimize lung function, increase exercise tolerance, and empower individuals with the knowledge and skills to better manage their condition on a day-to-day basis.
- The American Thoracic Society and the European Respiratory Society defined pulmonary rehabilitation in 2013.
- Patients with chronic respiratory issues can benefit from pulmonary rehabilitation, which consists of an Exercise and education program. Our physiotherapists and respiratory experts collaborate closely.
- We evaluate every patient separately, enabling us to make sure that your exercises are properly adapted To your needs.
We treat patients with a range of respiratory diseases, not just one or two.
- COPD
- Idiopathic pulmonary disease
- Bronchiectasis
- The goal of PR is to improve respiratory function and, by extension, quality of life (QOL) and participation In daily activities for those who have recently experienced an exacerbation. When compared to standard Care, PR has been shown to significantly enhance health-related QOL and exercise capacity in people With chronic obstructive pulmonary disease (COPD).
- According to studies, PR is beneficial for people with Mild to severe COPD. Although it is unknown whether these advantages continue after this time period, People with COPD who undergo PR are expected to use healthcare services more efficiently during the Next 12 months.
Specify Pulmonary Rehabilitation
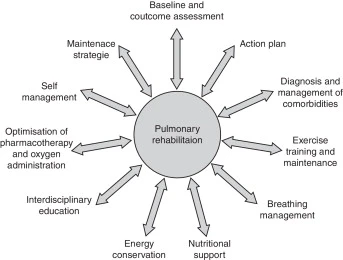
Depending on the resources available, PR programs differ from person to person and center to center, but Generally speaking, they will include:
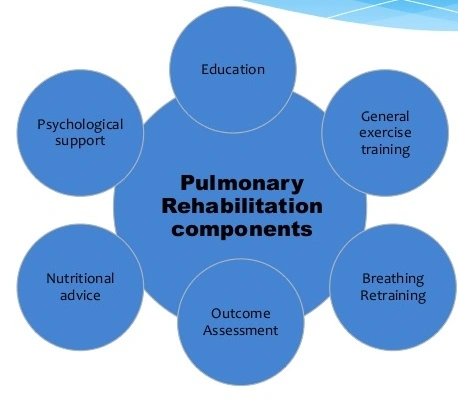
Contributions from multiple disciplines
- Exercise
- Diet plans
- Disease awareness
- Psychological support
- Behavioral modification
A typical session involves a group of COPD patients attending a class at a gym or community center where They engage in supervised exercise under the supervision of a physiotherapist. They then participate in an Educational session with a teacher (usually a nurse or allied health professional) on a variety of subjects, Including managing COPD, using bronchodilators, nutrition, stress, and anxiety.
Structure
- The duration of structured Pulmonary Rehabilitation programs might range from 6 to 8 weeks to a year. A Minimum of 12 supervised sessions over a period of six to twelve weeks with twice-weekly supervised Exercise sessions (plus a third unsupervised session) is advised by the British Thoracic Society. PR can Be situated in the community, a hospital, or both. According to research, inpatient PR had greater results Than community PR when using the Chronic Respiratory Questionnaire, which assesses dyspnea, Fatigue, emotional function, and mastery. After completing PR, it is advised by guidelines that people be Given access to some form of fitness program.
Adherence
- NICE recommendations advise stressing the significance of PR adherence to people in order to improve QOL and respiratory function. Optimizing access to PR, which includes convenient class schedules, Proper physical access to facilities, good public transportation linkages, and prompt referrals to PR, is one Strategy to specifically increase adherence.
Maintenance
- To preserve improvements in pulmonary function, exercise tolerance, and QOL after PR, guidelines advise Maintaining an exercise regimen. In persons with moderate-to-severe COPD, improvements made Following an eight-week outpatient PR program can be maintained with a maintenance program at the Two-year follow-up. Participants in this study maintained higher levels of performance in the 6-minute walk Test, body mass index, airflow obstruction, dyspnea score, and exercise capacity tests.
- The exercise Component of the maintenance program includes home cycle ergometers and twice-a-month hospital-Based supervised exercise sessions. This maintenance program had a 66% compliance rate.
Contraindications
The NICE recommendation states that the following people shouldn’t receive PR:
- Individuals who are unable to walk
- Individuals with unstable angina
- Myocardial infarction
Pulmonary rehabilitation advantages
The advantages of pulmonary rehabilitation are well documented, and it has been demonstrated to improve Quality of life when used in conjunction with other therapies. Previous clients reported that it assisted them With:
- Increasing assurance
- Increasing your awareness of your lung condition
- Gaining knowledge from a variety of health professionals
- Assisting in reducing shortness of breath
- Increase your capacity for activity and level of fitness
- The Freeman Hospital, Royal Victoria Infirmary, and Kenton Park Sports Center all offer this service.
Considerations
Other elements to take into account are:
- Unstable heart condition
- Motor problems
- Instructions with difficulty due to cognitive or mental health issues
- The presence of a support person to facilitate and promote compliance
Intervention
Physiotherapists are crucial in the prescription, supervision, and evaluation of exercise results. According to Research, more people are prescribing exercises based on guidelines (using the FITT methodology, or Frequency, Intensity, Time, Type) than ever before. In comparison to standard care, participants who Exercise both maximally and functionally exhibit statistically significant benefits after PR.
- Positioning, workouts, use of a bronchodilator, etc.
Functional training is crucial in cases of advanced illness, excessive weakness, or exhaustion.
- Change the surroundings for more comfort
- Workspaces supported in practical locations to prevent bending
- Find a table to move large objects on while working.
- Bathtubs in addition to chairs at stair landings
- Utilizing assistive technologies and adaptable equipment
- Providing adequate ventilation in areas with emissions, such as kitchens
Tasks that affect performance:
- Slow tempo
- Minimize jerky motions of the body
- Plan your work to include relaxation and breaks.
Include symptom-relief techniques:
- Keep your breathing rhythm consistent and avoid Valsalva
- Avoid talking incessantly while working.
- Senior people can pace while performing lifting chores when they have an obstructive pulmonary illness; They can also lean forward (which increases intra-abdominal pressure, pushes the diaphragm up into a More favorable position, and enables the auxiliary muscles of inspiration to draw the chest into Inspiration).
- Rapid, shallow breathing is made simpler by restrictive lung disease (which prevents the respiratory System’s elastic resistance).
- Using biofeedback, one can relax non-respiratory muscles and lessen anxiety caused by dyspnea.
Exercise-specific Intervention
Progression-based weight training and supervised aerobic exercise should both be prescribed.
Goals should be developed and agreed upon, and exercises should be recommended individually based on The first assessment. Regular monitoring of participant effort is advised, with a focus on any chest pain, Discomfort, or dyspnea.
- For Minor pulmonary condition
The latter can be measured using the BORG scale. See here for suggestions on how to work out.
- Cough, sputum: Extremely effortful symptoms
- Spirometry: Display the anticipated Vital Capacity (VC), FEV1 (Forced Expiratory Volume in the First Second), which is between 70 and 80 percent
- ABG: moderate hypoxemia that is normal
- Exercise evaluation and training, suggested individual workouts, no need for formal rehabilitation
- Pertaining to mild lung disease
2. For Moderate lung disease
- Shortness of breath during regular activities is typical in patients with moderate lung disease.
- Acute pneumonia episode following major surgery is when the pulmonary illness is discovered, showing Promising results with PR
- VC and FEV1 55-70% (signifies breathing difficulty at approximately 3–4 METS)
- Exercise testing: Perform a 12-minute walk test or start at a low Metabolic Equivalent (MET) of 1.5 MET And increase it by 0.5 MET at each stage while monitoring ECG, BP, and HR.
Exercise guidelines:
Intensity: HR during a time when the patient’s dyspnea is rated as 2-3 on the Borg’s scale of perceived Exertion
- Repeatedly, 5-7 times each week
- Use O2 if symptoms appear.
3. For Serious Lung Illness
- Exhalation problems during the majority of daily activities
- 50% for VC and FEV1
- At rest, one needs oxygen.
- Some people exhibit R ventricular dysfunction.
- Exercises set at a steady endurance test of 2-3 METs or low-level intermittent tests are testing options.
Training: interval training, five times per week, once a day, 20 seconds of exercise followed by frequent Rests.
Close supervision: Every 3% drop in SPO2 should be observed when monitoring oxygen levels. When the SPO2 drops below 88%, oxygen therapy is advised.
How to set up an Exercise Programme
1) Recognize your limitations
- Make sure you possess the information and abilities necessary to instruct, inspire, and motivate the Students who attend your classes.
2) Identify the product’s unique selling proposition
- Patients with pulmonary pathologies might benefit from a wide variety of activities, and they frequently Gravitate toward a particular exercise. This could involve an aerobic activity like cycling, walking, or Rowing. Others, on the other hand, like activities that combine a variety of exercises, such as cross-Training or high-interval intensity training, being outside, or honing abilities, like dance or hiking.
- Find a market that will draw customers to your desired location and motivate them to stay there.
3) Begin small and progress
Level A counts the participants first, then the number and size of the class.
- Promote through community-based organizations
- Promote your organization to neighbors, coworkers, family, and friends. Try putting up flyers or using Posters to promote local businesses at the YMCA, library, community center, gym, or place of worship in Your town.
- Join and participate in Facebook groups focused on fitness or even just local communities with members In your target market.
- Publiciseonline
- Create a presence online, whether through websites, blogs, or social media.
- Connect with engaging, memorable brand hashtags.
- Good music gives listeners the option of two favorite playlists or a recent hit song
- Make it socially acceptable to promote others:
- Partner exercises (which we’ll talk about more below)
- Making it quite apparent that, despite the fact that everyone is there for different reasons, they should all Work hard as a team to get fit.
- Celebrate achievements. Celebrate when your team achieves its objectives. This can be as easy as going For a cup of coffee after working out.
Level B. Build Intensity
- Start with minimal reps, sets, and loads.
- Encourage patients to pay attention to their bodies and build up carefully.
What takes place during pulmonary rehab?
Your medical team may carry out one of the following tests to assist in creating your pulmonary rehabilitation Plan:
- Exercise stress test to gauge your blood pressure, heart rate, and oxygen saturation while you work out
- Breathing examinations to evaluate the health of your lungs
- Measure your walking distance in six minutes with the six-minute walk test.
- In addition to learning physical therapy or breathing exercises that you can practice at home, you may receive pulmonary rehabilitation in a hospital or clinic. You might also employ smartphone-based course monitoring or activity trackers.
The following instructions and training could be part of your pulmonary rehabilitation plan:
Breathing techniques
- You can pick up particular breathing exercises like pursed lip breathing, yoga breathing, or computer-assisted feedback. Especially when you are physically active or under stress, you may better control your Breathing and prevent feeling out of breath by using these tactics. You might also pick up some tips on How to get rid of lung mucus.
Education
- Your healthcare professionals can provide information on your lung disease and suggestions for managing It in group or one-on-one sessions.
- You might discover more about how the lungs function as well as the best ways to take your medications.
- In order to prevent or manage a flare-up, you could learn to spot its early symptoms.
- Your group might be able to assist you in quitting smoking.
- By discovering simpler ways to complete daily tasks, you may learn how to preserve your energy and Prevent being out of breath. This might involve finding techniques to prevent bending, lifting, and reaching As well as coping mechanisms for stress.
- Psychological guidance
- People who have a chronic (long-term) lung condition may often struggle with mental issues including Anxiety and despair. Training in stress management can be provided through individual or group support.
Exercise training
- Exercise training seeks to improve your arms, legs, back, and the breathing muscles you employ. You can Practice exercises to increase your flexibility and stamina, which will make it simpler to perform daily jobs And activities you enjoy.
- Your medical team may advise utilizing medication to clear your airways or modifying your usual oxygen Therapy while engaging in physical activity.
Nutritional guidance
- In order to manage your illness and feel your best, you will learn what foods to eat and how to prepare Meals. You can help ensure that you are getting the essential nutrients in the right amounts by seeking Nutritional guidance. In order to help you gain muscle mass, a dietitian may also suggest a weight-loss Strategy, dietary supplements, or medications.
How long is a program of pulmonary rehabilitation?
- Pulmonary rehabilitation often consists of two to three sessions per week spread out over a few weeks or Months.
- Your healthcare team will do tests to examine your lung function once more at the conclusion of your Program to see if your breathing has improved. There will be some of these tests that you already took at The beginning of your program, such as the exercise tests.
FAQ
What function does a physiotherapist play in lung rehabilitation?
In order to increase activity and improve the quality of life in individuals with chronic respiratory Conditions, physiotherapy is crucial. The physiotherapist conducts an evaluation, taking into account Not only breathing issues but also the impact of other conditions on their ability to breathe and general Health.
Exercises for pulmonary rehabilitation are what? Or What Exercises Can You Do at Home for Pulmonary Rehabilitation?
7 Home Exercises for Pulmonary Rehabilitation
Breathing from the belly. COPD is a frequent factor in people enrolling in pulmonary rehab programs.
Lips pursed, breathing.
Lifting weights.
Arms are raised.
Leg elongations.
The Tai Chi.
Stretching gently.
What three elements make up pulmonary rehabilitation?
Pulmonary Rehabilitation Elements
Symptoms like breathlessness can be made better.
Restore the lungs’ capacity for function.
Boost your standard of living.
How is pulmonary rehabilitation equipment used?
The majority of pulmonary rehabilitation programs take place in hospital gymnasiums and may make Use of weight machines for resistance training as well as treadmills, stationary bikes, arm and rowing Ergometers, and other aerobic exercise equipment.
Which four pulmonary rehabilitation techniques help to cleanse the airways?
The four main elements of comprehensive pulmonary rehabilitation programs are typically as follows:
Exercise instruction.
Education.
Behavioral and psychosocial intervention.
Outcome evaluation.
Which methods are employed in pulmonary physical therapy?
The active cycle of breathing techniques, positive expiratory pressure devices, breathing exercises, Percussions, and chest and abdominal muscular exercises were the most frequently employed Pulmonary physical therapy procedures.
Reference
- Pulmonary Rehabilitation. (n.d.). Physiopedia. https://www.physio-pedia.com/Pulmonary_Rehabilitation
- Shenoy, M. A. (2023, July 25). Pulmonary Rehabilitation. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK563166/
- Pulmonary Rehabilitation – http://www.physiofit.in. (2020, August 4). http://www.physiofit.in. http://www.physiofit.in/pulmonary-physiotherapy-rehabilitation/The Basics of Pulmonary Rehabilitation. (n.d.). https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/pulmonary-rehab
- Pulmonary Rehabilitation. (n.d.). Cystic Fibrosis | COPD | MedlinePlus. https://medlineplus.gov/pulmonaryrehabilitation.html