Oculopharyngeal Muscular Dystrophy (OPMD)
Table of Contents
What is Oculopharyngeal Muscular Dystrophy?
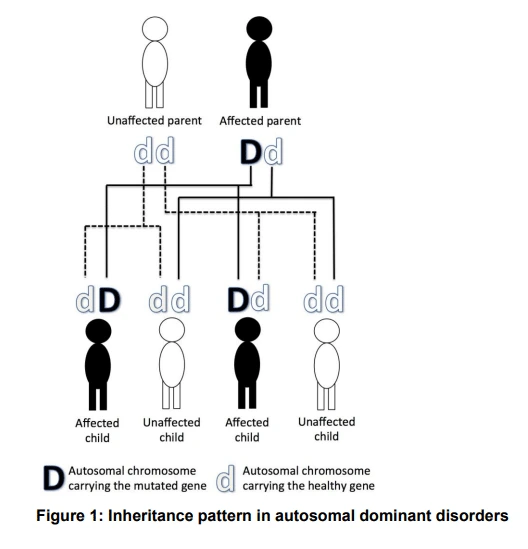
Oculopharyngeal genetic disorder (OPMD) could be a rare kind of genetic disease with symptoms generally starting when a person is 40 to 50 years old. It is often autosomal dominant neuromuscular disease or autosomal recessive. the foremost common inheritance of OPMD is autosomal dominant, which implies just one copy of the mutated gene has to be present in each cell. Children of an affected parent have a 50% chance of inheriting the gene.
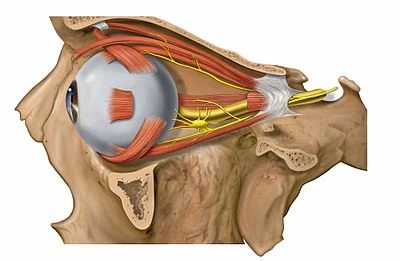
The term “oculopharyngeal” refers to the eyes (ocular-) and part of the throat called the pharynx (-pharyngeal). Affected people generally first feel the weakness of the muscles in both eyelids that causes droopy eyelids (ptosis). Ptosis can aggravate over time, causing the eyelid to weaken vision, and in some cases, limit eye movement, together with ptosis, affected people develop weakness of the throat muscles that causes difficulty swallowing (dysphagia). Dysphagia begins with dry food, but over time, liquids can even become difficult to swallow. Dysphagia can cause saliva to collect and a wet-sounding voice. many of us with the oculopharyngeal hereditary disease even have weakness and wasting (atrophy) of the tongue. These problems with food intake may cause starvation, choking, or a bacterial lung infection called bronchopneumonia.
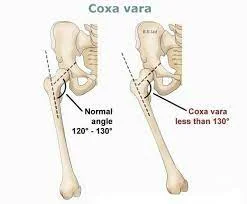
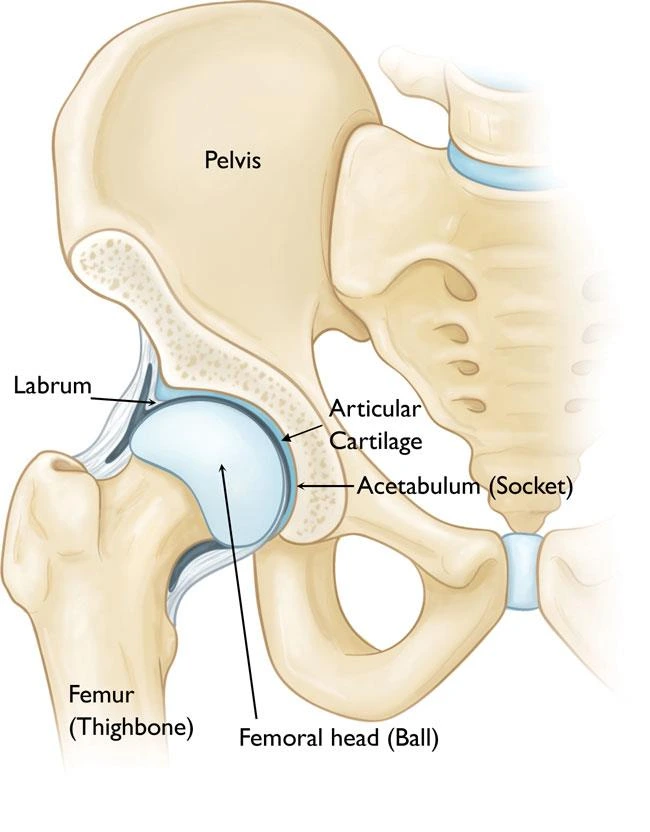
Individuals with oculopharyngeal dystrophy frequently have weakness within the muscles near the middle of the body (proximal muscles), particularly muscles within the shoulders, upper legs, and hips (limb-girdle muscles). The weakness slowly gets worse, and folks may have the help of a cane or a walker. Rarely, affected individuals need wheelchair assistance.
Rarely, do individuals have a severe variety of oculopharyngeal inherited disorders with muscle weakness that begins before age 45 and have trouble walking independently by age 60? These individuals often even have disturbances in nerve function (neuropathy), a gradual loss of intellectual functioning (cognitive decline), and psychiatric symptoms like depression or strongly held false beliefs (delusions).
Autosomal dominant inheritance is the most typical variety of inheritance. Less commonly, OPMD may be inherited in an autosomal recessive pattern, which suggests that two copies of the mutated gene must be present in each cell, both parents must be carriers of the mutated gene, and frequently show no signs or symptoms. The PABPN1 mutation contains a GCG trinucleotide repeat at the 5′ end of the coding region, and expansion of this repeat then results in autosomal dominant oculopharyngeal inherited disorder (OPMD) disease.
Causes of Oculopharyngeal Muscular Dystrophy
OPMD is caused by a genetic problem. the matter is from a gene that has the knowledge needed to form a protein called polyadenylate-binding protein (PABPN1). The defect results in a buildup of PABPN1 within the muscle cells. The PABPN1 clumps inside the muscle cells and should cause the cells to die. This results in muscle weakness.
The defective gene that causes OPMD is moved down from a parent to their child. Most often, someone with the disease has only 1 copy of the gene defect. In some cases, an individual might get two copies of the gene, one from each parent. this could cause more severe OPMD. The disease will aggravate more quickly.
Mutations within the PABPN1 gene cause oculopharyngeal genetic disease. The PABPN1 gene provides instructions for creating a protein that’s found throughout the body. The PABPN1 protein plays a vital role in processing molecules called messenger RNAs (mRNAs), which function as genetic blueprints for creating proteins. PABPN1 alters a part at the tip of mRNA molecules that protect mRNA from being lessened. The PABPN1 protein is also involved in transporting mRNA within the cell.
The PABPN1 protein contains a part where 10 copies of the protein building block (amino acid) alanine occur during a row. This stretch of alanines is thought of as a polyalanine tract. The role of the polyalanine area in normal PABPN1 protein operation is unknown. Mutations within the PABPN1 gene that cause oculopharyngeal inherited disorder to lead to a PABPN1 protein with an abnormally long (extended) polyalanine tract that features between 11 and 18 alanines. Typically, affected individuals with shorter polyalanine tracts tend to possess milder signs and symptoms that develop later in life compared to those with longer polyalanine tracts. the additional alanines cause the PABPN1 protein to create nonfunctional clumps within muscle cells. These clumps (called intranuclear inclusions) accumulate and are thought to impair the conventional functioning of muscle cells, eventually causing death. The resulting loss of muscle cells over time presumably causes muscle weakness seen in people with oculopharyngeal inherited disease. In severe cases, it’s likely that intranuclear inclusions affect nerve cells similarly to muscle cells.
Genetics
OPMD is thanks to a mutation of the pABPN1 gene, which was first described in 1988. The mutation leads to an expansion of the alanine (GCN; denoted in and of itself because four different codons – GCA, GCT, GCC, and GCG – can encode the organic compound alanine) repeat region on chromosome 14q11.2. This region is an element of the polyadenylate-binding protein nuclear 1 gene (PABPN1, previously abbreviated as PABP2) N-terminus. PABN1 has regulatory functions within the polyadenylation of template RNA. The N-terminal domain is often (GCN)10 (denoted (GCN)10/Ala 10) but the length of the alanine expansions range from +1 to +8. The mutation is stable across generations and doesn’t exhibit genetic anticipation.
Common mutations sorted by prevalence are:
GCN)13, the foremost common dominant mutation in Quebec and worldwide
(GCN)11, a recessive polymorphism that’s carried by 1-2% of North American, European and Japanese individuals. It causes a more severe phenotype when a patient could be a compound heterozygote with both the (GCN)13 and also the (GCN)11 variants
Rare homozygote cases that carry two dominant mutations inherited from their two affected parents that have a far more severe phenotype
Although the inheritance pattern is often autosomal dominant, an allelic autosomal recessive form has been documented (see common mutations above). In cases of autosomal dominant OPMD, while even one mutation is sufficient to cause disease, occasionally, both alleles are mutated which ends up not only in an earlier manifestation of the disease but faster and more severe progression in addition. In autosomal dominant patients, every child of a heterozygous carrier features a 50% chance of inheriting the disease-causing mutation. there’s nearly a whole penetrance pattern with an increased risk of presentation with increased age. most people with the mutation have presented by the 7th decade of life (with average onset within the 5th decade). For those with an autosomal recessive mutation, the offspring are going to be obligate heterozygote (carriers) but their risk of being affected is smaller amount than 1% given the two carrier rate for the (GNC)11 recessive allele.
Pathophysiology
The PABPN1 gene is liable for the integrity and transport of mRNA in striated muscle cells throughout the body, preserving its integrity and performance. In patients with PABPN1 mutation, the fragility of mRNA is increased leading to clumps intracellularly. These clumps (intranuclear inclusions) lead to progressive somatic cell dysfunction, eventual death, and thus progressive clinical muscle dysfunction.
In addition to genetic testing, a muscle biopsy could also be helpful in the diagnosis of OPMD. The presence of intranuclear inclusions (INI) in myonuclei could be a specific histologic hallmark of OPMD. Per slide, INI containing PABPN1, and lots of other RNA-binding proteins, may be seen by microscopy as tubular filaments in 4-5% of skeletal muscle nuclei of OPMD patients. it’s not known what’s the reason for OPMD but the hypothesis is that the pathology is caused by either 1) the clumping proteins (INI), or 2) the dearth of the traditional protein. Clinically unaffected muscles may additionally have histologic findings, like rimmed vacuoles and ragged red fibers, that indicate a dystrophic pathology (but the findings within the unaffected muscles don’t seem to be specific to OPMD).
How to manage oculopharyngeal muscular dystrophy?
A speech-language pathologist SLP can teach you ways to handle speech or swallowing problems associated with OPMD. These may include swallowing techniques and methods for talking. An occupational therapist can facilitate you with flexible methods for daily tasks. you’ll also find a cane, walker, or other walking aid helpful if the OPMD affects your leg muscles.
It’s important to figure along with your healthcare team to handle any swallowing issues. Strategies like changing the feel of food, taking smaller bites, or holding your head in certain ways while swallowing could also be helpful. you will have to have a procedure to create swallowing safer and lighter. you will have to see a nutritionist to form sure you get enough nutrition if you employ a feeding tube.
Symptoms of Oculopharyngeal Muscular Dystrophy
The condition generally affects the muscles within the upper eyelids and throat. you’ll first notice drooping eyelids or trouble swallowing. Most of the time, OPMD gets worst very slowly.
Common symptoms include:
- Eyelid drooping is could be enough to want special glasses to brace the eyelids open or surgery to boost the eyelids.
- Choking or swallowing problems (dysphagia). Dry foods could also be the primary to cause of trouble. But swallowing liquids can later be a challenge.
- Tongue shrinking
- Pooling of saliva
- Facial muscle weakness
- Leg and arm weakness
Terms of the signs (and symptoms) of oculopharyngeal inherited disease would be according to the following:
- Ptosis
- Weakness of the extraocular muscles
- Dysphagia
- Aspiration pneumonia (complication)
- Proximal limb weakness
Though the aforementioned signs/symptoms are the foremost common, there are cases though rare, where the peripheral systema nervosum has had involvement with a significant reduction of myelinated fibers.
In homozygous cases, this congenital disease is severe and starts earlier in the affected individual’s life.
Diagnosis of Oculopharyngeal Muscular Dystrophy
The clinical features of oculopharyngeal Muscular Dystrophy (OPMD) intersect with features of several other neuromuscular diseases, making the diagnosis a challenge. A doctor may begin to suspect an OPMD diagnosis based upon clinical evaluation, an in-depth patient history, and identification of characteristic findings, like droopy eyelids (ptosis), difficulty swallowing (dysphagia), and difficulty speaking (dysarthria).
A diagnosis of OPMD is often confirmed through commercially available blood tests that detect the precise genetic disorder within the PABPN1 gene, referred to as a repeat expansion, that’s related to OPMD. The PABPN1 gene normally contains 10 repeats of a selected DNA sequence (GCN), but the mutated versions of the PABPN1 gene cause OPMD to contain an expanded number of GCN repeats. The blood tests want to confirm an OPMD diagnosis and detect the expanded numbers of GCN repeats within the mutated PABPN1 gene.
Sometimes, a person with suspected OPMD is found to own two normal copies of the PABPN1 gene. during this case, muscle biopsy is also wont to detect the subtle histological features of OPMD. Because the PABPN1 gene is a blueprint for the PABPN1 protein, mutations within the PABPN1 gene cause the formation of abnormal PABPN1 proteins that form clumps in muscle cells (intranuclear inclusions or INI). These clumps accumulate and are thought to impair the conventional functioning of muscle cells, and possibly nerve cells additionally. INI is highly specific to OPMD; other common biopsy findings in patients with OPMD that are less specific include variation within the diameter and appearance of muscle fibers, ragged red fibers, and rimmed vacuoles.
Therefore, the presence of those features in a very muscle biopsy is mostly employed in concert with other factors to assist confirm an OPMD diagnosis.
Why do eyelids droop?
There is a variety of reasons that lids might sag. In most cases, eyelid droop either appears in childhood and is said to be a genetic condition, or it happens gradually as muscles stretch out.
Whether or not droopy eyelid exercises improve your lids may depend upon which of those conditions are the cause:
- age, which causes v, muscles, and skin to become weaker, lose volume, get more improvident gradually
- incorrect placement of Botox injections which partially paralyze the muscles within the eyebrow or lid
- glaucoma eye drops cause fat loss within the eye area
- myasthenia gravis, which could be a disease marked by fatigue and lack of muscle control
- third nerve palsy, a condition within which a nerve involved in the movement of your eye is broken
- neurological or paralytic disease
- eye injury
- autoimmune conditions
- diabetes
- stroke
Treatment of Oculopharyngeal genetic disorder
Medical Treatment
If sagging lids interfere together with your ability to work out or function, and exercises for droopy eyelids haven’t solved the matter, you’ll be able to speak along with your doctor about medical treatments.
Dysphagia
Difficulty swallowing, or dysphagia, can cause an individual to aspirate food or liquid into the lungs, which successively may result in a significant problem called bronchopneumonia. If you discover that you’re choking frequently while eating or drinking, you’ll have your swallowing abilities evaluated by knowledgeable. There is a variety of techniques that will help treat dysphagia, starting from holding the top in numerous positions to changing the consistency of foods and liquids. The commercial thickener may give liquids a more compliant consistency. In advanced cases, a nonsurgical procedure called throat stretching or a surgery called a cricopharyngeal myotomy is also warranted. Tube feeding is another choice for advanced cases. Your MDA clinic will refer you to a speech-language pathologist (SLP) or an otolaryngologist (ear, nose, and throat doctor) pro re nata.
Limb weakness
The trouble with recollecting the feet when walking can result in stammering and falls. Leg braces, a cane, or a walker can help. Eventually, those with OPMD may have to use a wheelchair to create mobility more convenient. Upper arm and shoulder weakness that limits function will be addressed with adaptive techniques through physical therapy.
Ptosis
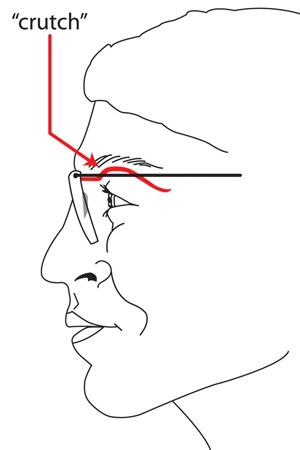
Droopy eyelids, or ptosis, can significantly impair vision and should cause social awkwardness. This problem will be resolved with a sort of surgery called a frontalis sling performed by an oculoplastic surgeon. For a “low-tech” solution, some people use connections to glasses that hold the eyes open. These are called eyelid crutches or ptosis crutches.
Ptosis Repair Surgery
Ptosis repair surgery will completely fix the condition. This surgery includes reattaching the eyelid muscles to lift the eyelid to a traditional position. Physicians may recommend supplemental ointments or injected fillers to reinforce and help tighten the eyelid skin and improve the results of surgery. Repair surgery may have side effects, like temporary numbness of the eyelid, scarring, dry eyes, and infection.
Eye drops
For temporary cases of eyelid droop caused by Botox injection, one older study trusted Source suggested that ticlopidine eyedrops may contribute to a faster recovery because they cause the eyelids to contract quickly, mimicking droopy eyelid exercises.
Blepharoplasty
An upper eyelid blepharoplasty may be a very trendy cosmetic surgery technique that tightens and raises the eyelids. It’s most frequently an aesthetic procedure and isn’t covered by insurance unless a medical condition has caused the ptosis.
Functional surgery
For medical cases of ptosis, a resection of the muscle is commonly used for mild cases. In moderate cases, a shortening of most eyelid muscles is also performed. An eyebrow lift is also recommended for more severe cases.
Physiotherapy Treatment
Currently no cure or no specific treatment to extinguish the symptoms or stop the disorder’s progression.
A consistent diet planned with the assistance of a dietitian together with exercises taught by a therapist can assist with mild symptoms of dysphagia.
The surgical intervention also can help temporarily manage symptoms associated with ptosis and dysphagia. Cutting one in all the throat muscles internally, an operation called cricopharyngeal myotomy may be a method to ease symptoms in further severe cases.
Many of those affected with proximal limb weakness will eventually require assistive devices like a wheelchair.
Power Wheelchair
Wheelchair
As with all surgical procedures, they are available with many risk factors. because the dysphagia becomes more severe, patients become malnourished, lose significant weight, become dehydrated, and suffer from repeated incidents of bronchial pneumonia. These last two are often the explanation for death.
Exercises
You can work eyelid muscles by raising your eyebrows, placing a finger underneath, and holding them up for several seconds at a time while trying to shut them. This creates resistance like weight lifting. rapid, forceful blinks and eye rolls also work eyelid muscles.
Exercise for Ptosis
To Help Drooping Eyelids

While face exercises have grown in popularity in recent years, only a few studies are conducted to gauge the effectiveness of eye or eyelid exercises in helping improve the looks of skin sagging or wrinkles. One recent supporting study did end in associates reporting real improvement in 18 of 20 facial areas and noting they were satisfied. Trials to this point are small, though, so there’s little medical evidence to make a copy of the thought that facial exercise might improve your eyelids.
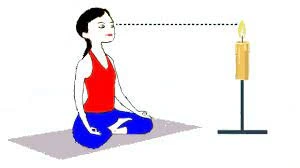
Trataka yogic eye exercise
Intended for overall eye health and vision improvement, the Trataka yogic eye exercise is well-known among the ayurvedic community. Because eye movement is linked to eyelid movement, this exercise can be beneficial. Trataka could be a sequence of practices in yoga that are beneficial for your eye health in a number of ways.
One such exercise is named Bahiranga, and involves the subsequent steps:
Sit in an exceedingly meditative upright posture either on the ground or on a firm chair. Keep your head straight and palms facing down. Keeping your eyes open, look straight ahead at one point. Without moving your head, slowly move your eyes towards the right shoulder and rest look for several seconds without blinking. Slowly move your gaze back to the middle position, and so repeat on the left side.
There are various adaptations to the present exercise. additionally, to the above movements, you’ll incorporate the subsequent gazes — all of which begin and end with looking at a set point and need you to stay your head still:
- Look up and down.
- Direct focus to the tip of the nose.
- Try to look upward and see between your eyebrows.
- Rotate your eyeballs slowly clockwise and counter-clockwise.
Wearing a watch Patch
If just one of your eyelids droops, you will tend to use the opposite eye for tougher tasks, similar to you’d use your good hand or leg rather than one that’s injured. to create sure that the weaker eyelid gets the maximum amount of natural exercise possible, you may want to cover your good eye with a patch. this suggests that you’ll perform some eyelid exercises during the day without even realizing it.
Wearing a watch patch might not appear to be an actual exercise, but it’s one of the simplest ways to strengthen drooping eyes, especially for kids who are diagnosed with congenital ptosis (droopy eyelid at birth). If a baby has severe unilateral (in one eye) ptosis, they’re in danger of developing further issues like lazy eye or strabismus (crossed eyes). In fact, strabismus occurs in 10.3% to 32% of youngsters with droopy eyelids.
Because therapists opt to wait until children are 3 to five years old before performing corrective surgery for ptosis, putting a closed patch over the healthier eye can strengthen the weaker eye and help prevent the onset of added conditions while your child awaits the suitable procedure.
Although medical professionals previously suggested wearing a watch patch for 6 hours on a daily basis or more, recent studies show that children only have to wear an eye-fixed patch for 2 hours daily for this exercise to figure.

Eyelid Ptosis Exercises
Eyelid ptosis exercises can help reduce drooping. Exercises within which you squint along with your lower eyelids can help to decrease the hollows and puffiness beneath your eyes. as an example, begin by sitting erect or lying supine. While putting index fingers at the outer corners of your eyes and then place your middle fingers on the inner corners of the eyes. As apply gentle pressure with these fingers, direct look to the ceiling and squint strongly with only the lower eyelids. Keep your upper eyelids wide open. Release the squint so repeat the exercise 10 times.
Lower and Stretch
To strengthen your upper eyelids, begin by looking directly at your face in a very mirror. Place your index fingers slightly below your eyebrows, keeping your fingers slightly curved. Hold eyebrows against the corrugation of bone above the eyes. Close your eyelids, stretching your upper lids down. Repeat this subtle movement five times so squeeze your eyes shut for a count of six. Relax the contracted position of your eyelids on a count of three then open your eyes. Perform the exercise twofold daily, five days per week.
Pencil Push-Up

This eye exercise is intended to strengthen your musculus and improve your lazy eye’s ability to converge properly. Start by taking a daily pencil and holding it up ahead of your face. Focus with both of your eyes on a tiny low piece of text or letter that’s printed on the side of the pencil. Then, start moving the pencil closer and closer to the cross of your nose. In line with the Mayo Clinic, the exercise must be performed five days per week for a quarter-hour every day. If you’re doing the exercise correctly, you’ll perform around 100 repetitions per day of the exercise.
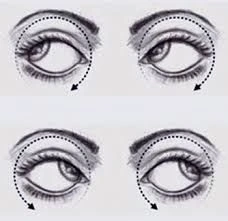
Eye Roll Exercise
This eye roll exercise is meant to strengthen your eye muscles still as help relax your eyes. Start by sitting down on a chair together with your back straight and your feet firmly touching the bottom. Both eyes close and, place fingertips on the tops of both eyelids. ensure that you are pressing on your eyelids with only three fingers per hand. From here, perform one full eye appear a clockwise direction. Roll your eyes in the incorrect way just once. Repeat this exercise back and forth until you’ve got performed the exercise 50 times. Perform three to 5 days every week, betting on your eye strength.

Computer Vision Therapy
Computer vision therapy exercises are designed to assist reduce the effect of esotropia on your vision. Sit before your computer together with your back straight and your eyes level with the pc screen. Using any basic vision program, like Home Vision Therapy, perform computer-based eye exercises for an hour or more each day 2. Many of those computer exercises directly target troubles with convergence and work on strengthening your eye muscles to assist eliminate these problems 2. Exercises involve small dots on your screen converging in the middle of the screen. Both of your eyes must follow the separate dots until they converge within the middle of the screen.
For Droopy Eyebrow
You can perform an exercise that strengthens both the muscles within the forehead and eyelids and requires the coordination of movements between your eyebrows and eyelids. Starting by lifting your eyebrows so close your eyes. While your eyebrows are lifted, close your eyes. Lower your eyebrows to complete one rep. Perform one set of 10 reps. after you close your eyelids, avoid squeezing or contorting your face. concentrate on raising the outer part of each eyebrow.
Raises Your Eyebrows
In the same way that a smile lifts the muscles around your lips, you’ll be able to gently lift your eyelids. Start by placing your fingertips at the outer corners of the eyes. Slowly and gently press your lower eyelids upward. The skin on the edges of and beneath your eyes is going to be raised up toward your nose. Hold this position for a minimum of 6 seconds and then release and back to the starting position.
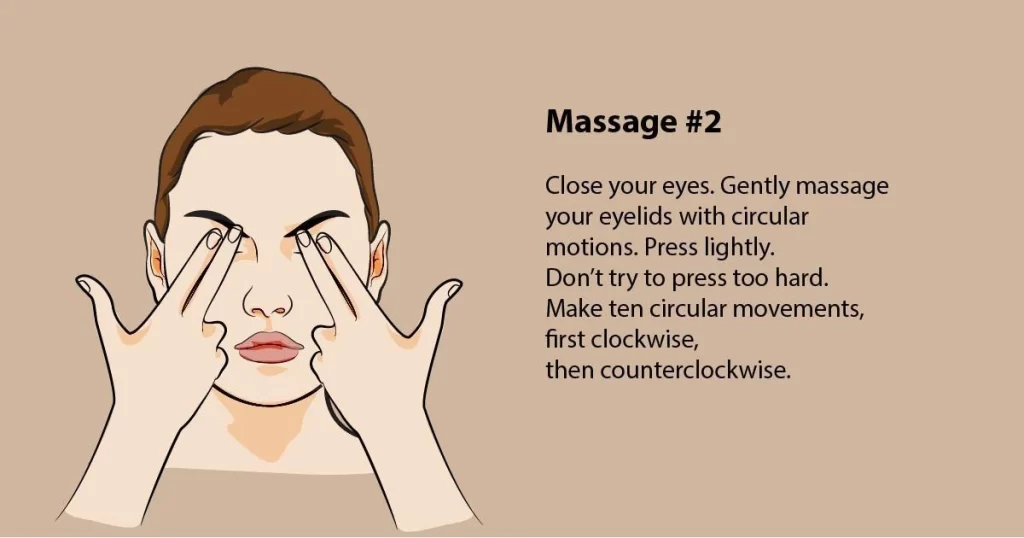
Eye Massage
Stimulate the attention muscles with a watch massage. Place your ring fingers on the environs of the attention socket bone, and pressing very lightly, work your way around the socket using small circular movements. Repeat for one minute.
Blinking
Once we sleep deeply, we do not blink, and this could cause a build of fluid around the eyes. If you discover your eyes are puffy upon wakening, blink rapidly for 30 seconds, and also the fluids should begin to dissipate. an additional pillow may also help prevent the build from eye fluids overnight
Temple Massage

Use your index finger to massage the temples. The temple area is found at the side of your head in line with the attention socket and is slightly indented. Massage the temples for one minute at a time to assist reduce puffy eyes.
Accupressure Hand Massage
Open your hand with the palm facing you, and locate the purpose between your index and finger. Using the opposite hand, massage the ridge of skin between the 2 fingers, and also massage the within of the primary digit of the 2 fingers. Continue massaging for a minimum of one minute before switching hands. Hand reflexology works on the premise of zone therapy, which purports that every of the body’s organs incorporates a corresponding external reflex point. this can be a useful exercise that will be performed unnoticed whenever your eyes feel strained or tired.
Exercises For Dysphagia

Shaker Exercise
Purpose: To improve your ability to swallow and strengthen muscles
How to Perform: First, lie flat on your back and lift your head slightly off the bottom. Have your head raised high enough so your eyes are fixated on your toes? Hold this position for some seconds and so place your head back off. Repeat this same movement some more times. For best results, try this exercise three to 6 times throughout the day. Over time, you’ll be able to increase the duration of the top lift and also the number of repetitions.
Hyoid Lift Maneuver
Purpose: Builds swallowing muscle strength and control
How to Perform: Place multiple small pieces of paper on a towel before you. Next, place a straw in your mouth and suck on the straw, allowing the paper to induce picked up by the tip of the straw. Keep sucking on the straw as you bring the straw over to a cup, and stop sucking to release the paper into the cup. you ought to aim to successfully place all of the pieces of paper into the cup. you’ll start out with just 3 to five pieces of paper and slowly increase to around 10.
Effortful Swallow
Purpose: Improve the contact and coordination between the various muscles used while swallowing
How to Perform: While dry swallowing, squeeze all of the muscles related to swallowing as hard as possible. Repeat this up to 10 times in an exceedingly single session. you must do 3 sessions of this exercise per day to sufficiently strengthen your muscles.
Supraglottic Swallow
Purpose: Improves your ability to swallow food
How to Perform: Take a deep breath and keep holding your breath as you place a little bite of food in your mouth and swallow. Then, cough to clear any remnants of saliva or food which can have gone down past your vocal cords. Lastly, exhale. During your first few attempts at the exercise, don’t use food. Once you’ve got sufficient practice with this exercise, you’ll be able to try it with a little piece of food in your mouth.
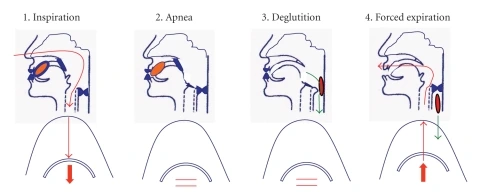
Super Supraglottic Swallow Maneuver
Purpose: Improve ability to swallow food and strengthens swallowing muscles
How to Perform: This exercise is largely identical because the previous one but may be a little more intense. This time, you ought to bear down while taking a deep breath and so swallow hard.
Please undertake these swallowing exercises only at the advice and instruction of your treating therapist.
Safety Considerations
If you are feeling pain while doing any of those exercises, you ought to either reduce the number of repetitions you complete or try something else.
And you’ll want to make certain you’re using proper techniques since repeated muscle use within the face can actually cause wrinkles to become more defined if you’re not being careful. Additionally, if you’ve had facelifts, including injections or dermal fillers, facial exercises may not be right for you, since they will cause the fillers not to last as long.
Finally, you must note that some symptoms associated with ptosis are also signs of a more serious condition affecting the muscles, nerves, brain, or cavity.
you must get in contact along with your doctor if you experience any of the following:
- Affected vision
- Double vision
- Eye pain or redness
- Difficulty moving your eye
- Weakness of facial muscles, arms, or legs, paired with difficulty in speaking or swallowing and a headache
- Sudden drooping of 1 eye
- Even if you don’t think your drooping eyelids are cause for a real medical concern, it’s always an honest idea to test along with your doctor and see what else they may suggest assisting take care you’re protecting your vision and your skin because it ages.
Complications of Oculopharyngeal hereditary condition
In severe OPMD, upper leg weakness may need to use a wheelchair. This is often rare, though.
The main complications of OPMD need to do with swallowing problems (dysphagia). this could cause weight loss and nutrition problems. It can even cause choking and therefore the breathing of food, saliva, liquids, or stomach contents into the lungs (aspiration). This will outcome in infections and cause pneumonia, which may be fatal. you’ll need a procedure to cut back the danger of aspiration. the general public with OPMD has normal lifespans.
FAQ
Is an Oculopharyngeal hereditary condition a neurological disorder?
Oculopharyngeal congenital disease (OPMD) may be a rare genetic muscle disorder with onset during adulthood most frequently between 40 and 60 years old. OPMD is defined as a slowly progressive muscle disorder (myopathy) affecting the muscles of the upper eyelids and the throat.
How common is Oculopharyngeal muscular dystrophy?
OPMD affects men and ladies equally, and this genetic disorder is often inherited from either one parent (autosomal dominant, the foremost common form) or both parents (autosomal recessive form). The frequency of the autosomal dominant form is estimated to be 1 in 100,000 in Western countries.
Can Oculopharyngeal genetic abnormality cause death?
Disease progression varies from one individual to a different. Complications include choking, regurgitation, aspiration, and pneumonia. Consecutive bronchial pneumonia, along with malnutrition or maybe starvation, is the leading cause of death in patients with OPMD.
What causes eye muscles to weaken?
Myasthenia gravis causes muscle weakness that usually has times when it improves and other times when it gets worst. It frequently affects the eyes and faces at first, but usually spreads to other parts of the body over time.
Is able to restore eye muscles?
Eye Circles: While sitting or standing, move your eyes in an exceedingly clockwise direction 20 times, making the circle as wide as you’ll be able to. Relax for 10 seconds, then repeat the other way. Doing this 3 times daily will help to stretch your eye muscles.
Can surgery fix weak eye muscles?
Eye muscle repair is surgery to correct musculus problems that cause strabismus (crossed eyes). Strabismus surgery corrects and aligns the muscles of the attention. The conjunctiva links the attention ball to the eye socket. The external muscles of the attention are found behind the conjunctiva.
How does one exercise with muscular dystrophy?
Strength Exercises
Because the muscles of somebody with MD are already weak, it’s recommended that they follow a lightweight, high-repetition regimen instead of trying to lift heavy weights. Maintain the weights wherever between 5 and 10 pounds to start out and once you feel comfortable gradually increase the weights.