BRUNNSTROM APPROACH
INTRODUCTION :-
The Brunnstrom approach is a type of physiotherapy treatment used with patients with movement problems following damage to the brain and spinal cord, (central nervous system/ CNS). The Brunnstrom Approach sets out a sequence of stages of recovery from hemiplegia after a stroke. It was developed by the Swedish physical therapist Signe Brunnström, and emphasises the synergic pattern of movement which develops during recovery.
After the stroke has occurred, your muscles become weak due to the lack of coordination between the brain and body. This causes the muscle synergies to move in abnormal patterns. Most treatments offered to stroke patients will focus on trying to inhibit atypical muscle synergies and movements. The Brunnstrom Approach, on the other hand, teaches patients how to use the abnormal synergy patterns to their advantage.
PRINCIPLE :-
1st Principle – Normal movement (how a healthy individual moves) requires muscles working together (synergistically) following damage to the CNS the muscles will not work as well together. During recovery muscles will start working together better.
2nd Principle – Following damage to the CNS, movement recovery follows a specific sequence. The sequence is:
- Immediately after the onset of injury there may be no “voluntary” movement.
- Spasticity (increased muscle tone) appears, basic movement reflexes appear.
- Patient begins to gain voluntary control over their reflexes. This may cause an increase in spasticity.
- Basic movement patterns are developed. This leads to a reduction in spasticity.
- As progress continues, more complex movement patterns are learnt and there is a further decrease in spasticity.
- Spasticity disappears and individual movements become possible and coordination approaches normal.
- Normal function is restored.
STAGES :-
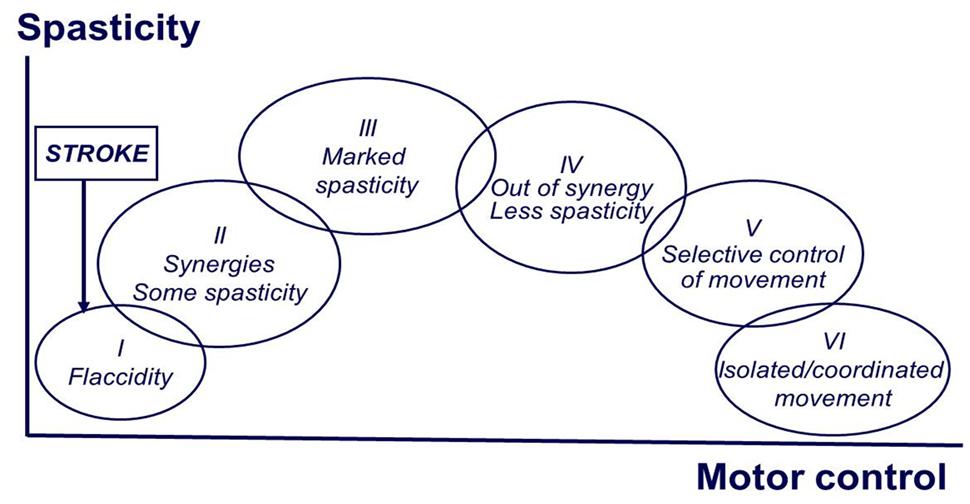
Stage 1: Flaccidity
The first stage in Brunnstrom’s Approach is the initial period of shock immediately after stroke where flaccid paralysis sets in. Flaccid paralysis (flaccidity) is the medical term for a complete lack of voluntary movement. This paralysis is caused by nerve damage that prevents the muscles from receiving appropriate signals from the brain, whether or not the brain is still capable of moving those muscles.
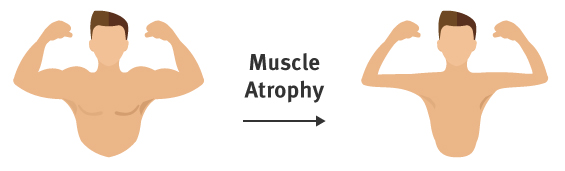
In the early state of flaccid paralysis, the stroke survivor cannot initiate any muscle movements on the affected side of their body. If this continues for long enough without intervention or physical therapy, the unused muscles become much weaker, and begin to atrophy. The medical term for this loss of muscle tone is hyptonia. Hyptonia causes weakness and sometimes numbness that seriously interferes with a patient’s quality of life. This condition also requires lifestyle modifications to protect the affected limbs from injury.
Stage 2: Starting of Spasticity
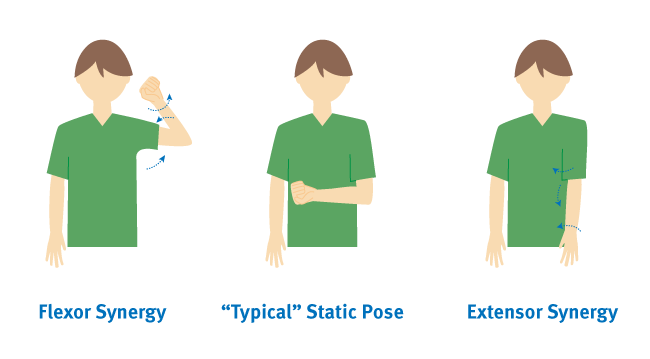
The second stage in stroke recovery marks the redevelopment of some basic limb synergies as certain muscles are stimulated or activated and other muscles in the same system begin to respond. Muscles begin to make small, spastic, and abnormal movements during this stage. While these movements are mostly involuntary, they can be a promising sign during your recovery. Minimal voluntary movements might or might not be present in stage two.
Muscle synergies result from muscles coordinating movements to perform different tasks. Because the muscles are linked, one activated muscle may lead to partial or complete responses in other muscles.
During this stage, patient has mainly two type of synergy pattern. The first, the flexor synergy, includes the external rotation of the shoulder, flexion of the elbow, and supination of the forearm. The second, the extensor synergy, includes internal rotation of the shoulder with elbow extension and pronation of the forearm.
In this stage 30 and 40 percent of stroke survivors also experience spasticity. This is a velocity-dependent increase in your normal stretch reflexes, and during Stage 2, it presents as a resistance to passive movement. Stage 2 spasticity contributes to the jerky upper body movements characteristic of the flexor and extensor synergies.
Stage 3: Increased Spasticity
Spasticity in muscles, reaching its peak. Spasticity is a feeling of unusually stiff, tight, or pulled muscles. It is caused by damage from a stroke to nerve pathways within the brain or spinal cord that control muscle movement. Spasticity causes an abnormal increase in muscle stiffness and tone that can interfere with movement, speech, or cause discomfort and pain.
During stage 3, synergy patterns also start to emerge and minimal voluntary movements should be expected. The increase in voluntary movement is due to being able to initiate movement in the muscle, but not control it. The appearance of synergy patterns and coordination between muscles facilitate the voluntary movements which become stronger with physiotherapy.
Passive exercises, also known as passive range-of-motion exercises, should be continued during this stage to improve your range of motion. Patients and family/caregivers should be educated about the importance of maintaining range of motion and doing daily exercises.
Stage 4: Decreased Spasticity
During stage four, spastic muscle movement begins to decline. Patients will regain control mostly in the extremities, and they will have a limited ability to move normally. The movements may still be out of sync with muscle synergies. The focus during this stage is to strengthen and improve muscle control. Now that you are regaining motor control and can start to make normal, controlled movements on a limited basis.
Therapists use active-assisted range of motion (AAROM) exercises when a stroke patient has some ability to move. A therapist may help guide the movement with their own body or use bands and other exercise equipment to support the patient.
Stage 5: Complex Movement Combinations
In stage 5, spasticity continues to decline and synergy patterns within the muscles also become more coordinated, allowing voluntary movements to become more complex. The patient will be able to make more controlled and deliberate movements in the limbs that have been affected by the stroke. Isolated joint movements might also be possible.
Stage 6: Spasticity Disappears
At stage six, spasticity in muscle movement disappears completely. You are able to move individual joints, and synergy patterns become much more coordinated. Motor control is almost fully restored, and you can coordinate complex reaching movements in the affected extremities. Abnormal or spastic movements have ceased, and a full recovery may be on the horizon.
Stage 7: Normal Function Returns
The last stage in Brunnstrom’s Approach is when you regain full function in the areas affected by the stroke. You are now able to move your arms, legs, hands, and feet in a controlled and voluntary manner.
BENEFITS of the Brunnstrom approach :-
The Brunnstrom approach emphasises the ability to recover normal movement by facilitating reflexes, basic muscle synergies and sensory stimulation. This will help:
- Increase muscle strength
- Stretch tight muscles
- Regain motor control
- Recover voluntary movement
- Improve functional tasks such as sit to stand, walking, reaching, grasping and hand to mouth
- Improve the sequence of functional activities in order to achieve a specific aim
- Improve posture
- Increase independence
USES :-
specialised neurological physiotherapists use the Brunnstrom approach to rehabilitate patients with different neurological disorders. This approach is also used in conjunction with other types of treatment depending on the symptoms of the individual following injury.
The Brunnstrom approach is currently used to treat many neurological conditions including those with:
- Cerebral Palsy
- Head Injury
- Parkinson’s disease
- Stroke
- Spinal Cord Injury





One Comment