Distal Muscular Dystrophy (DD)
Table of Contents
What is distal muscular dystrophy?
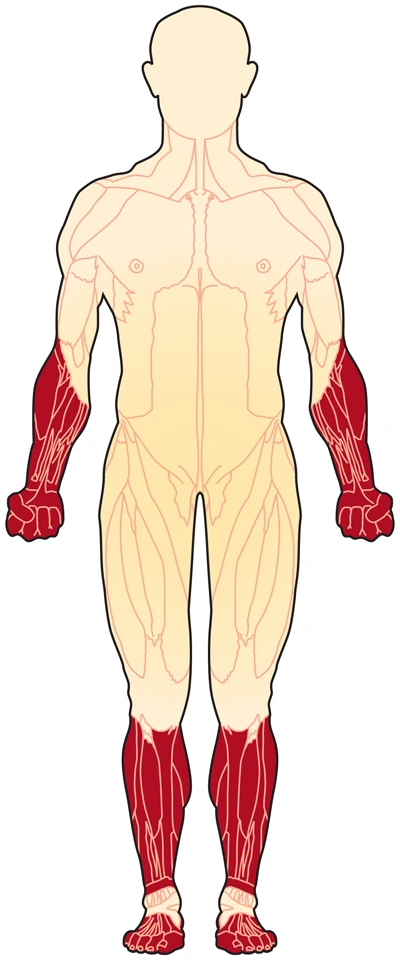
Distal muscular disease (DD) could also be a gaggle of rare diseases that affect your muscles (genetic myopathies). DD causes weakness that starts within the lower arms and legs (the distal muscles). It may progressively spread to the affected area of your body. The muscles shrink (atrophy).
DD has several forms. DD usually appears between ages 40 and 60. But it can sometimes show as early because of the adolescent years. DD affects both men and women.
Classification of Distal Muscular Dystrophies
| Types of DD | Cause | Inheritance Pattern |
| Welander distal myopathy | abnormalities in chromosome 2 gene | dominant |
| Finnish (tibial) distal myopathy | titin abnormalities | dominant |
| Miyoshi distal myopathy | dysferlin abnormalities | recessive |
| Nonaka distal myopathy; also called hereditary inclusion-body myositis type 2 (HIBM2) | GNE abnormalities | recessive |
| Gowers-Laing distal myopathy | MYH7 abnormalities | dominant |
| Hereditary inclusion-body myositis type 1 (HIBM1) | unknown | dominant |
| Distal myopathy with vocal cord and pharyngeal weakness | abnormalities in chromosome 5 gene | dominant |
Causes/Inheritance of Distal Muscular Dystrophy
What causes distal genetic abnormality (DD)?
All types of hereditary conditions are inherited — that’s, they’re caused by mutations (changes) in a person’s genes. Our genes are manufactured from DNA and reside in our chromosomes. Each gene contains the “recipe” for a distinct protein and its variations, and these proteins are necessary for our bodies to function correctly. When a gene features a mutation, it’s going to make a defective protein or none the least bit. most typically, missing or defective proteins within the muscles prevent muscle cells from working properly, resulting in symptoms of hereditary disease, including muscle weakness and wasting over time.
The different kinds of DD are caused by many genetic defects, not all of which are yet known. a number of the DDs are given different names supported by various symptoms but actually could also be caused by defects on the identical gene.
What are the inheritance patterns in DD?
Most varieties of DD are inherited in an autosomal dominant pattern, but some follow a recessive pattern of inheritance. In brief, if a disease is recessive, two copies of the defective gene (one from each parent) are required to supply the disease. Both parents would be a carrier of the gene fault, but wouldn’t have the disease. If a disease is dominant, then only 1 copy of the inherited disorder is required to cause the disease. Anyone with the gene fault will have disease symptoms and might pass the disorder to children.
Many times dystrophy appears to possess occurred “out of the blue,” but truly, one or both parents could also be carriers, silently harboring the modification. Often parents don’t know they’re carriers of disease until they need a baby who has the disease.
The genes in your body generally occur in pairs. You inherit a duplicate from each parent. A change in exactly 1 copy of the gene is enough to cause most kinds of DD. this suggests the disease is passed down in an exceedingly dominant manner. In another class of DD, the disease occurs as long as you have got changes in both of the genes.
These recessive varieties of DD include Nonaka distal myopathy and Miyoshi genetic abnormality. In Finnish distal myopathy, people with 1 copy of the changed gene have a weakness within the muscles within the fronts of the lower legs (the tibial muscles) after age 40. People with Finnish DD who inherit 2 changed genes have muscle problems in childhood. they will need a wheelchair by age 30.
A mutation within the MATR3 gene has been detected in people with distal myopathy 2. This gene provides instructions for creating a protein called matrin 3, which is found within the nucleus of the cell as a part of the nuclear matrix. The nuclear matrix may be a network of proteins that has structural support for the nucleus and aids in several important nuclear functions.
The role of the matrin 3 protein is unknown. This protein can bind to (attach) RNA, which could be a chemical first cousin of DNA. Some studies indicate that matrin 3 binds and stabilizes a sort of RNA called messenger RNA (mRNA), which provides the genetic blueprint for proteins. Matrin 3 might also bind certain abnormal RNAs which may cause nonfunctional or harmful proteins, thereby blocking the formation of such proteins. Other studies suggest that the matrin 3 protein could also be involved in cell survival.
The MATR3 point mutation identified in people with distal myopathy 2 changes one protein building block (amino acid) within the matrin 3 protein. The effect of this mutation on the function of the protein is unknown, although one study suggests that the mutation may change the placement of the protein within the nucleus. Researchers are working to work out how this chromosomal mutation results in the signs and symptoms of distal myopathy 2.
Signs and Symptoms of Distal Muscular Dystrophy
The specific symptoms and progression of the distal myopathies differ greatly, even between members of the same family. Slowly progressive degeneration and weakness of the voluntary distal muscles cause these diseases. In such cases, muscles including different proximal muscles may become involved.
Vocal cord and pharyngeal weakness: Symptoms usually start between ages 35 and 60 with weakness in the hands, legs, and voice, similarly to difficulty swallowing.
Finnish (tibial) distal myopathy: Weakness usually starts after age 40 within the lower extremities, especially within the muscles above the tibia, the larger bone of the leg.
Gowers-Laing distal myopathy: The onset is from childhood to 25 years old. It begins with weakness in leg and neck muscles and advances to the upper leg, hands, and neck muscles.
Hereditary inclusion-body myositis (myopathy) type 1 (HIBM1): HIBM1 generally starts between the ages of 25 and 40. It starts affecting the muscles of the thigh and also the muscles that are custom to lift the highest of the foot, later expanding out advance.
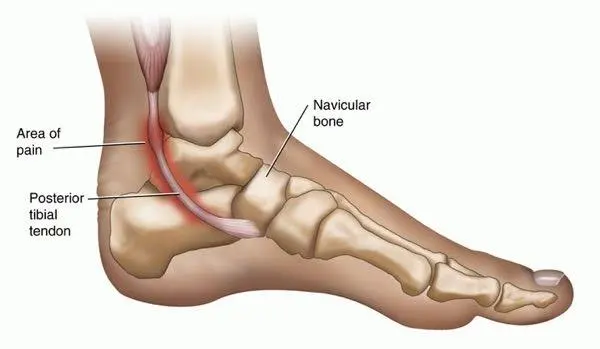
Miyoshi distal myopathy: Symptoms start between the ages of 15 and 30, with weakness within the lower extremities, especially the calves.
Nonaka distal myopathy: Often in families of Japanese descent, symptoms start between ages 20 and 40. First symptoms appear within the front lower leg muscles then spread to the upper arm and leg so the neck muscles.
VCP (valosin-containing protein) myopathy (IBMPFD): It is caused by a mutation that causes various conditions, it shows as body myositis, osteitis deformities of bone, or frontotemporal dementia. people can have one, two, or all of the conditions.
Welander distal myopathy: Symptoms are between ages 40 and 50 and affect the upper and lower extremities.
What happens to someone with a distal hereditary disease (DD)?
- The main symptom is a weakness that typically starts within the lower arms or legs.
- vocal cord and pharyngeal (throat) weakness affect the voice, hands, and legs.
- The first symptom of distal muscular dystrophy (DD) is weakness within the distal muscles (those far from the hips and shoulders like those within the hands, feet, lower arms, or lower legs).
- Muscle mass within the affected regions may become visibly wasted (decreased in size).
- In some cases, arms, legs,s or trunk muscles may weaken to the purpose where mobility and range of motion are limited.
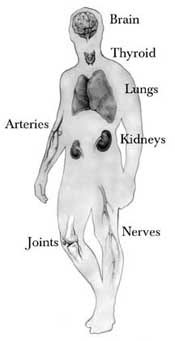
- Some types of distal hereditary disease affect the muscles used for speaking or swallowing and may affect the center.
For most varieties of inherited diseases, symptoms start to point out in childhood or within the teen years. In general, children with the condition:
- Fall down often
- Have weak muscles
- Have muscle cramps
- Trouble in getting up, climbing stairs, running, or jumping
- Walk on their toes or waddle
Some also will have symptoms like:
- A curved spine (called scoliosis)
- Droopy eyelids
- Heart problems
- Trouble breathing or swallowing
- Vision problems
- Weakness within the muscles of the face
Prognosis
The prognosis for DD will rely on the subtype an individual has. It also depends on the progression of the disorder in individuals. Some people undergo slow progression and have an awfully mild disorder course, while others may have important weaknesses and impairment.
For example, in Finnish hereditary disease, thanks to muscle weakness, the flexibility to run is also lost by age 30.
In contrast, in some disorders like Welander distal myopathy, muscle weakness can range from mild to severe, so those with mild weakness can keep movement quite well.
In Laing distal myopathy, the progression is disorder improbability slow that even into an identity’s 60s, wheelchairs or movement aids don’t appear to be needed. Someone with VCP disorder will have to appear in conditions that may affect the bone or brain, impacting their prognosis.
Diagnosis of Distal Muscular Dystrophy
Your health service provider will start by taking your health history and asking about recent symptoms, past health conditions, and family health history. Your provider will provide you with a physical exam and test your muscle strength. you will need other tests.
These include:
- Blood tests for muscle enzymes like creatine kinase
- DNA blood tests for known DD changes
- Muscle biopsy to seem for the precise problem within the muscle cells
- Electromyography to live the electrical activity of the muscles
- MRI or ultrasound tests to seem at the muscles
- You may first see your main healthcare provider and then again be observed by a neurologist. Some neurologists have specific training to treat muscles and nerve diseases. Your healthcare provider also may refer you to a clinic that focuses on managing DD.
Diagnosing any sort of genetic defect involves first taking an in-depth medical and case history, and doing a physical exam. The exam is particularly important in seeing any pattern of weakness.6
Diagnostics include the following:
Nerve conduction studies and electromyography (EMG): These tests use electricity sent through needles inserted into muscles to gauge the electrical activity within the muscles and nerves.
Creatine kinase (CK) test: CK leaks out of damaged muscles, so when this enzyme is found within the blood, muscle damage is present for a few abnormal reasons. This test shows that it’s the muscles that are full of weakness.
Muscle biopsy: this might be done to further explore the results of the CK test. This involves taking a tiny low piece of muscle and examining it within the lab. this could show the muscle proteins present, any abnormal levels of proteins, and if they’re within the right places, and it can give clues on the genes that will be involved.
Genetic testing: this can be through with a blood sample. All sorts of genetic disorders are inherited and have different mutations or abnormalities. Genetic testing can help to work out the sort of DD someone has.
Tests of muscle strength, reflexes, and coordination. These help doctors rule out other problems with their system.
Imaging can show the standard and amount of muscle in your child’s body.
They may get:
MRI, or resonance imaging. It uses powerful magnets and radio waves to form pictures of its organs.
Ultrasound uses sound waves to create pictures of the within of the body.
Treatment of Distal Muscular Dystrophy
Medical treatment
Medicines can help ease symptoms.
They include:
- Eteplirsen (Exondys 51), golodirsen (Vyondys53), and vitolarsen (Viltepso) for treating DMD. they’re injection medications that help treat individuals with a selected mutation of the gene that ends up in DMD, specifically by increasing dystrophin production. confer with your child’s doctor about possible side effects.
- Anti-seizure drugs that reduce muscle spasms.
- Blood pressure medicines that help with heart problems.
- Drugs that turn down the body’s system, called immunosuppressants; will slow damage to muscle cells.
- Steroids like prednisone and deflazacort (Emflaza) cut down muscle damage and may help to breathe better for the child. they will cause serious side effects, like weak bones and a better risk of infections.
- Creatine, a chemical normally found within the body, which will help supply energy to muscles and improve strength for a few people. Ask your child’s doctor if these supplements are a decent idea for them.
- Surgery can help with different complications of hereditary conditions, like heart problems or trouble swallowing.
- Scientists are also searching for new ways to treat genetic diseases in clinical trials. These trials test new drugs to determine if they’re safe and if they work. They often are how for people to do new medicine that won’t available to everyone. Your doctor can tell you if one among these trials may well be a decent acceptable child.
Physiotherapy Treatment
There is no cure for DD. But supportive care can facilitate your keep your strength and adaptability. physiotherapy is very important to stay in your range of motion. physical therapy can help with ways to adapt to activities like eating, walking, or computer use. you furthermore may get help from certain aids. These include:
- Lower-leg braces to treat foot drop
- Other lightweight leg braces for support
- Handwriting aids
- Mouse and keyboard alternatives
- Cuffs, braces, openers, and other adaptive devices
Several kinds of therapy and assistive devices can improve the standard and sometimes the length of life in folks that have a distal genetic disease.
Examples include:
- Range-of-motion and stretching exercises: hereditary disease can restrict the flexibleness and mobility of joints. Limbs often draw inward and become fixed therein position. Range-of-motion exercises can help to stay joints as flexible as possible.
- Low-impact aerobics, like walking and swimming, can help maintain strength, mobility, and general health. Some varieties of strengthening exercises also could be helpful. But it is vital to speak to your doctor first because some styles of exercise can be harmful.
- Braces or mobility devices: Braces can help keep muscles and tendons stretched and versatile, slowing the progression of contractures. Braces may aid mobility and performance by providing support for weakened muscles. Devices like lower leg braces can help with symptoms like foot drop (difficulty moving the front part of the foot), and other leg braces can provide support and stability. Power scooters, walkers, canes, and wheelchairs can make movement easier and relieve fatigue DD.
- Occupational therapy: physiotherapy can help people adapt to everyday activities like eating, using the pc, and getting dressed. The therapist can show the way how to use assistive devices, options, or tools to assist with daily activities.
- Speech therapy: it’ll teach them easier ways to speak if their throat or facial muscles are weak.
- Respiratory therapy: It can help if your child has trouble breathing. They’ll learn ways to create it easier to breathe or get machines to assist
- Assistive devices for the computer/keyboard: These can facilitate your type more quickly if you’ve got weakness within the hands and/or arms.
If a person has problems swallowing, assistance is also needed to stop aspiration (when food or drink are breathed into the lungs) or choking (blocking of the airway). If the guts are affected, this must be monitored. Because each subtype can have such different symptoms, the therapies can vary widely, looking on a person’s needs.
Exercises:
- Joint-Blocking Exercises
Joint-blocking exercises, as demonstrated by Kaiser Permanente, prevent adjacent joints from moving because the affected joint flexes and extends.
Perform one DIP-joint-blocking exercise by placing your hand palm-up on a table and using your other hand to stabilize the center section of your affected finger — just below the fingertip joint.
While holding the remainder of your finger straight, slowly bend and straighten only the tip joint of your finger.
Repeat this blocking exercise with each of your fingers and hold your required position for 3 to 5 seconds before relaxing.
- Range-of-Motion Exercises
Several range-of-motion (ROM) exercises can increase mobility and reduce pain in your DIP joints as a part of your distal ginglymus injury treatment.
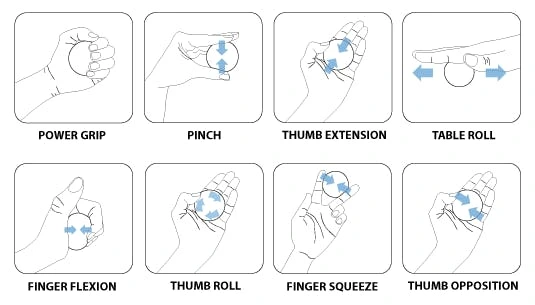
Upper Limb exercises:
(1) Finger Flexion
Grasp the painful finger along with your unaffected hand.
Place your thumb on the highest side of the affected finger below the highest joint.
Using your forefinger, push only the tip of your finger up, until you are feeling a simple stretch.
Complete this exercise with all your fingers 8 to 12 times.
(2) Finger Extension
Place your affected hand flat on a table.
Lift and lower one finger at a time without working the table.
Repeat this exercise 8 to 12 times.

(3) Passive Stretching
Hold the tip of your finger or toe together with your opposite hand.
Gently stretch and bend the joint until you are feeling a stretch.
Hold for 10 seconds and repeat thrice.
Complete this stretch several times in the morning and several other times during the hours of darkness.
(4) Make a Fist
Hand and finger exercises can help strengthen your hands and fingers, increase your range of motion, and provide you pain relief. Stretch only until you’re feeling tightness. you mustn’t feel pain. Start with this easy stretch:
Make a mild fist, wrapping your thumb across your fingers.
Hold for 30 to 60 seconds. Release and spread your fingers wide.
Repeat with both hands a minimum of fourfold
(5) Finger Stretch
Try this stretch to assist with pain relief and to boost the range of motion in your hands:
Place your hand on a table or other flat surface with your palm down.
Gently straighten your fingers as flat as you’ll against the surface without forcing your joints.
Hold for 30 to 60 seconds so release.
Repeat a minimum of fourfold with each hand.

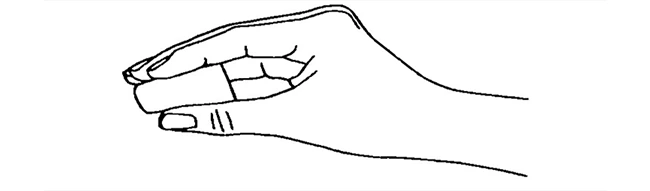
(6) Claw Stretch
This stretch helps to improve the range of motion of your fingers.
Hold your gift ahead of you, palm facing you.
Bend your fingertips all the way down to touch the bottom of every finger joint. Your hand should look like a touch of a claw.
Hold for 30 to 60 seconds and release. Repeat a minimum of fourfold on each hand.
(7) Grip Strengthener
This exercise can make it easy to open the knobs of the door and hold things without dropping them.
Hold a soft ball in your palm and squeeze it as hard as you’ll.
Hold for some seconds and release.
Repeat 10 to fifteen times on each hand. Do this exercise a few times every week, but get break your hands for 48 hours in between sessions. If your thumb is broken please don’t try this exercise.
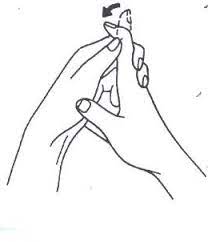
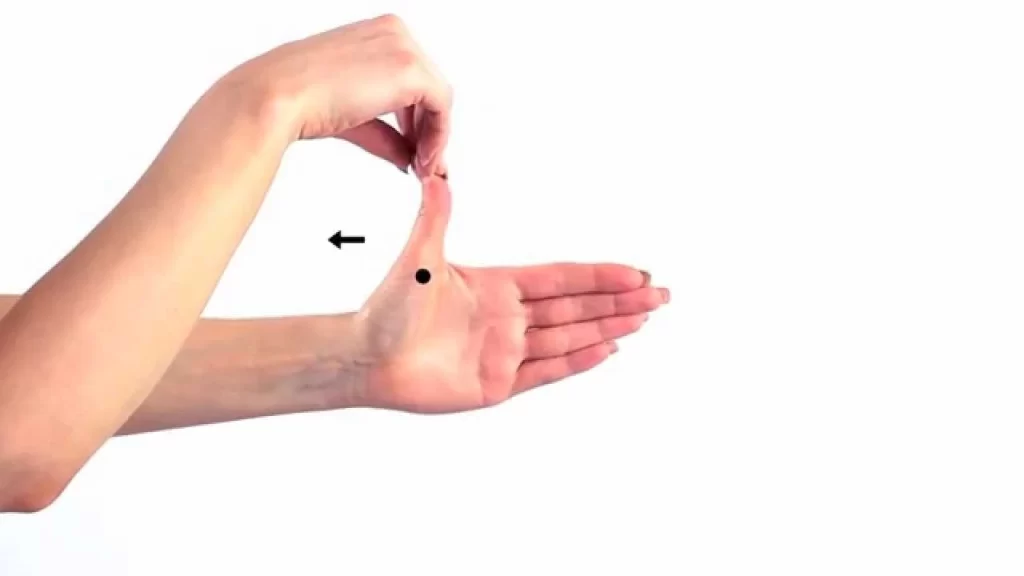
(8) Pinch Strengthener
This exercise is to helps improve and strengthen the muscles of the fingers and thumb. It can facilitate your turning keys, opening food packages, and using the gasoline pump more easily.
Pinch a soft foam ball or some putty between the guidelines of your fingers and your thumb.
Hold for 30 to 60 seconds.
Repeat 10 to fifteen times on both hands. do that exercise two to a few times every week, but rest your hands for 48 hours in between sessions. Don’t try this exercise if your thumb joint is broken.

(9) Finger Lift
Use this exercise to assist increase the range of motion and suppleness of your fingers.
Place your hand on a table or other flat surface with your palm down.
Gently lift one finger at a day without working on the table then lower it.
You can also lift all of your fingers and thumb directly, and so lower.
Repeat eight to 12 times on each hand.
(10) Thumb Extension
Strengthening the muscles of your thumbs can facilitate your grab and lifting of heavy things like cans and bottles.
Put your hand flat on a table. Wrap a band around your hand at the bottom of your finger joints.
Gently move your thumb off from your fingers as far as you’ll.
Hold for 30 to 60 seconds and release.
Repeat 10 to fifteen times with both hands. you’ll be able to do that exercise two to a few times every week, but rest your hands for 48 hours in between sessions.
(11) Thumb Flexion
This exercise helps to increase the range of motion in the thumbs.
Start along with your give ahead of you, palm up.
Extend your thumb far from your other fingers as far as you’ll. Then bend your thumb across the palm so it touches the bottom of the small finger.
Hold for 30 to 60 seconds.
Repeat a minimum of fourfold with both thumbs.

(12) Thumb Touch
This exercise helps increase the range of motion in your thumbs, which helps with activities like learning your toothbrush, fork, spoon, and pens once you write.
Hold your give before you, together with your wrist straight.
Gently touch your thumb to every one of your four fingertips, one at a time, making the form of an “O.”
Hold each stretch for 30 to 60 seconds. Repeat a minimum of fourfold on each hand.
(13) Thumb Stretches
Try these two stretches for your thumb joints:
Hold your give, palm facing you. Gently bend the tip of your thumb down toward the bottom of your index. Hold for 30 to 60 seconds. Release and repeat.
Hold this position, and palm facing you. Gently stretch your thumb across the palm using the lower thumb joint. Hold for 30 to 60 seconds. Release and repeat fourfold.
(14) An Exercise Tip
If hands and fingers feel stiff and painful, try to warm them up before starting the exercise. this may make it easier to maneuver and stretch. Use a warmer or soak them in warm water for about five to 10 minutes. Or, for a deeper warmth, rub some oil on your hands, place on a pair of rubber gloves, then soak them in warm water for some minutes.

(15) Play With Clay
Playing with putty or clay could be a good way to extend the range of motion in your fingers and strengthen your hands at the identical time. And it won’t even want exercise. Squish the clay into a ball and, roll it into long “snakes” along with your palms, or use the fingertips to pinch spikes on a dinosaur.
Lower Limb Exercises:

(1) Toe splay
This movement will facilitate your gain control over your toe muscles.
Sit in an exceedingly straight-backed chair along with your feet gently resting on the ground.
Spread all of your toes apart as far as comfortable. Hold for five seconds.
Repeat 10 times.
You can make this exercise harder by looping an elastic device around the toes of every foot.
(2) Toe raise
This three-part exercise will start to urge your toes and feet to move.
Sit straight with a backed chair along with the feet flat on the ground.
Keep your toes flat on the bottom and lift your heels until only the balls of your feet and toes touch the bottom. Hold for five seconds.
Point your toes in order that only the ends of your big and second toes touch the bottom. Hold for five seconds.
Keep your heel off the bottom and roll your toes under in order that the tops of your toes touch the bottom. Hold for five seconds.
Repeat each position 10 times.
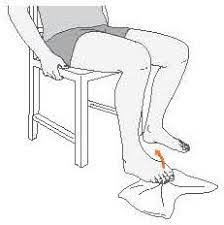
(3) Toe extension
This stretch is sweet to forestall or treat plantar fasciitis, which causes heel pain.
Sit in an exceedingly straight-backed chair with your feet flat on the ground.
Pick one foot and place it on your opposite thigh.
Grab your toes with one hand and pull them up toward your ankle until you’re feeling a be the underside of your foot and in your heel cord.
Massage the arch of your foot together with your other hand during the stretch. Hold for 10 seconds.
Repeat 10 times on each foot.
(4) Toe curls
This exercise will strengthen the muscles on the highest of your feet and toes.
Sit in an exceedingly straight-backed chair together with your feet flat on the ground.
Lay a kitchen towel or face towel on the ground ahead of you therefore the short end is at your feet.
Put the toes of 1 foot on the tip of the towel, and scrunch your toes so you pull the towel toward you.
Repeat five times with each foot.
You can increase the issue of this exercise by placing a little weight (like a can of soup) on the far end of the towel.
(5) Marble pickup
This exercise will strengthen the muscles on the underside of your feet and toes.
Sit in a very straight-backed chair together with your feet flat on the ground.
Place 20 marbles and a little bowl on the ground before you.
Pick up one marble at a time together with your toes and place it within the bowl. Use one foot to choose up all 20 marbles.
Repeat with the opposite foot.

(6) Big-toe stretch
Keep a good range of motion in your toe with this three-part stretch. It feels good after having the feet packed in dress shoes all day.
Sit in an exceedingly straight-backed chair with your feet flat on the ground.
Pick one ad and place it on the opposite thigh.
Gently use your fingers to stretch your hallux up, down, and to the side aloof from the opposite toes. Hold this stretch position in each direction for 5 seconds.
Repeat 10 times in each direction.
Repeat with the alternative foot.

(7) ball roll
Rolling the underside of your foot on a tough ball can ease arch pain and treat plantar fasciitis.
Sit in a straight-backed chair with your feet flat on the ground.
Place a ball on the ground near your feet.
Put your foot on top of the ball and roll it around, massaging the underside of your foot.
Increase or decrease pressure pro re nata.
Roll for 2 minutes on each foot.
If you don’t have any tennis balls, you can also use frozen water.
(8) Achilles stretch
The cord that runs up your heel into your calf muscles is termed the tendon. Keeping it flexible, can prevent pain in the foot, ankle, and leg.
Stand toward the facing a wall, with palms on the wall, and arms outstretched.
Place one foot back behind with the knee straight, and bend the knee on the other leg.
After then, Lean forward from the hips until you feel the stretch in your Achilles tendon and calf muscle.
Change your stance if necessary to feel the pull while keeping your heels on the ground.
To feel the stretch in a very different place, bend the rear knee slightly and push your hips forward.
Hold the stretches for 30 seconds each and repeat thrice.
Switch legs and repeat.

(9) Sand walking
Walking barefoot through sand strengthens and stretches your feet and toes and provides a good calf workout. Walking in sand is more tiring than walking on hard paths, so confirm you switch around before you’ve worn yourself out.
Find some sand — for instance, at a beach, desert, or court.
Take off your shoes and socks.
Walk.
Risk factors of Distal hereditary disease
Because the genetic defects that cause DD are usually passed on through families (hereditary), you have got the next risk for DD if the condition runs in your family. Some styles of DD are rather more common in certain groups. as example, Nonaka distal myopathy most ordinarily appears in people of Japanese descent.
Taking Care of Your Child
It’s hard when your child loses strength and can’t do the items other kids can do. The genetic defect could be a challenge, but it doesn’t need to keep your child from enjoying life.
There are many belongings you can do to assist them to feel stronger and obtain the foremost out of life.
Eat right: A healthy, It is well-balanced diet is nice for your child normally. It’s also important for helping them lodge in a healthy weight, which might ease breathing problems and other symptoms. If it’s hard for them to chew or swallow, sit down with a dietitian about foods that will be easier to eat.
Stay active: Many Exercises can help to improve a child’s muscle strength and make them feel better. Try low-impact activities like swimming.
Get enough sleep: Ask the therapist about some beds or pads that may make your child easier and rested.
Use the proper tools: Many tools such as wheelchairs, crutches, or electric scooters can help your child if they need trouble walking.
The disease will presumably have an enormous impact on your family: Remember that it’s okay to ask a doctor, counselor, family, or friends for help with any stress, sadness, or anger you will feel. Support groups also are good places to speak to people who have lived with hereditary conditions. they’ll help your child connect with others like them and provide you and your family with advice and understanding.
Complications
- Trouble walking. Some people with genetic defects eventually have to use a wheelchair.
- Trouble using arms.
- Shortening of muscles or tendons around joints (contractures).
- Breathing problems.
- Curved spine
FAQ
Is distal muscular dystrophy curable?
How is the distal congenital disease treated? there’s no cure for DD. But supportive care can facilitate your keep your strength and adaptability. physiatrics is very important to stay in your range of motion.
What does distal muscular dystrophy feel like?
Typically, the primary symptom of distal dystrophy (DD) is weakness within the distal muscles — those farthest far away from the hips and shoulders like those within the hands, feet, lower arms, or lower legs. With time, other muscle groups may become affected moreover. Intellect isn’t affected during this disease.
How does someone get muscular dystrophy?
In most cases, genetic disease (MD) runs in families. it always develops after inheriting a faulty gene from one or both parents. MD is caused by mutations (alterations) within the genes chargeable for healthy muscle structure and performance.
What organs does distal muscular dystrophy affect?
Many individuals eventually lose the flexibility to run. Some sorts of MD also affect the center, digestive system, endocrine glands, spine, eyes, brain, and other organs. Respiratory and cardiac diseases may occur, and a few people may develop a swallowing disorder.
Does weather affect muscular dystrophy?
Winter weather shouldn’t directly affect muscular dystrophies. However, the restrictions imposed by muscle weakness of any origin are magnified during the conditions of winter weather including the cold. These problems will resolve once these conditions change as do the seasons.
What is the anticipation of somebody with distal muscular dystrophy?
Until recently, children with Duchenne inherited disorder (DMD) failed to often live beyond their teens. However, improvements in cardiac and respiratory care mean that lifespan is increasing, with many DMD patients reaching their 30s and a few living into their 40s and 50s.
Does muscular dystrophy affect the brain?
only Congenital muscular dystrophies (CMDs) are a good group of muscular disorders that manifest with a very early onset of muscular weakness, sometimes associated with severe brain involvement.