Monogenic Diabetes
Table of Contents
What Is Monogenic Diabetes?
- Monogenic diabetes is an infrequent type of diabetes caused by a change or mutation to a single gene. It differs from type 1 or type 2 diabetes, and sometimes requires genetic testing for an accurate diagnosis.
- In monogenic diabetes, insulin production is decreased. This causes glucose (blood sugar) levels to increase. Yet not all cases of monogenic diabetes require insulin treatment.
There are 2 main forms of monogenic diabetes:
- neonatal diabetes mellitus (NDM) happens in newborns and infants
- maturity-onset diabetes of the young (MODY) is more usual than NDM and occurs in adolescents and young adults.
Key statistics
- Per the CDC’s 2020 report Trusted Source, 10.5 percent of all Americans have diabetes, with the vast majority having type 2.
- Monogenic diabetes accounts for approximately 1 to 4 percent of trusted Sources of all diabetes cases in the United States.
- A 2016 study reportsTrusted Source NDM is estimated to happen in anywhere from 1 in 20,000 to 1 in 500,000 infants.
How it is different from type 1 and type 2?
- While monogenic diabetes is a form of diabetes, it does various types 1 and 2, which are polygenic. Monogenic diabetes stems from a mutation or exchange in a single gene. Polygenic types outcome from mutations in multiple genes.
- All cases of type 1 diabetes need insulin treatment, while type 2 diabetes & monogenic diabetes do not always require insulin. Insulin treatment is more likely to be required as people with monogenic diabetes get older.
What are the Causes of Monogenic Diabetes?
- Monogenic diabetes is due to changes or mutations in a single gene. Monogenic types of diabetes are sometimes inherited from just one parent, called an “autosomal dominant” gene. Sometimes the mutation or change occurs spontaneously, which means it’s not inherited.
- While certain types of monogenic diabetes may be temporary, it can sometimes also be a lifelong condition.
Symptoms of Monogenic Diabetes
- Symptoms of monogenic diabetes can differ, depending on which kind it is. Knowing how to recognize possible symptoms of MODY or NDMTrusted Source, especially in a young child, can assist you to get timely, appropriate treatment.
| Symptoms | Neonatal diabetes mellitus (NDM) | Maturity-onset diabetes of the young (MODY) |
| frequent urination | ✓ | ✓ |
| rapid breathing | ✓ | |
| dehydration | ✓ | ✓ |
| thirst | ✓ | |
| blurry vision | ✓ | |
| recurrent skin infections | ✓ | |
| recurrent yeast infections | ✓ |
How to Diagnose the Monogenic Diabetes?
- Blood sugar tests and genetic testing are utilized to diagnose monogenic diabetes such as MODY and NDM. Genetic testing can be done by blood or saliva samples. The DNA is examined for exchanges in the genes that cause monogenic diabetes.
The National Institutes of HealthTrusted Source explains that genetic testing for monogenic diabetes is recommended if:
- diabetes is diagnosed previous 6 months of age,
- diabetes is diagnosed in children or young adults, especially those with a family history of diabetes, or those who do not have typical features of type 1 or 2,
- there is stable & mild fasting hyperglycemia, especially without obesity,
- There are at least 14 different genesTrusted Sources associated with Maturity-onset diabetes of the young (MODY), and more are still being discovered and researched. The type of gene detected can indicate Maturity-onset diabetes of the young (MODY’s) severity or mildness.
The tests are most usually used to detect the following genes:
- HNF1A gene (MODY 3),
- glucokinase gene or GCK (MODY 2),
- HNF4A gene (MODY 1),
- HNF1B gene (MODY 5).
For those with Maturity-onset diabetes of the young (MODY), other clinical tests can be used in addition to genetic testing. Per a 2020 overviewTrusted Source of clinical screening approaches for Maturity-onset diabetes of the young (MODY), these may include:
- testing antibodies for type 1 diabetes such as anti-GAD antibodies, or zinc transporter antibodies (which are low in people with Maturity-onset diabetes of the young (MODY))
- checking the C-peptide level (which indicates whether the body creates insulin)
- If a newborn or a baby starts having symptoms of diabetes, it is often recommended to test for monogenic diabetes. It is infrequent for type 1 diabetes to occur in infants, and type 2 diabetes can affect older kids, not babies. Neonatal diabetes mellitus (NDM) could be missed or misdiagnosed without genetic testing.
Treatment of Monogenic Diabetes
- The treatment turns on the genetic mutation causing monogenic diabetes, & the severity of the condition or type.
- Certain forms of monogenic diabetes can be managed with diet & exercise, while others need insulin. Treatment with an oral medication known as a sulfonylurea agent may also be necessary. Sulfonylurea is an oral medicine that assists the body release more insulin into the blood.
Treatments for diabetes hang upon your type of diabetes, how well-managed your blood glucose level is, and your other existing health condition.
- Type 1 diabetes: If you have this type, you should lay insulin every day. Your pancreas no longer creates insulin.
- Type 2 diabetes: If you have this type, your treatments can include the medications (both for diabetes and for conditions that are risk factors for diabetes), insulin, and lifestyle changes such as losing weight, making healthy food choices, and being one and more physically active.
- Prediabetes: If you have prediabetes, the goal is to maintain you from progressing to diabetes. Treatments are focused on treatable risk factors, such as losing weight by eating a healthy diet (such as the Mediterranean diet) and exercising (at least five days a week for 30 minutes). Many of the strategies used to cure diabetes are similar to those recommended to treat diabetes (see the prevention section of this article).
- Gestational diabetes: If you have this type and your glucose level is not very great, your initial treatment might be modifying your diet and getting regular exercise. If the target goal is still not met or your glucose level is very high, your healthcare (doctor) team may start medication or insulin.
Oral medications & insulin tasks in 1 of these ways to treat your diabetes:
- Stimulates your pancreas to create & release one or more insulin.
- Stabilize down the release of glucose from your liver (extra glucose is stored in your liver).
- Blocks the breakdown of the carbohydrates in your stomach or intestines so that your tissues are very sensitive to (better react to) insulin.
- Assists rid your body of glucose through improved urination.
What oral medications are approved to treat diabetes?
- Above 40 medications have been approved by the Food & Drug Administration for the treatment of diabetes. It is beyond the extent of this article to review all of these drugs. Instead, we will shortly review the main drug classes available, how they work, and present the names of certain drugs in each class. Your healthcare (doctor) team will determine if the medication is right for you. If so, they will decide which specific drug(s) are good to treat your diabetes.
Diabetes medication drug classes involve:
- Sulfonylureas: These drugs decrease blood glucose by causing the pancreas to release one or more insulin. Ex. include glimepiride (Amaryl), glipizide (Glucotrol), and glyburide (Micronase, DiaBeta).
- Glinides (also called meglitinides): These drugs decrease blood glucose by getting the pancreas to release more insulin. Ex. include repaglinide (Prandin) and nateglinide (Starlix).
- Biguanides: These drugs lower how much glucose the liver produces. It also increases how insulin works in the body and steady down the conversion of carbohydrates into sugar. Metformin (Glucophage) is an example.
- Alpha-glucosidase inhibitors: These drugs reduce blood glucose by delaying the breakdown of carbohydrates and decreasing glucose absorption in the small intestine. An example is acarbose (Precose).
- Thiazolidinediones: These drugs increase the way insulin works in the body by allowing more glucose to enter into muscles, fat, and the liver. Ex. include pioglitazone (Actos) and rosiglitazone (Avandia).
- GLP-1 analogs (also known as incretin mimetics or glucagon-like peptide-1 receptor agonists): These drugs improve the release of insulin, reduce glucose release from the liver during later meals and delay food emptying from the stomach. Ex. include exenatide (Byetta), liraglutide (Victoza), albiglutide (Tanzeum), semaglutide (Rybelsus) and dulaglutide (Trulicity).
- DPP-4 inhibitors (also known as dipeptidyl peptidase-4 inhibitors): These drugs assist your pancreas release more insulin after meals. They also decrease the amount of glucose released by the liver. Ex. include alogliptin (Nesina), sitagliptin (Januvia), saxagliptin (Onglyza), & linagliptin (Tradjenta).
- SGLT2 inhibitors (also known as sodium-glucose cotransporter 2 inhibitors): These drugs work on your kidneys to separate glucose in your body through your urine. Ex. include with canagliflozin (Invokana), dapagliflozin (Farxiga), & empagliflozin (Jardiance).
- Bile acid sequestrants: These drugs reduce cholesterol and blood sugar levels. Examples include colestipol (Colestid), cholestyramine (Questran), and colesevelam (Welchol).
- Dopamine agonist: This medication reduces the amount of glucose released by the liver. An example is bromocriptine (Cyclocet).
- Many oral diabetes medications may be utilized in combination or with insulin to achieve good blood glucose management. Certain of the above medications are available as a combination of 2 medicines in a single pill. Others are accessible as injectable medications, for ex., the GLP-1 agonist semaglutide (Ozempic) and lixisenatide (Adlyxin).
Always take out your medicine similarly as your healthcare (doctor) prescribes it. Discuss your personal questions and concerns with all of them.
What insulin medications are approved to treat diabetes?
There are types of insulin for diabetes. If you require insulin, your healthcare team (doctor) will discuss the various types and if they are to be combined with oral medications. To follow is a short review of insulin types.
- Rapid-acting insulins: These insulins are taken out 15 minutes previous meals, they peak (when it best lowers blood glucose) at one hour and work for another two to four hours. Ex. include the insulin glulisine (Apidra), insulin lispro (Humalog), and insulin aspart (NovoLog).
- Short-acting insulins: These insulins take about 30 minutes to reach your bloodstream, reach their peak effects in 2 to 3 hours and last for three (3) to six hours. An ex. is insulin regular (Humulin R).
- Intermediate-acting insulins: These insulins reach your bloodstream in 2 to 4 hours, peak in 4 to 12 hours, and work for up to 18 hours. An example is NPH.
- Long-acting insulins: These insulins effort to retain your blood sugar stable all day. Commonly, these insulins last for about 18 (eighteen) hours. Examples include insulin glargine (Basaglar, Lantus, Toujeo), insulin detemir (Levemir), & insulin degludec (Tresiba).
- There are insulins that are a fusion of various insulins. There are insulins that are combined with a GLP-1 receptor agonist medication (e.g. Xultophy, Soliqua).
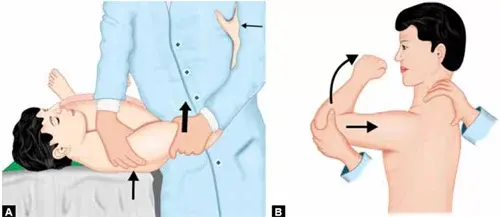
How is insulin taken? How many various ways are there to take out insulin?
Insulin is available in several diverse formats. You and your healthcare provider (doctor) will conclude which delivery method is right for you based on your preference, lifestyle, insulin requirements, and insurance plan. Here is a fast review of available types.
- Needle and syringe: With this method, you will insert a needle into a vial of insulin, pull back the syringe, and fill the needle with the genuine dose of insulin. You will inject the insulin into your belly or thigh, buttocks, or upper arm – rotating the injection spots. You may require to give yourself one or more shots a day to continue your target blood glucose level.
- Insulin pen: This device seems such as a pen with a cap. They happen prefilled with insulin or with insulin cartridges that are inserted and replaced for later use.
- Insulin pump: Insulin pumps are small, computerized devices, about the size of a small cell phone that you put on your belt, in your pocket, or under your clothes. They deliver rapid-acting insulin 24 hours a day through a little flexible tube known as a cannula. The cannula is inserted lower the skin using a needle. The needle is then removed leaving only the flexible tube to lower the skin. You replace the cannula every 2 (two) to 3 (three) days. Another type of insulin pump is attached straightly to your skin and does not utilize tubes.
- Artificial pancreas (also called a closed-loop insulin delivery system): This system utilizes an insulin pump linked to a continuous glucose monitor. The monitor checks your blood glucose levels every 5 (five) minutes and then the pump delivers the needed dose of insulin.
- Insulin inhaler: Inhalers allow you to breathe in a powdered inhaler through an inhaler device that you insert into your mouth. The insulin is inhaled into your lungs, then linked up into your bloodstream. Inhalers are approved for utilization by adults with Type 1 or Type 2 diabetes.
- Insulin injection port: This delivery method includes the placement of a little tube into the tissue beneath your skin. The port is clasped in place with an adhesive patch. You utilize a needle and syringe and insulin pen and inject the insulin through this port. The port is changed every certain day. The port supplies a single site for injection rather than having to rotate injection sites.
- Jet injector: This is a needleless delivery method that utilizes high pressure to make a fine spray of insulin through your skin.
Are there other treatment options for diabetes?
- Yes. There are 2 types of transplantations that might be an option for a select number of patients who have Type 1 diabetes. A pancreas transplant is possible. However, getting an organ transplant requires taking out immune-suppressing drugs for the release of your life and dealing with the side effects of these drugs. However, if the transplant is successful, you will possibly be able to stop taking insulin.
- The type of transplant is a pancreatic retreat transplant. In this transplant, clusters of islet cells (the cells that create insulin) are transplanted from an organ donor into your pancreas to back those that have been destroyed.
- Another treatment down research for Type 1 diabetes is immunotherapy. Since Type 1 is an immune system disease, immunotherapy holds promise as a way to utilize medication to turn off the areas of the immune system that cause Type 1 disease.
- Bariatric surgery is another treatment opportunity that is an indirect treatment for diabetes. Bariatric surgery is an option if you have Type 2 diabetes, have obesity (body mass index over 35), and are contemplated the best candidate for this type of surgery. Much increased blood glucose levels are glanced at in people who have lost a significant amount of weight.
- Of course, other medications are advised to treat any existing health problems that contribute to improving your risk of developing diabetes. such as high blood pressure, high cholesterol, and other heart-related diseases.
Physiotherapy Management
- Therapeutic exercise programs contain the major side of management. Patient education for perfect foot care is an essential area of the physical therapy program for diabetic patients.
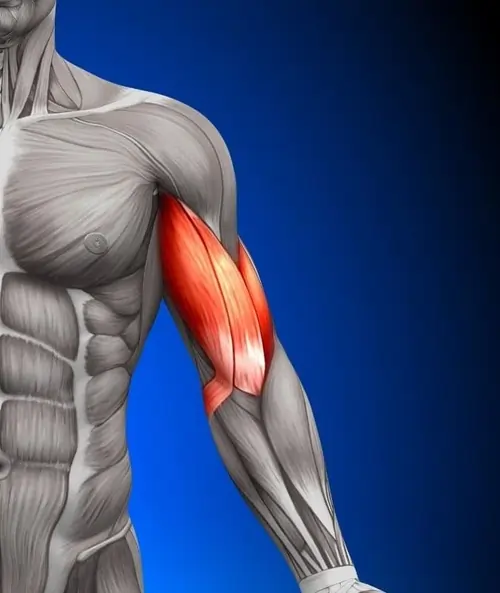
Exercise Therapy
- A sound, independently tailored exercise prescription is a basis for the management of Diabetes Mellitus (DM).
Salient Points
- It is recommended that people with Diabetes Mellitus (DM) must have regular aerobic exercise and strength training to reassure positive adaptations in the control of blood glucose concentration, insulin action, muscular strength & exercise tolerance.
- Importance of different modes of exercise in patients with type 2 diabetes – increases the uptake of glucose by muscles, improves utilization, alters lipid levels, improves high-density lipoprotein, and decreases triglyceride and total cholesterol.
- Exercise assists people to overcome disability by curing, treating, and rehabilitating neuromuscular complications like neuropathies, skin breakdown, foot ulcers, arthritis, other joint pains, frozen shoulder, back pain, and osteoarthritis associated with Diabetes Mellitus (DM).
- Moderate to great levels of different modes of exercise such as cardiorespiratory fitness exercises, aerobic exercise, and progressive resistance exercises are also associated with substantially decrease morbidity and mortality in men and women with diabetes.
Guidelines for a sound exercise program are as follows:
- Do not exercise if the blood glucose level is reduced to 100 mg/dl or greater than 250 mg/dl.
- Preferably, exercise indoors rather than outdoors to minimize the risk of integumentary and musculoskeletal trauma, as well as for the patient to have immediate access to important things to address hypoglycemia, hyperglycemia, or diabetic ketoacidosis.
- Patients are greatly advised to wear the medical tag for diabetics every time they come out of their house to go somewhere else.
- Every time have a carbohydrate snack at hand during each exercise session. A glass of orange juice or milk is a better lift for a patient who is experiencing hypoglycemia.
- Exercise at a normal temperature. Ne’er exercises in extreme temperatures.
- For Type 1 (Insulin Dependent) patients, ne’er exercise during the high times of insulin. Collaborate with the nurse in charge of the patient discussing the type of insulin administered.
- Type 2 diabetics are advised to have an average of 30 (thirty) minutes of exercise timing per session.
- Always wear perfect footwear & exercise in a safe & secure environment.
- Type 1 diabetics may require to reduce insulin or increase food intake prior to the beginning of an exercise program. Physical Therapists must coordinate with the monitoring physician for this case.
- During prolonged exercise timing, 10-15 grams of carbohydrate snack is recommended every 30 minutes.
- Clients who are on Sulfonylureas are red flags causes it can cause exercise-induced hypoglycemia. Closely coordinate with the monitoring physician if this was missed previous to the referral.
- Menstruating women require improved insulin during menses, especially if they are not active.
- There should be no short-acting insulin injections close to the muscles to be exercised within 1 (one) hour of exercise.
- Patients should eat two hours before exercising. If planning to exercise later meal, patients must wait 1 (one) hour prior to starting.
- Patients must always carry their personal portable blood glucose monitor. They must check their glucose levels previous and later exercise.
- Patients are advised to drink 17 oz. of fluid after the previous exercise.
- If blood glucose is reduced to 100 mg/dl but not decreased to 70mg/dl, the physical therapist may provide a carbohydrate snack and then recheck the glucose level after 15 minutes.
- Make sure exercise does not contribute to unimportant stress for the patient. Stress improves insulin requirements. A low progression from aerobic and resístance exercises is the key.
- Avoid exercising delay at night.
- If faced with an unexpected and difficult situation wherein the physical therapist is in doubt whether the patient is experiencing hyperglycemia or hypoglycemia, always give a glass of orange juice or milk or a carbohydrate snack. This is the safest action because this can relieve hypoglycemia (if it is indeed) and can not harm it if it is hyperglycemia.
- Exercise 5 (five) times a week as maintenance (or at least every other day) and at the same schedule/time, preferably.
- As much as possible, the patient must not exercise alone, so that there will always be someone to assist in unexpected conditions.
- Best examples of carbohydrate snacks (10-15 grams of carbohydrates) are half (1/2) a cup of fruit juice or cola, 8 oz. of milk, 2 (two) packets of sugar, and 2 oz. tube of honey or cake deco gel.
When to see a medical professional?
- If you notice symptoms of diabetes or monogenic diabetes in your baby, child, or teen, tell your doctor. This is especially right if there is a family history of diabetes or monogenic diabetes.
- Tell your doctor about risk factors and what to look out for. You may be referred to a pediatric endocrinologist, a doctor who specializes in diagnosing and treating hormone problems in young people, involving diabetes.
Is monogenic diabetes curable?
- Since Maturity-onset diabetes of the young (MODY) is caused by a genetic mutation, a genetic test can also help diagnose it. This testing will determine the exact type of Maturity-onset diabetes of the young (MODY). Maturity-onset diabetes of the young (MODY) is caused by a genetic mutation passed on through the family. There is currently no way to prevent or cure it, yet it can be managed and predicted.
Takeaway
- Monogenic diabetes is a form of diabetes caused by a single gene transmutation rather than multiple. Monogenic diabetes may be managed differently than the more common polygenic types 1 and 2 and does not always require insulin treatment.
- Monogenic diabetes is treatable, yet an accurate diagnosis is essential to getting the proper care. Knowing your family’s medical history of diabetes and getting genetic testing done can assist confirm the presence of this condition. Knowing what symptoms to watch out for, especially in infants and young adults, can also assist identify and treat monogenic diabetes as soon as possible.
- Research into this infrequent type of diabetes is ongoing. Your healthcare team (doctor) will work with you to figure out the best plan for your sub-type of monogenic diabetes.
FAQs
Maturity-onset diabetes of the young (MODY) is a rare form of diabetes that is different from both type 1 and type 2 diabetes, and runs strongly in families. Maturity-onset diabetes of the young (MODY) is caused by a mutation (or change) in a single (one) gene. If a parent has this gene mutation, any child they have has a 50% chance of inheriting it from them.
Genetic testing for monogenic diabetes includes providing a blood or saliva sample from which a DNA link is isolated. The DNA is analyzed for exchanges in the genes that cause monogenic diabetes. Genetic testing is done by specialized labs.
Monogenic diabetes is a rare type of diabetes caused by a change or mutation to a single (one) gene. It differs from type 1 or type 2 diabetes, and often needs genetic testing for an accurate diagnosis. In monogenic diabetes, insulin production is reduced. This causes glucose (blood sugar) levels to rise.
There is currently no way to prevent or cure it, but it can be managed and predicted.
A typical patient with glucokinase–maturity-onset diabetes of the young (GCK-MODY) commonly maintains good β-cell function and has a subacute or incidental presentation without ketosis. They are commonly non-obese without features of insulin resistance (IR) such as hypertension, or fatty liver.
GCK-MODY is a very mild type of condition. People with this type have slightly elevated blood sugar levels, particularly in the morning previous eating (fasting blood sugar). However, affected individuals sometimes have no symptoms related to the disorder, and diabetes-related complications are extremely rare.
Monogenic diabetes is a rare type of diabetes that’s caused by a single (one) gene mutation. There are currently over 10 different types of MODY and with new genetic testing, more are being uncovered. It accounts for about 1-2% of all diabetes cases, though its prevalence may actually be up to 5%.
Brittle Diabetes (Labile Diabetes) Brittle diabetes mellitus (or labile diabetes) is a term used to describe particularly hard-to-control type 1 diabetes. Those people who have brittle diabetes are more likely to experience sometime, extreme swings in blood glucose levels, causing hyperglycemia or hypoglycemia.