CRANIAL NERVE 3,4 AND 6
Table of Contents
CRANIAL NERVE: 3,4 AND 6
occulomotor, trochlar and abducens
OCULOMOTOR:
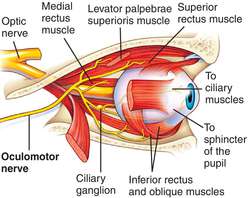
The oculomotor nerve is the third cranial nerve (CN III). It enters the orbit via the superior orbital fissure and innervates extrinsic eye muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the intrinsic eye muscles that enable pupillary constriction and accommodation (ability to focus on near objects as in reading). The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in the control of eye movement.
Superior branch
The superior branch of the oculomotor nerve or the superior division, the smaller, passes medially over the optic nerve. It supplies the superior rectus and levator palpebrae superioris.
Inferior branch
The inferior branch of the oculomotor nerve or the inferior division, the larger, divides into three branches.
TROCHLEAR NERVE:

-The trochlear nerve, also called the fourth cranial nerve or CN IV, is a motor nerve (a somatic efferent nerve) that innervates only a single muscle: the superior oblique muscle of the eye, which operates through the pulley-like trochlea.
-The trochlear nerve carries axons of type GSE, general somatic efferent, which innervate skeletal muscle of the superior oblique muscle.
-The superior oblique muscle ends in a tendon that passes through a fibrous loop, the trochlea, located anteriorly on the medial aspect of the orbit.
ABDUCENS NERVE:
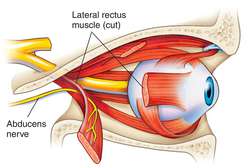
The abducens nerve is a nerve that controls the movement of the lateral rectus muscle in humans, responsible for outward gaze. It is also known as the abducent nerve, the sixth cranial nerve, sixth nerve, or simply CNVI. It is a somatic efferent nerve.
The abducens nerve supplies the lateral rectus muscle of the human eye. This muscle is responsible for outward gaze. The abducens nerve carries axons of type GSE, general somatic efferent.

Assessment of cranial nerves III, IV, and VI:
1.Pupillary light reflex
-Ask the patient to fixate on a distant target
-Shine a pen torch into each eye in turn, bringing the beam in quickly from the lateral side
-Observe both the direct (ipsilateral) and consensual (contralateral) response

2.Pupillary accommodation

– The accommodation reflex involves both convergence of the eyes (requiring adduction of both eyes) and simultaneous constriction of the eyes
-Ask the patient to look at an object held at distance
-Bring the object to within 10cm of the patient, asking the patient to follow it with their eyes
-Watch the pupils for equal convergence and constriction
-Ask the patient to look straight ahead and check for signs of nystagmus or ptosis.
3.Ocular movements
-Ask the patient to keep their head still and follow an object
-Move the object around in an H formation, assessing both horizontal and vertical gaze

-Watch the pupils to assess the eye movements and any signs of nystagmus
-Checking the conjugate gaze may also be warranted at this point
-Ensure to ask the patient to let you know if they experience any double vision throughout
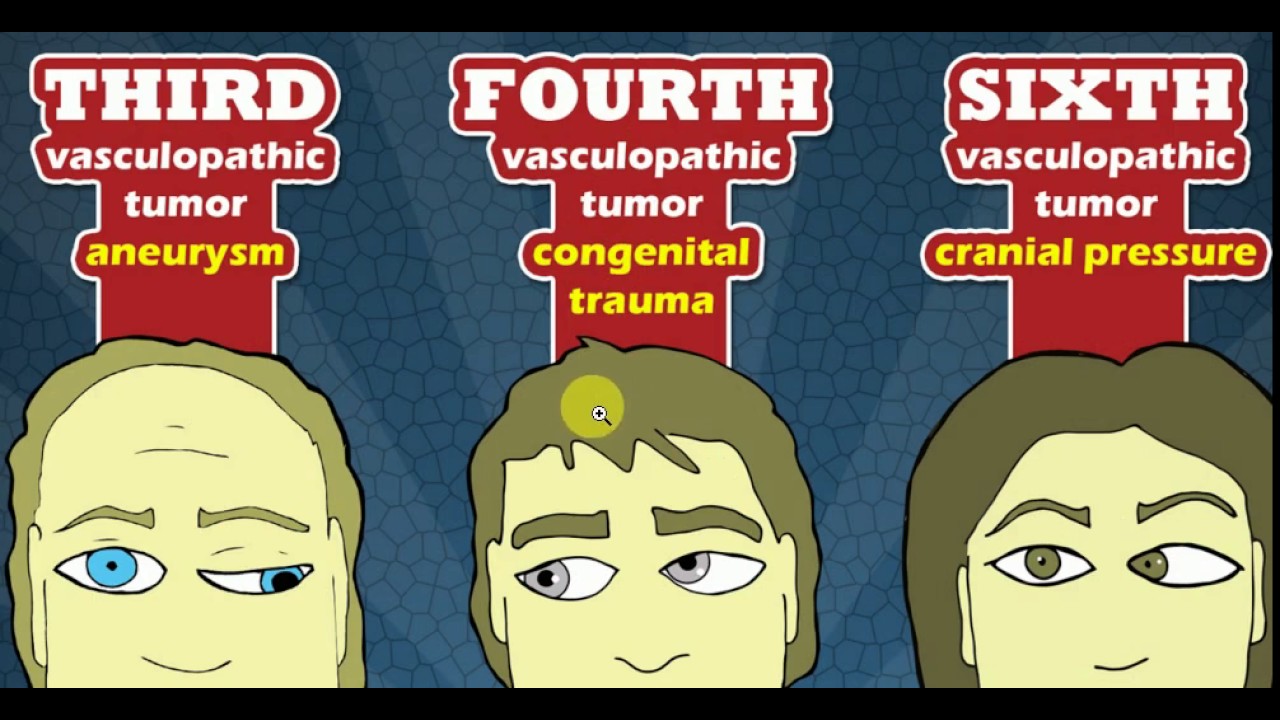
DAMAGE TO THE NERVE:
DIPLOPIA:
Diplopia is typically experienced by adults with VI nerve palsies, but children with the condition may not experience diplopia due to suppression. The neuroplasticity present in childhood allows the child to ‘switch off’ the information coming from one eye, thus relieving any diplopic symptoms. Whilst this is a positive adaptation in the short term, in the long term it can lead to a lack of appropriate development of the visual cortex giving rise to permanent visual loss in the suppressed eye; a condition known as amblyopia.
VERTICAL DIPLOPIA:
Injury to the trochlear nerve cause weakness of downward eye movement with consequent vertical diplopia (double vision). The affected eye drifts upward relative to the normal eye, due to the unopposed actions of the remaining extraocular muscles. The patient sees two visual fields (one from each eye), separated vertically. To compensate for this, patients learn to tilt the head forward (tuck the chin in) in order to bring the fields back together—to fuse the two images into a single visual field. This accounts for the “dejected” appearance of patients with “pathetic nerve” palsies.
ESOTROPIA:

The nerve dysfunction induces esotropia, a convergent squint on distance fixation. On near fixation the affected individual may have only a latent deviation and be able to maintain binocularity or have an esotropia of a smaller size. Patients sometimes adopt a face turned towards the side of the affected eye, moving the eye away from the field of action of the affected lateral rectus muscle, with the aim of controlling diplopia and maintaining binocular vision.
NYSTAGMUS:

Nystagmus is a condition of involuntary (or voluntary, in rare cases)eye movement, acquired in infancy or later in life, that may result in reduced or limited vision.Due to the involuntary movement of the eye, it has been called “dancing eyes”.
TREATMENT:
-Treatment can be as simple as wearing an eye patch, or special glasses or contacts. Botox injections or eyelid surgery may be used to correct a squint that causes double vision. Similarly, a cataract operation may be necessary if a cataract is the cause, or dry eye treatment may help if dry eye is the cause.
-Drugs such as Botox or Baclofen can reduce some nystagmic movements, although results are usually temporary. Some people with nystagmus benefit from biofeedback training.
-Both eyeglasses and contact lenses can help people with nystagmus see better, but I have found contact lenses to be the superior alternative for many with nystagmus. With glasses, the eyes sweep back and forth over the lens centers and vision is not as clear. With contacts, however, the lens centers move with the eyes.