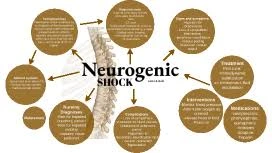
Neurogenic shock
Table of Contents
What is neurogenic shock?
Neurogenic shock is a distributive type of shock resulting in hypotension which means low blood pressure, usually with bradycardia [ slowed heart rate ], generated by disturbance of autonomic nervous system pathways. It can happen after damage to the central nervous system, like spinal cord damage & traumatic brain damage.
The restricted heart rate results from a vagal reaction unopposed by a sympathetic nervous system (SNS) response. Some cardiovascular fluctuation is exacerbated by hypoxia or therapy with endotracheal or endobronchial suction utilized to prevent pulmonary aspiration.
This shock is a potentially devastating difficulty, conducting to organ dysfunction & death if not promptly recognized & treated.
Pathophysiology
This type of shock is diagnosed established on a person’s symptoms & blood pressure levels.
Neurogenic shock’s production contains:
- warm & pink skin
- struggled to breathe
- low blood pressure
- dizziness
- anxiety
- history of trauma to the upper spine and head
if the damage is to the head or neck, hoarseness or problem swallowing may happen.
Signs of neurogenic shock are determined from other structures of shock by the lack of symptoms of the compensatory mechanisms activated by the SNS, generally in another type of shock. ‘This SNS response is generated via the release of epinephrine & norepinephrine, & signs of these neurotransmitters’ activity are typically absent where the shock is of neurogenic origin.
Those signs and symptoms in non-neurogenic shock would contain tachycardia increased heart rate [tachycardia], increased breath rate [tachypnea], sweating, & adaptive vasoconstriction, which helps in another type of shock to shunt blood out from the extremities & to the important organs In this shock, the body loses its capability to trigger the SNS so that only the parasympathetic technique stays. The resulting loss of sympathetic tone plays an important role in another type of shock.
Causes of Neurogenic Shock
This shock most typically occurs following spinal cord damages that disrupt the innervation of the collection of energy to the sympathetic nervous system. The sympathetic nervous system is accountable for activating the body’s “fight or flight” response. When activated, the body is on high alert, the blood vessels tighten which means constriction, & blood pressure & heart rate increase. The sympathetic nervous system is countered by the parasympathetic nervous system, which is accountable for the “rest and digest” functions. When triggered, the blood vessels dilate [expand], blood pressure & heart rate decrease, & digestion is stimulated. Both systems are important for proper functioning.
Normally, the parasympathetic & sympathetic nervous systems alternate dominance throughout the day, relying on the situation, to support the body’s requirements. During neurogenic shock following spinal cord damage, the loss of empathetic innervation results in unopposed parasympathetic stimulation. In other terms, the body’s relaxation reaction takes over without restriction.
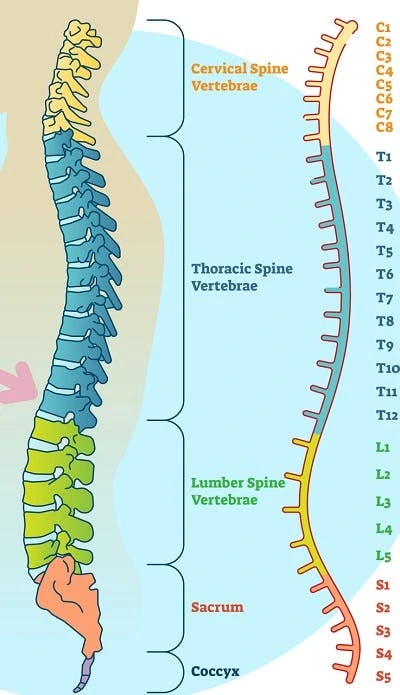
Because sympathetic innervation of the heart is associated with the T1 to T5 levels of the spinal cord, neurogenic shock is most common in people with T6 or higher level spinal cord damage. People with cervical spinal cord damage are more likely to experience neurogenic shock than those with thoracic SCIs. Additionally, the higher & more complete the SCI, the more painful the shock. Although much more irregular, it is also possible for people with spinal cord damage below the T6 level to experience neurogenic shock. Sympathetic innervation of the blood vessels persists to the L2 level of the spinal cord.
While neurogenic shock is considerably typically associated with spinal cord injuries, it can also be induced by:
- Spinal anesthesia
- Guillain Barre syndrome
- Autonomic nervous system toxins
- Transverse myelitis
- Trisomy 21
- Skeletal dysplasia
- Tonsillopharyngitis
- Other neuropathies
Signs and Symptoms of Neurogenic Shock
Neurogenic shock normally lasts between 1 to 6 weeks after a spinal cord injury ensues. While it mostly involves the cardiovascular system, neurogenic shock can cause permanent tissue injury if left untreated. Therefore, it’s important to be aware of its symptoms & seek immediate medical attention. Loss of sympathetic innervation induces the blood vessels to dilate, which causes limited pressure moving blood throughout the body. As a result, cells are not adequately fueled with the oxygen & nutrients required for optimal body functioning.
Loss of sympathetic innervation may also induce blood to pool in the veins of the limbs. Rather than going back to the heart, blood may accumulate in the arms & legs. This creates a dangerous cycle where less & less blood circulates throughout the body.
Common symptoms of neurogenic shock contain:
Hypotension: Low blood pressure means lower than 90 mm Hg systolic or 60 mm Hg diastolic.
Bradycardia: Lower than normal heart rate [ below 60 beats a minute ].
Dry, warm skin: Instead of cool, moist skin, the patient undergoes dry, warm skin due to vasodilation & the inability to vasoconstrictor.
Diaphragmatic breathing: If the damage is below the 5th cervical vertebra, will exhibit diaphragmatic breathing due to failure of nervous management of the intercostal muscles which are required for thoracic breathing.
Respiratory arrest: If the damage is above the 3rd cervical vertebra, the patient will go into respiratory arrest, due to loss of nervous control of the diaphragm.
These symptoms can present themselves in a combination of ways, including:
- Fatigue
- Dizziness or lightheadedness
- Weakness
- Confusion
- Blurred vision
- Nausea
- Fainting
- Shortness of breath
- Poor concentration
Diagnosis of neurogenic shock
Diagnosis of neurogenic shock is achievable via the following tests:
Computerized tomography (CT) scan: A CT scan may supply a better look at anomalies seen on an X-ray.
Xrays: Medical personnel generally order these tests on people who are imagined of having spinal cord damage after trauma.
Magnetic resonance imaging (MRI): Magnetic resonance imaging uses a strong magnetic area & radio waves to produce computer-generated images.
Differential Diagnosis
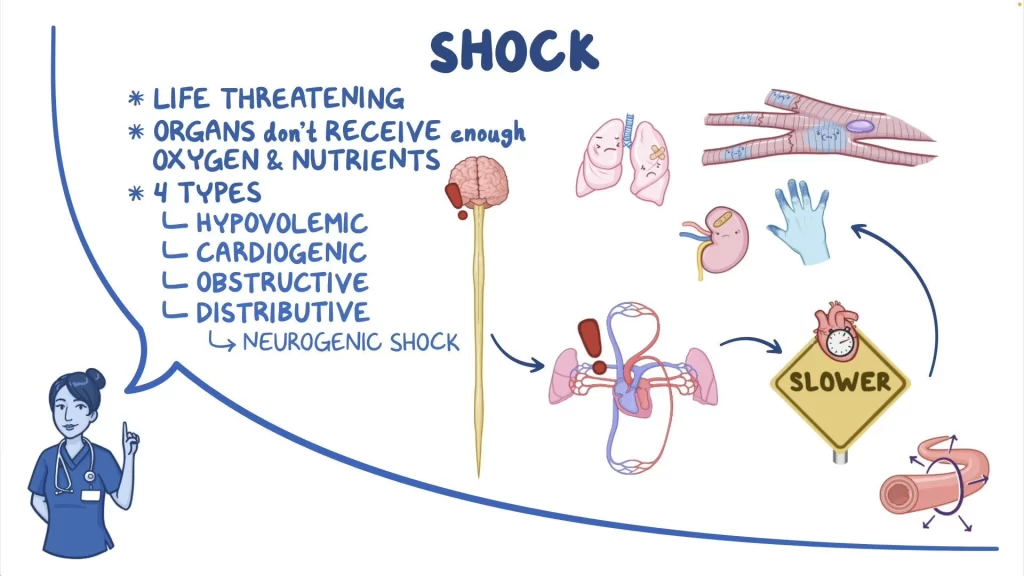
- Hypovolemic shock
- Obstructive shock
- Cardiogenic shock
- Septic shock
Shocks are associated with tachycardia. The term “spinal shock” means the acute loss of motor, sensory, and reflex parts below the level of damage & can be associated with neurogenic shock.
Treatment
When blood pressure & heart rate fall too low, the body does not have adequate blood supply to function appropriately. As a result, poorly controlled neurogenic shock can cause important cardiovascular & neurological damage. Therefore, treatment for neurogenic shock concentrates on restoring heart rate & blood pressure to normal levels.
Medical Management
Treatment of neurogenic shock includes:
Restoring sympathetic tone: It would be either via the stabilization of a spinal cord injury or, in the example of spinal anesthesia, by placing the patient properly.
Immobilization: If the patient has a supposed case of spinal cord damage, traction may be required to stabilize the spine to bring it to the correct alignment.
IV Fluids: IV fluids are the primary therapy for low blood pressure. They fill fluid levels in the veins to assist stabilize blood pressure.
Vasopressors: If IV fluids demonstrate ineffective, vasopressors can assist tighten blood vessels & increase blood pressure. Commonly used vasopressors contain norepinephrine, dopamine, & epinephrine.
Atropine: If the heart rate is low, the doctor may specify atropine. It supports normalize heart rate by interfering with parasympathetic action.
Inotropic agents: Inotropic mechanisms such as dopamine may be invested in fluid resuscitation.
Steroids: Patients with clear neurological deficits can be given I.V. steroids, such as methylprednisolone in high doses, within 8 hours of the commencement of neurogenic shock.
Heparin: Administration of heparin or low molecular weight heparin as defined may contain thrombus formation.
It’s also suggested by the American Association of Neurological Surgeons and the Congress of Neurological Surgeons’ Guidelines that mean arterial blood pressure (MAP) is maintained at 85 to 90 mmHg for the first 7 days following acute Spinal cord injury.
Nursing Treatment
Nursing treatment of a patient with neurogenic shock contains:
Nursing Assessment
Examination of a patient with neurogenic shock should contain:
ABC assessment: The prehospital provider should follow the basic airway, breathing, & circulation system of the trauma patient while protecting the spine from any extra exercise.
Neurologic assessment: Neurologic deficiencies & a general level at which anomalies began should be recognized.
Nursing Diagnosis
Established on the investigation data, the nursing diagnoses for a patient with neurogenic shock are:
Risk for inadequate breathing pattern: This is related to the impairment of innervation of the diaphragm lesions at or above C-5.
Risk for trauma: This is related to temporary weakness or instability of the spinal column.
Insufficient physical movement: This is related to neuromuscular impairment.
Disturbed sensory perception: This is related to the destruction of sensory tracts with altered sensory reception, transmission, & integration.
Acute pain: This is related to the pooling of the blood secondary to thrombus formation.
Nursing Care Planning & Goals
The main goals for the patient contain:
- Maintain satisfactory ventilation as evidenced by the absence of respiratory distress & ABGs within acceptable limits.
- Demonstrate proper behaviors to support the respiratory effort.
- Maintain accurate alignment of the spine without further spinal cord damage.
- Hold a position of function as evidenced by the lack of contractures, & foot drop.
- Increase the strength of unaffected or compensatory body parts.
- Demonstrate techniques or behaviors that allow the resumption of activity.
- Identify sensory impairments.
- Identify behaviors to compensate for deficiencies.
- Verbalize understanding of sensory needs & potential for deprivation or overload.
Nursing Interventions
Nursing interventions are required towards supporting cardiovascular & neurologic function until the generally temporary outbreak of neurogenic shock resolutions.
Elevate the head of the bed: Elevation of the head helps control the spread of the anesthetic agent up the spinal cord when a patient accepts spinal or epidural anesthesia.
Lower extremity interventions: Applying anti-embolism stockings & elevating the foot of the bed may help underestimate the pooling of the blood in the legs & prevent thrombus formation.
Exercise: Passive range of motion [ROM] of the immobile extremities helps stimulate circulation.
Airway patency: Maintain patent airway keep head in a neutral position, advance the head of the bed slightly if tolerated, & use airway adjuncts as indicated.
Oxygen: Administer oxygen by an appropriate approach [nasal prongs, mask, intubation, ventilator].
Activities: Plan movements to provide uninterrupted rest times & encourage involvement within personal tolerance & ability.
BP monitoring: Measure & monitor BP before & after movement in acute phases or until stable.
Reduce anxiety: Assist patient to identify & compensate for alterations in sensation.
Neurogenic Shock vs Spinal Shock
Neurogenic shock & spinal shock are 2 separate situations that are frequently confounded with one another because they can both happen after spinal cord damage. Additionally, they can also share signs involving hypotension & bradycardia
The neurogenic shock predominantly occurs in the T6 group of damage or higher, spinal shock can appear following damage to any part of the spinal cord.
Without sympathetic tone, blood cannot efficiently circulate throughout the body, which results in a reduced heart rate, low blood pressure, & temperature dysregulation.
In contrast, spinal shock results in the temporary loss of all motor, sensory, & reflex functions below one’s level of damage. It’s caused by inflammation & swelling of the spinal cord, which determines blood flow below the level of damage. Once the spinal cord is stabilized & swelling dies down, people may gradually recover some reflexes, sensations, & motor control. This will primarily rely on the severity of the spinal cord damage.
Evaluation
Expected patient results are:
- Maintained satisfactory ventilation.
- Demonstrated proper behaviors to support the respiratory effort.
- Maintained correct alignment of the spine without further spinal cord damage.
- Maintained position of function.
- Increased strength of unaffected or compensatory body regions.
- Demonstrated techniques or behaviors that enable resumption of movement.
- Determined sensory impairments.
- Identified behaviors to compensate for deficiencies.
- Verbalized understanding of sensory requirements & potential for deprivation or overload.
Documentation Guidelines
The focus of documentation is:
- Relevant history of the situation
- Respiratory, breath sounds, and use of accessory muscles
- Laboratory values
- Past and recent history of damages, awareness of safety requirements
- Use of safety equipment or methods
- Environmental concerns, safety problems
- Level of function, ability to participate in specific or selected activities
- Client’s description of the response to pain, specifics of pain inventory, expectations of pain management, & acceptable level of pain
- Primary medication use
- Plan of care, specific interventions, & who is involved in the planning
- Education plan
- Response to interventions, teaching, actions performed, & treatment regime
- Attainment or progress toward expected outcomes
- Changes to the plan of care
Prognosis
What can predict if have neurogenic shock?
It’s possible to have hypotension and low blood pressure for 5 weeks after the damage.
How long does neurogenic shock last: Neurogenic shock symptoms can last 4 to 5 weeks.]
When can go back to work or school?
Producing to work or school will rely on the extent of the spinal cord damage & other damages from the accident. May require you to make major changes in your life to adjust the restricted mobility.
Outlook for neurogenic shock
Without treatment, shock is usually fatal. With treatment, the outlook depends on:
- Age
- The severity of the injury
- Injuries to the organs
- Other medical difficulties
- How long have to wait for treatment
- Other difficulties like being unable to speak or balance
How well the body responds to treatment
Having spinal cord damage makes them 2 to 5 times as likely to die early compared to those who don’t have that damage. The threat of death is highest in the 1st year after spinal cord damage.
How do I take care of myself?
Because of the spinal cord damage, you’ll be more possible to have other issues like deep vein thrombosis. Also, one or more of your organs may be damaged because of the absence of blood flow during neurogenic shock.
When should I see my healthcare provider?
Should contact the provider if anything varies with the condition: vital signs, pain level, etc.
When should I go to the ER?
Should get quick help if have:
- Chest pain
- Dizziness
- Nausea
FAQ
Neurogenic shock guides the hemodynamic triad of hypotension, bradycardia, & peripheral vasodilation resulting from extreme autonomic dysfunction & the interruption of sympathetic nervous system control in acute spinal cord damage. Hypothermia is characteristic.
If the sympathetic nervous system doesn’t function well, the blood pressure could drop & can affect the brain, tissues, & spinal cord. Other causes of neurogenic shock include car accidents that induce central nervous system damage and spinal cord injury. Sports damage causes trauma to the spine.
Lay the person down & elevate the legs & feet slightly, unless they think this may cause pain or further damage. Keep the person still & don’t move the person unless required. Form CPR if the person offers no signs of life, such as not breathing, coughing, or moving.
Neurogenic shock represents the hemodynamic changes resulting from a premature loss of autonomic tone due to spinal cord damage. It is commonly seen when the level of damage is above T6. Spinal shock, on the other hand, directs to the loss of all triumphs below the level of harm & is not circulatory.
In extreme cases, the person may need a blood transfusion. Internal or external wounds may require surgery. Cardiogenic shock boosts blood volume with intravenous fluids. Remedies to constrict the blood vessels will improve the heart’s ability to pump.
Neurogenic shock is a segment of spinal shock syndrome & guides to the hemodynamic instability seen in these patients with hypotension, bradycardia, & hypothermia secondary to sympathetic-parasympathetic dysfunction or inequality.